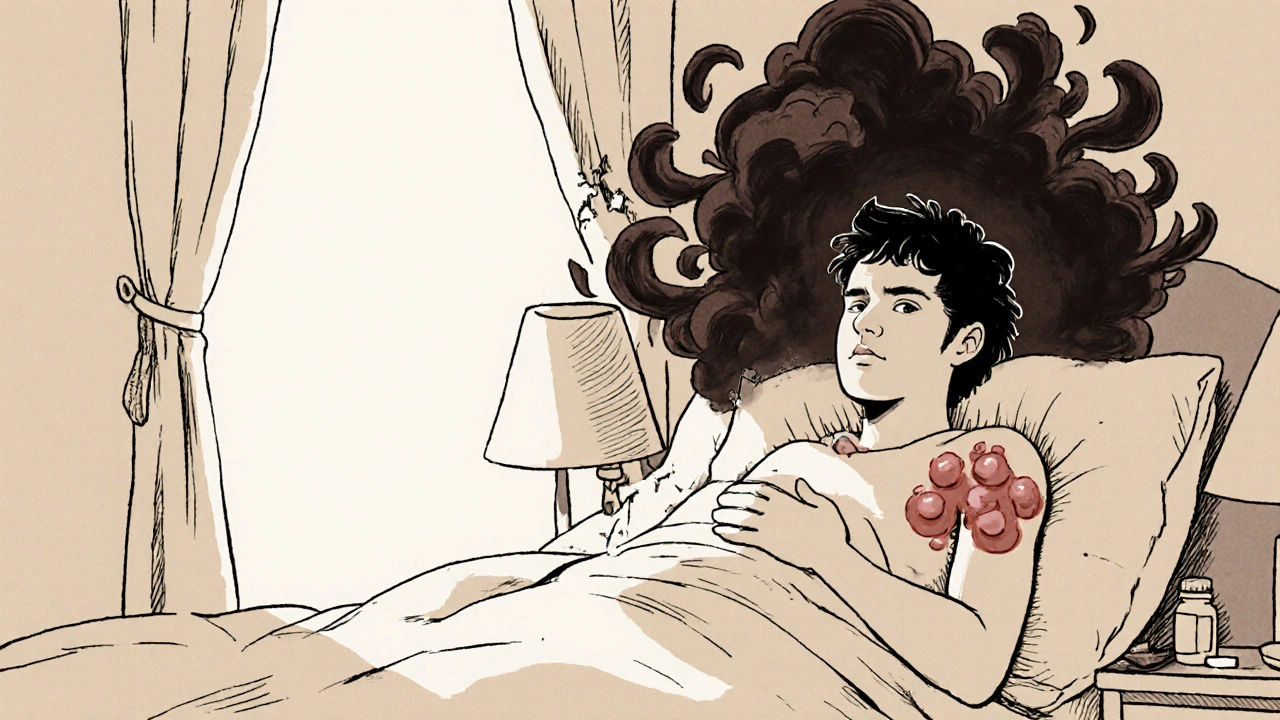
Imagine waking up every morning with deep, throbbing pain in your armpits or groin-not from an injury, not from infection you can see, but from something inside your skin that won’t go away. For more than 1 in 50 people, this is daily life with hidradenitis suppurativa (HS). It’s not acne. It’s not a boil. It’s a chronic, inflammatory condition that forms painful nodules, abscesses, and tunnels under the skin, often leaving scars and limiting movement, sleep, and social life. For decades, treatment meant antibiotics, hormonal pills, or surgery. But now, a new wave of targeted drugs called biologics is changing everything.
What Exactly Is Hidradenitis Suppurativa?
HS starts when hair follicles in areas with apocrine sweat glands-like the armpits, groin, under the breasts, and between the buttocks-become blocked. The blockage isn’t from dirt or oil. It’s caused by abnormal skin cell growth and thickening, trapping bacteria and triggering a fierce immune response. The body doesn’t just fight the bacteria; it attacks the surrounding tissue, creating deep, painful lumps that turn into abscesses, drain pus, and form tunnels (sinus tracts) under the skin.
It’s not contagious. It’s not caused by poor hygiene. And it’s not rare. Around 1% to 4% of people worldwide have it, with women affected three times more often than men. Most people first notice symptoms between ages 20 and 29. Many live with it for years before getting a correct diagnosis-some wait over a decade. That’s because doctors often mistake it for recurrent boils or ingrown hairs.
The pain is constant. Not just when the lumps are swollen, but often in the background. People describe it as a deep, burning ache that makes sitting, walking, or even wearing tight clothes unbearable. The emotional toll is just as heavy. Many avoid intimacy, skip the gym, or stop going out altogether because of the odor, drainage, and visible scarring.
Why Traditional Treatments Often Fall Short
For years, the go-to treatments were antibiotics like clindamycin or doxycycline, hormonal therapies like birth control pills or spironolactone, and surgical drainage or removal of affected tissue. These can help in mild cases, but they rarely stop the disease from progressing.
Antibiotics reduce inflammation temporarily but don’t change the underlying immune overreaction. Hormonal treatments help some women, especially those whose HS flares with their cycle, but they don’t work for everyone. Surgery removes visible lesions, but if the disease is still active underneath, new nodules form nearby. Many patients end up with multiple surgeries, scarring, and no real long-term relief.
The real problem? These treatments don’t target the root cause: the runaway inflammation. HS isn’t just a skin problem-it’s a systemic immune disorder. That’s why biologics, which were first developed for conditions like psoriasis and rheumatoid arthritis, became such a game-changer.
How Biologic Therapy Works
Biologics are made from living cells and designed to block specific parts of the immune system that drive inflammation. Unlike antibiotics or steroids that suppress the whole immune system, biologics are like precision missiles-they hit only the targets causing the damage.
In HS, three key inflammatory molecules are overactive: TNF-alpha, IL-17A, and IL-17F. These cytokines act like alarm bells, telling immune cells to attack healthy tissue. Biologics silence those alarms.
There are now three FDA-approved biologics for HS:
- Adalimumab (Humira): Blocks TNF-alpha. First approved in 2015. Given as a weekly or every-other-week injection. About 42% of patients see at least half their lesions improve within 12 weeks.
- Secukinumab (Cosentyx): Blocks IL-17A. Approved in early 2024. Given as monthly injections after an initial weekly dose. In trials, 45% of patients achieved major improvement at 16 weeks.
- Bimekizumab (BIMZELX): Blocks both IL-17A and IL-17F. Approved in mid-2024. This dual-action approach is the most potent so far, with 67% of patients seeing 50% or more lesion reduction at 16 weeks.
These aren’t just numbers. Real patients report life-changing results. One woman from Perth, who’d been on antibiotics for six years with no relief, started secukinumab and saw her abscesses disappear within five weeks. Another man with HS since his teens said he slept through the night for the first time in 15 years after starting bimekizumab.

Comparing the Biologics: Efficacy, Cost, and Side Effects
Not all biologics are the same. Here’s how they stack up:
| Biologic | Target | HiSCR50 at 12-16 Weeks | Dosing Schedule | Monthly Cost (US) | Common Side Effects |
|---|---|---|---|---|---|
| Adalimumab (Humira) | TNF-alpha | 41.8% | 40 mg weekly or every other week | $5,800 | Injection site reactions, upper respiratory infections |
| Secukinumab (Cosentyx) | IL-17A | 44.5% | 300 mg monthly after 5 weekly doses | $6,200 | Headache, fungal infections, diarrhea |
| Bimekizumab (BIMZELX) | IL-17A and IL-17F | 66.9% | 320 mg monthly after 640 mg loading dose | $6,900 | Candida infections, fatigue, mild nausea |
Bimekizumab shows the strongest results, especially for people with lots of inflamed nodules. But adalimumab still has a place-especially for those with advanced scarring and sinus tracts. Secukinumab strikes a balance between effectiveness and tolerability.
Cost is a huge barrier. In the U.S., monthly prices range from $5,800 to $6,900. Even with insurance, many patients pay $800-$1,200 out of pocket. Medicaid patients face approval rates as low as 45%, while those with private insurance get approved about 80% of the time. In Australia, PBS subsidies are limited, and access varies by state. Many patients rely on patient assistance programs from drugmakers to afford treatment.
Who Benefits Most-and Who Doesn’t
Biologics work best for people with Hurley Stage II or III HS:
- Stage II: Multiple abscesses and sinus tracts, but not fully connected.
- Stage III: Widespread, interconnected tunnels and abscesses, often with heavy scarring.
They’re less effective in Stage III patients with heavy, long-standing scarring. That’s because biologics reduce inflammation, but they can’t undo scar tissue. That’s why experts stress: start early.
People with other autoimmune conditions-like psoriasis or Crohn’s disease-often respond better to biologics because their immune systems are already primed to react to these drugs.
But not everyone is a candidate. You can’t start biologics if you have:
- Active tuberculosis
- Chronic hepatitis B or C
- Uncontrolled heart failure
- A recent serious infection
Before starting, you’ll need blood tests, a TB skin test, and a review of your medical history. Your doctor will also check your vaccination status-you need to be up to date on shingles, pneumonia, and flu shots.
What Happens After You Start?
Most people see some improvement within 4 to 8 weeks. But it takes 12 to 16 weeks to know if the drug is working well enough. Doctors use the IHS4 score-a tool that counts abscesses, nodules, and draining tunnels-to track progress.
If you’re not improving by week 12, your doctor may switch you to another biologic. About 30% of people who don’t respond to adalimumab do respond to secukinumab or bimekizumab.
Side effects are usually mild: redness or itching at the injection site, headaches, or minor colds. But because biologics suppress part of the immune system, you’re at higher risk for serious infections like pneumonia or tuberculosis. That’s why regular check-ins with your dermatologist are critical.
Interestingly, many patients see improvements in their cholesterol levels too. Triglycerides drop, HDL (the good cholesterol) rises. This suggests biologics aren’t just helping the skin-they may be reducing long-term heart disease risk, which is higher in HS patients.
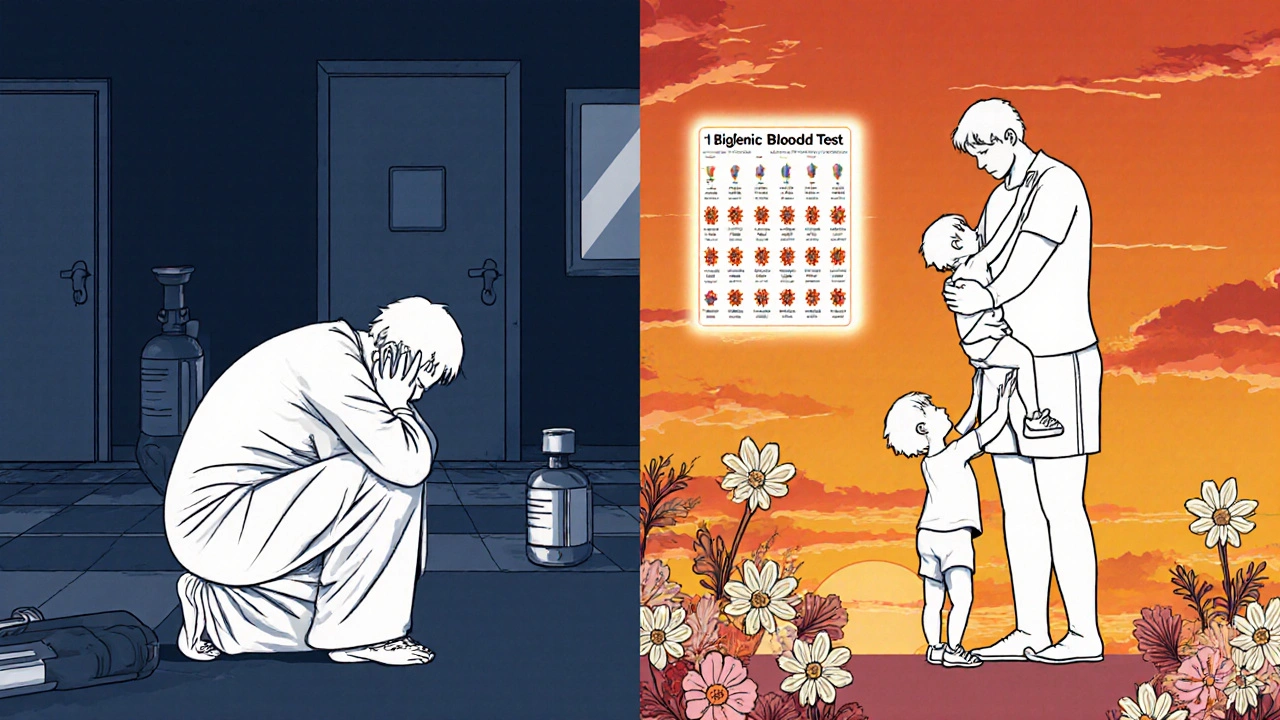
Real Stories, Real Challenges
On patient forums like MyHSteam and Reddit, people share what really happens:
- “After 10 years of pain, adalimumab gave me back my life. But I had to quit my job to manage the injections and doctor visits.”
- “I started bimekizumab and saw my abscesses vanish in 6 weeks. Then I got a yeast infection and had to pause treatment.”
- “I can’t afford it without insurance. I’m on a waiting list for a patient assistance program.”
- “I stopped because the cost was too high. Now I’m back to antibiotics and painkillers.”
Many say the biggest win isn’t just fewer lumps-it’s being able to wear shorts again, hug their kids without fear, or sleep through the night.
But the emotional burden doesn’t vanish overnight. Some feel guilt for not being “grateful enough” for treatment. Others feel isolated when friends don’t understand why they can’t just “take a pill.”
What’s Next? The Future of HS Treatment
The field is moving fast. Three new biologics are in late-stage trials:
- Guselkumab: Targets IL-23. Early results show 58% response rate.
- Spesolimab: Blocks IL-36. Shows promise for patients who didn’t respond to IL-17 inhibitors.
- TAK-279: A new oral drug that blocks TYK2, a key immune signaling molecule.
Some researchers are even exploring combination therapy-using biologics alongside minor surgical procedures to remove stubborn tunnels. One study showed 89% of patients responded when biologics were paired with surgical cleaning, compared to 67% with biologics alone.
And there’s hope for personalized treatment. A 2024 study identified a 12-gene signature that can predict who will respond to adalimumab with 85% accuracy. That means in the future, you might get a blood test before starting treatment to know which drug will work best for you.
By 2030, experts predict 70% of moderate-to-severe HS patients will be on biologics. Right now, it’s about 28%. The gap is closing-but only if access improves.
What You Can Do Now
If you think you have HS:
- See a dermatologist who knows HS. Don’t settle for a general practitioner who calls it “recurrent boils.”
- Ask about your Hurley stage. That determines your treatment options.
- Start biologics early. The sooner you treat the inflammation, the less scarring you’ll get.
- Stop smoking. Smoking makes HS worse and reduces biologic effectiveness.
- Manage your weight. Even a 10% weight loss can reduce flare-ups.
- Join a support group. You’re not alone. Communities like the HS Foundation and MyHSteam offer real advice and emotional support.
HS is not your fault. It’s not something you caught. It’s a complex immune condition that’s finally being understood-and treated-in ways that work.
Biologics aren’t a cure. But for the first time, they offer real control. They turn a life of pain and isolation into one of manageable symptoms and restored dignity.
Can biologic therapy cure hidradenitis suppurativa?
No, biologics don’t cure HS. But they can put it into long-term remission. Many patients stay in remission for years as long as they keep taking the medication. Stopping treatment often leads to a return of symptoms.
How long does it take for biologics to work?
Most people notice improvement within 4 to 8 weeks. But full results take 12 to 16 weeks. Doctors usually wait until week 12 to decide if the treatment is working well enough. If there’s no improvement by then, switching to another biologic is common.
Are biologics safe for long-term use?
Yes, for most people. Biologics have been used safely for over 20 years in conditions like psoriasis and rheumatoid arthritis. The biggest risk is serious infections, which is why screening and monitoring are essential. Regular blood tests and check-ups help catch problems early.
Can I use biologics if I’m pregnant?
Some biologics, like adalimumab and secukinumab, are considered low-risk during pregnancy, but decisions must be made with your doctor. Many women with HS choose to continue treatment during pregnancy because uncontrolled HS can be more harmful than the medication. Always consult your dermatologist and OB-GYN before making changes.
Why do some people stop biologic therapy?
Cost is the top reason-many patients can’t afford the out-of-pocket expenses. Others stop due to side effects like infections, or because they don’t see enough improvement. Some feel discouraged after initial setbacks. But switching to another biologic often works. Never stop without talking to your doctor first.
Do I still need to see a surgeon if I’m on biologics?
Maybe. Biologics treat inflammation, but they don’t remove existing scar tissue or deep sinus tracts. If you have tunnels that drain constantly or cause pain, your doctor may recommend minor surgery to clean them out. Many now combine biologics with surgical debridement for the best results.
Can lifestyle changes help with HS even if I’m on biologics?
Absolutely. Stopping smoking can improve biologic effectiveness by up to 50%. Losing even 10% of your body weight reduces flare-ups. Wearing loose, breathable clothing and avoiding deodorants with aluminum can also help. Biologics work best when paired with smart daily habits.


Conor McNamara
they say biologics are the answer but i bet the pharmas are hiding something... why do they want us injecting stuff into our armpits? i think this is all about control. they dont want us healthy they want us dependent. check the patents. check the funding. something smells fishy.
steffi walsh
i just started secukinumab last month and OMG it’s like a miracle 🙏 i used to cry every night from the pain now i can wear shorts again and hug my niece without fear. you’re not alone ❤️
Leilani O'Neill
Honestly, if you're going to spend $7k a month on a drug, you should at least be Irish or have a PhD. This isn't some charity for people who can't afford to stop smoking or lose weight. It's a luxury treatment for the privileged.
Riohlo (Or Rio) Marie
Let’s be real - this isn’t medicine, it’s performative healthcare. Biologics are the new Tesla of dermatology. Everyone’s posting about their ‘journey’ like it’s a TED Talk. Meanwhile, the real sufferers are stuck in Medicaid limbo, GoFundMe-ing their way to a 300mg injection. The system doesn’t care if you can walk - it cares if you can pay.
Emanuel Jalba
I CAN’T BELIEVE PEOPLE ARE STILL USING ANTIBIOTICS 😭 I MEAN REALLY?? WHY ARE YOU LETTING YOURSELF BECOME A HUMAN PUS FACTORY WHEN THERE’S A $6900 SOLUTION?? YOU’RE NOT TRYING HARD ENOUGH. THIS ISN’T A CHOICE - IT’S A MORAL OBLIGATION TO YOURSELF.
Heidi R
You all act like this is a miracle. But what about the yeast infections? The fatigue? The fact that you’re now a walking immunosuppressed target? You think this is healing? It’s just swapping one prison for another.
Kristina Williams
they said vaccines were dangerous too now they want us to inject biologics? what next? nanobots in our sweat? i heard the government is putting tracking chips in the needles. you think your insurance is helping you? they just want you to live longer so you pay more taxes.
Christine Eslinger
I’ve been living with HS for 17 years. I tried everything - antibiotics, lasers, even a weird herbal tea someone on Facebook swore by. When I started adalimumab, I didn’t believe it either. But after 10 weeks, I slept through the night for the first time since college. It’s not magic. It’s science. And yes, it’s expensive. But if you’re reading this and still in pain - please, talk to your derm. You deserve relief.
Denny Sucipto
man i used to think i was broken. every time i looked in the mirror i saw failure. then i found this community. then i got on bimekizumab. now i can go to the beach with my kids. i don’t cry anymore when i change my shirt. it’s not perfect but it’s enough. you’re not alone. i see you.
Holly Powell
The Hurley staging criteria are outdated. The IHS4 score lacks sensitivity for subcutaneous sinus tract resolution. Current biologic trials overrepresent Stage II patients and underreport long-term fungal comorbidities. Without stratified biomarker analysis, we’re essentially engaging in empirical immunomodulation with high economic externalities.
Sarah Frey
Thank you for writing this with such care. I’ve been waiting years for someone to explain this without sugarcoating or sensationalizing. I’m not cured. But I’m no longer hiding. That matters.
Katelyn Sykes
i got the bimekizumab shot last week and my armpit stopped oozing like a volcano 🤯 i still have scars but i can breathe now and that’s enough for today
Gabe Solack
Just wanted to say - if you’re on a waiting list for patient assistance, don’t give up. I was in the same spot. Took me 8 months, but I got through. You’re not a burden. You’re a warrior. Keep going 💪
Yash Nair
in india we dont have these drugs at all so why are you all talking like its normal? we have to use turmeric paste and pray. america is so rich they think medicine is a shopping cart. we are not lazy we are just poor. stop judging people who cant afford your miracle drugs