For years, doctors have told people with high blood pressure to aim for 120/80-the number that’s been stamped on posters in clinics, printed on app screens, and repeated in every health pamphlet. But lately, that number has become controversial. Is 120/80 the right goal for everyone? Or should your blood pressure target be personal-based on your age, health, and lifestyle? The answer isn’t simple, and the debate is heating up among doctors, researchers, and patients alike.
Why 120/80 Became the Gold Standard
The 120/80 mm Hg target didn’t come out of nowhere. It’s based on decades of research showing that keeping blood pressure below this level reduces the risk of heart attacks, strokes, and kidney damage. The 2017 American Heart Association and American College of Cardiology guidelines were a turning point. They reclassified blood pressure into four categories: normal (<120/<80), elevated (120-129/<80), stage 1 hypertension (130-139/80-89), and stage 2 hypertension (≥140/≥90). That shift meant millions more people were labeled as having high blood pressure-even if they felt fine. The push for lower targets came largely from the SPRINT trial, a major study published in 2015. It followed nearly 9,400 adults with high blood pressure and compared two goals: one group aimed for under 120 mm Hg systolic, the other under 140 mm Hg. The results were striking: those who hit the lower target had a 25% lower risk of major heart events and a 27% lower risk of dying from any cause. It sounded like a no-brainer. If lower is better, why settle for anything else?The Pushback: Why Some Doctors Say No
But here’s the catch: SPRINT didn’t include everyone. It excluded people with diabetes, history of stroke, or high fall risk-exactly the kinds of patients most primary care doctors see every day. That’s where the American Academy of Family Physicians (AAFP) stepped in. In their 2022 review, they found that pushing everyone to 120/80 didn’t save more lives overall-but it did cause more problems. For every 33 people treated to reach that lower target, one would experience a serious side effect: dizziness, fainting, kidney issues, or dangerously low blood pressure. They recommended sticking with 140/90 as the primary goal for most adults. Why? Because the extra benefit of going lower was tiny. For example, to prevent one heart attack, you’d need to treat 137 people for nearly four years. That’s a lot of pills, doctor visits, and anxiety for a small gain. In Australia, where I live, many GPs follow this more cautious approach. We see patients who are elderly, on multiple medications, or living alone. For them, a sudden drop in blood pressure can mean a fall, a broken hip, and months in rehab. That’s not progress-it’s harm.What the Latest Guidelines Say
By 2025, the divide had widened. The AHA/ACC doubled down, recommending a target under 130 mm Hg systolic for everyone with hypertension-and encouraging 120 mm Hg when it’s safe. Meanwhile, Japan’s 2025 guidelines went even further, saying <130/80 should be the universal target for all patients, no exceptions. They argue that every 5 mm Hg drop in systolic pressure cuts cardiovascular risk by about 10%, no matter your age. But Europe took a middle path. The European Society of Hypertension says: aim for 120-129/70-79 if you’re under 65, 130-139 if you’re 65-79, and up to 140-150 if you’re over 80. That’s not a one-size-fits-all rule-it’s a tailored approach. So who’s right? The truth is, they’re all looking at the same data and seeing different things. The AHA sees potential. The AAFP sees risk. Japan sees consistency. Europe sees nuance.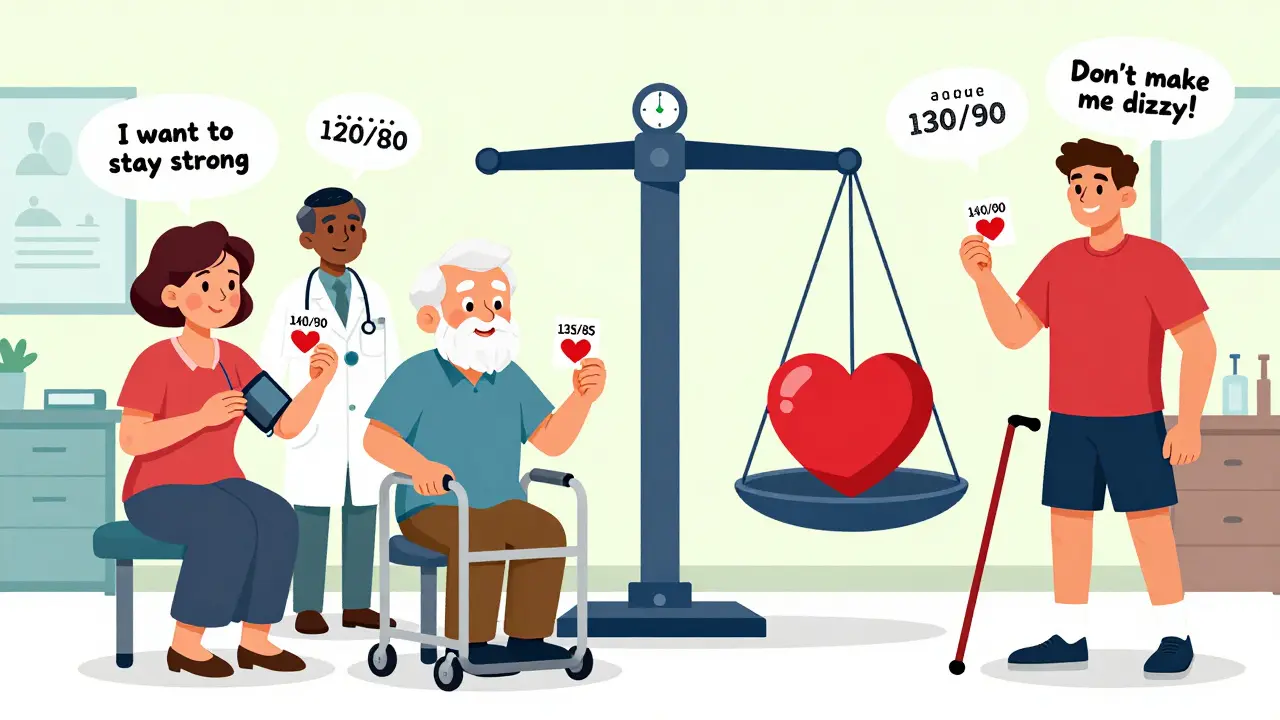
Who Should Aim for 120/80?
If you’re under 65, have diabetes, chronic kidney disease, or a 10-year cardiovascular risk above 7.5% (calculated using tools like the PREVENT score), then aiming for 120-130 mm Hg systolic makes sense. You’re in the group that benefited most in SPRINT. Your doctor may even start you on two medications right away to get you there faster. But if you’re older, frail, or taking five or more pills a day? Lowering your blood pressure too fast or too far can backfire. Studies show that in adults over 75, aggressive treatment increases the risk of falls, confusion, and hospitalization without clearly extending life. For them, 130-140 mm Hg might be the sweet spot. And what about people with stage 1 hypertension (130-139/80-89) and no other health problems? The AHA/ACC says try lifestyle changes first-cut salt, lose weight, move more, sleep better. Wait three to six months. Recheck. If your pressure hasn’t budged, then talk about meds. The AAFP agrees: don’t rush to pills.What About Side Effects?
Lower targets mean more drugs. More drugs mean more side effects. The most common? Dizziness, especially when standing up. Fatigue. Kidney function dips. High potassium levels. These aren’t just numbers on a lab report-they’re real symptoms that can make you feel awful or even land you in the ER. One study found that patients on intensive treatment needed one extra medication on average. That’s not just cost-it’s complexity. More pills mean more chances to forget, mix up, or stop taking them altogether. And if you’re already juggling meds for diabetes, arthritis, or depression, adding another one just to hit a number? It’s overwhelming. That’s why monitoring matters. If you’re going for 120/80, you need regular check-ins-not just blood pressure readings, but questions like: “Have you felt lightheaded lately?” “Do you get up at night to pee more?” “Any trouble walking or balancing?”The Real Goal: Your Health, Not Just a Number
Here’s what no guideline says out loud: Blood pressure is not a target to hit-it’s a tool to keep you alive and feeling well. If you’re 78, live alone, and your BP is 135/85, but you’re walking every day, eating well, sleeping soundly, and haven’t been to the hospital in five years-you’re doing better than someone who hits 118/76 but is dizzy, tired, and falling. The best treatment plan isn’t the one that gets you closest to 120/80. It’s the one that keeps you healthy, active, and independent. That’s why shared decision-making is no longer optional-it’s essential. Your doctor should say: “Here’s what the research says. Here’s what’s possible. Here’s what could go wrong. What matters most to you?” For some, it’s avoiding a stroke. For others, it’s staying off a walker. For some, it’s not taking another pill. Those aren’t trivial concerns-they’re life priorities.
What You Can Do Right Now
If you’re managing high blood pressure, here’s what to ask:- “Based on my age, health, and medications, what’s the right target for me?”
- “What are the risks of going lower? What are the risks of staying higher?”
- “If I feel dizzy or weak, should I lower my dose or stop the medication?”
- “Can we try lifestyle changes first before adding more pills?”
- “How often should I check my pressure at home, and what numbers should worry us?”
The Future: Personalized Blood Pressure Care
The next big shift won’t be another guideline. It’ll be personalization. Researchers are already testing AI tools that combine your genetics, kidney function, stress levels, sleep patterns, and even your social support network to predict how you’ll respond to different blood pressure treatments. The NIH just launched SPRINT-2-a new trial designed to test intensive treatment in real-world patients: older adults, people with diabetes, those at risk of falling. Results won’t come until 2028, but they might finally settle the debate. Until then, the best advice isn’t to chase 120/80. It’s to find your own balance. Your heart isn’t just a pump-it’s part of a life. And that life is worth more than a number on a screen.Is 120/80 the right blood pressure target for everyone?
No. While 120/80 is considered ideal for healthy adults, it’s not suitable for everyone. Older adults, those with multiple chronic conditions, or people at risk of falls may benefit more from a higher target like 130-140 mm Hg systolic. The goal is to reduce heart risks without causing harm from over-treatment. Your doctor should tailor the target based on your age, health, and lifestyle.
Why do some doctors recommend 140/90 instead of 120/80?
Doctors who recommend 140/90, like those following the American Academy of Family Physicians guidelines, point to evidence that lowering blood pressure below 130 mm Hg increases side effects-like dizziness, fainting, and kidney problems-without significantly reducing death rates in average patients. They argue that the small benefit doesn’t justify the extra medications, costs, and risks for many people, especially those over 65 or with complex health needs.
Can I lower my blood pressure without medication?
Yes, for many people, especially those with stage 1 hypertension (130-139/80-89) and no other health conditions, lifestyle changes can be enough. Cutting salt, losing weight, walking 30 minutes a day, limiting alcohol, managing stress, and eating more vegetables and whole grains can drop systolic pressure by 5-10 mm Hg. The AHA/ACC recommends trying these for 3-6 months before starting medication.
What are the signs my blood pressure is too low?
Symptoms of low blood pressure include dizziness or lightheadedness when standing, blurred vision, fatigue, nausea, confusion, cold or clammy skin, and fainting. If you’re on blood pressure medication and start feeling these symptoms, don’t ignore them. Talk to your doctor-your dose may need adjusting. Low pressure isn’t always better.
Should I buy a home blood pressure monitor?
Yes. Home monitoring gives a clearer picture than a single reading at the doctor’s office. Look for an upper-arm monitor that’s validated by organizations like the American Heart Association. Take readings at the same time each day, sit quietly for 5 minutes first, and keep a log. Share it with your doctor-it helps them see trends and adjust treatment safely.




Akshaya Gandra _ Student - EastCaryMS
so like... is 120/80 even real? my grandma’s 82 and her bp’s 140/85 and she still hikes every weekend. maybe the number’s just a myth made by people who’ve never met a real human.
Jacob Milano
Bro, I used to obsess over my numbers like they were SAT scores. Then I started walking 10k steps a day, sleeping like a baby, and eating actual food instead of ‘low-sodium’ cardboard. My bp dropped to 118/76 without meds. Maybe the goal isn’t the number-it’s the lifestyle behind it.
Jennifer Glass
It’s funny how we treat blood pressure like it’s a one-size-fits-all algorithm. We don’t expect everyone to have the same BMI or cholesterol, so why this? I’ve seen elderly patients on aggressive meds who feel dizzy all day just to hit 120/80. Sometimes the cure feels worse than the condition. Individualization isn’t just smart-it’s humane.
en Max
While the 120/80 mm Hg threshold has been widely disseminated as a clinical benchmark, recent meta-analyses-including the SPRINT trial-demonstrate a statistically significant reduction in cardiovascular events among high-risk populations; however, this benefit is not uniformly translatable across all age cohorts, particularly those over 75, where frailty, polypharmacy, and orthostatic hypotension introduce significant confounding variables. Thus, a risk-stratified, patient-centered approach is not merely advisable-it is ethically imperative.
Roshan Aryal
USA thinks it knows everything. In India, we treat hypertension with yoga, turmeric, and respect for elders-not pills and panic. Your 120/80 is a capitalist scam to sell more drugs. We live longer here without your numbers.
Chris Cantey
I used to think numbers meant control. Now I know they’re just mirrors. You stare at them long enough, you forget you’re the one breathing. The body doesn’t care about guidelines. It just wants to be left alone.
Angie Rehe
Stop romanticizing ‘individualized goals’-this is just doctors giving up. If we stop pushing 120/80, what’s next? ‘Oh, your cholesterol’s high? Just chill, bro.’ We need standards, not sentimentality. The data doesn’t lie.
Enrique González
My dad’s 70, has diabetes, and his BP’s 138/82. He’s got more energy than me. Stop treating people like lab rats. If you’re not dizzy, not fainting, and not in the ER-you’re doing fine.
saurabh singh
From India to the world: we’ve been doing this for centuries. Ayurveda says balance, not numbers. Eat light, walk slow, breathe deep. Your machine can’t measure peace. Maybe your BP drops when your mind stops screaming.
John Wilmerding
While the 2017 ACC/AHA guidelines established a target of <120/80 mm Hg for high-risk patients, subsequent subgroup analyses indicate that for individuals aged ≥75 years without diabetes or chronic kidney disease, a target of <140/90 mm Hg is associated with comparable cardiovascular outcomes and significantly reduced risk of adverse events. Clinical decision-making must integrate patient preferences, functional status, and comorbidity burden.
Peyton Feuer
my doctor just said ‘if you feel good, don’t stress the number.’ i used to check it 5x a day. now i just drink water, sleep, and walk. my bp’s 128/80 and i’m not dying. maybe that’s the real goal.
Terri Gladden
my sister got hospitalized because her bp dropped too low from meds trying to hit 120/80. she was in the hospital for a week. now they let her be at 140/85. she’s alive. that’s the only number that matters.
Aaron Mercado
It’s not about ‘personal goals’-it’s about accountability. If you let people off the hook because they ‘feel fine,’ then we’re just enabling denial. The heart doesn’t care how you feel-it only cares if you’re damaging it. 120/80 isn’t a suggestion. It’s a warning.
Abhishek Mondal
How dare you suggest that a Western medical standard-backed by decades of randomized controlled trials-should be replaced with anecdotal ‘feelings’ and ‘yoga’? Your ‘individualized’ approach is just pseudoscience dressed in cultural nostalgia. The data is clear: lower is better, period.