UC Inflammation Severity Calculator
Biomarker Input
Enter your recent test results to assess inflammation severity.
Severity Assessment
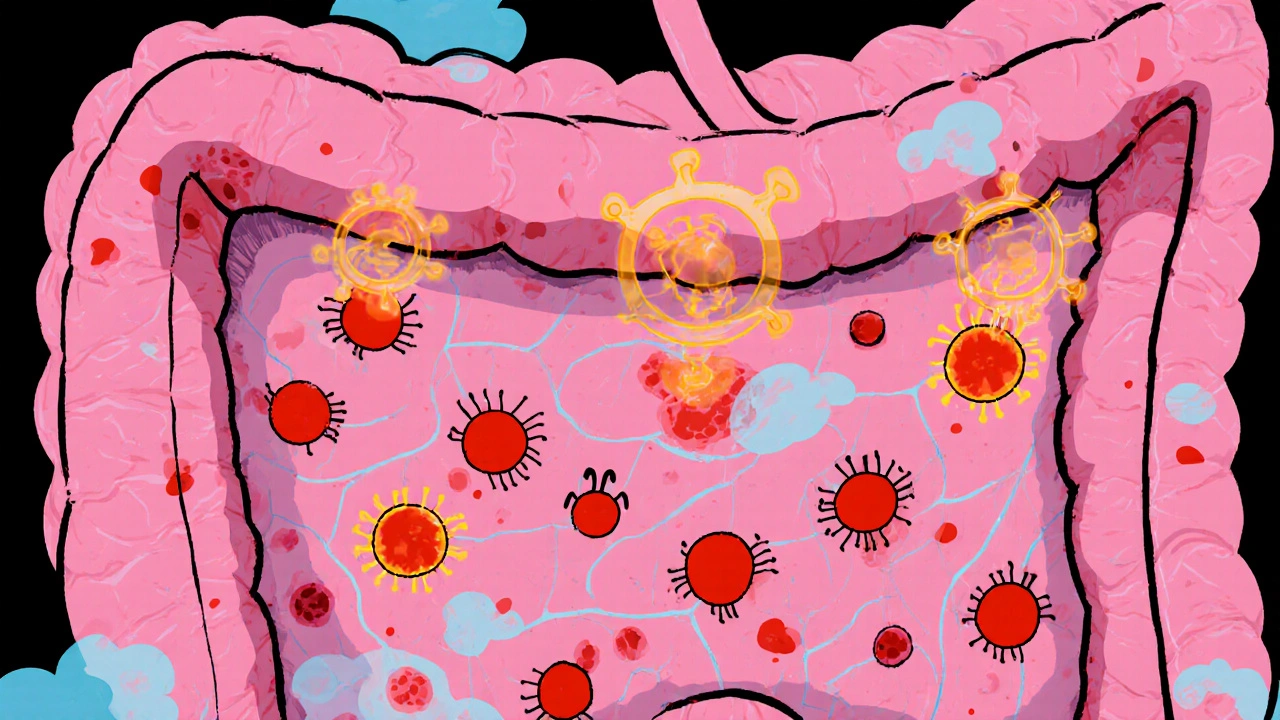
Ulcerative colitis is a chronic inflammatory bowel disease that causes ulcers and bleeding in the colon's inner lining. It belongs to the broader group of inflammation‑related disorders, where the immune system mistakenly attacks gut tissue.
What Is Ulcerative Colitis?
Ulcerative colitis (UC) affects only the large intestine, starting at the rectum and potentially extending to the entire colon. Unlike Crohn’s disease, which can involve any part of the gastrointestinal tract, UC’s lesions are continuous and confined to the mucosal layer.
Typical symptoms include abdominal cramping, frequent watery stools, urgency, and blood or mucus in the stool. About 900,000 people in the United States live with UC, and prevalence is rising in Australia, especially among younger adults.
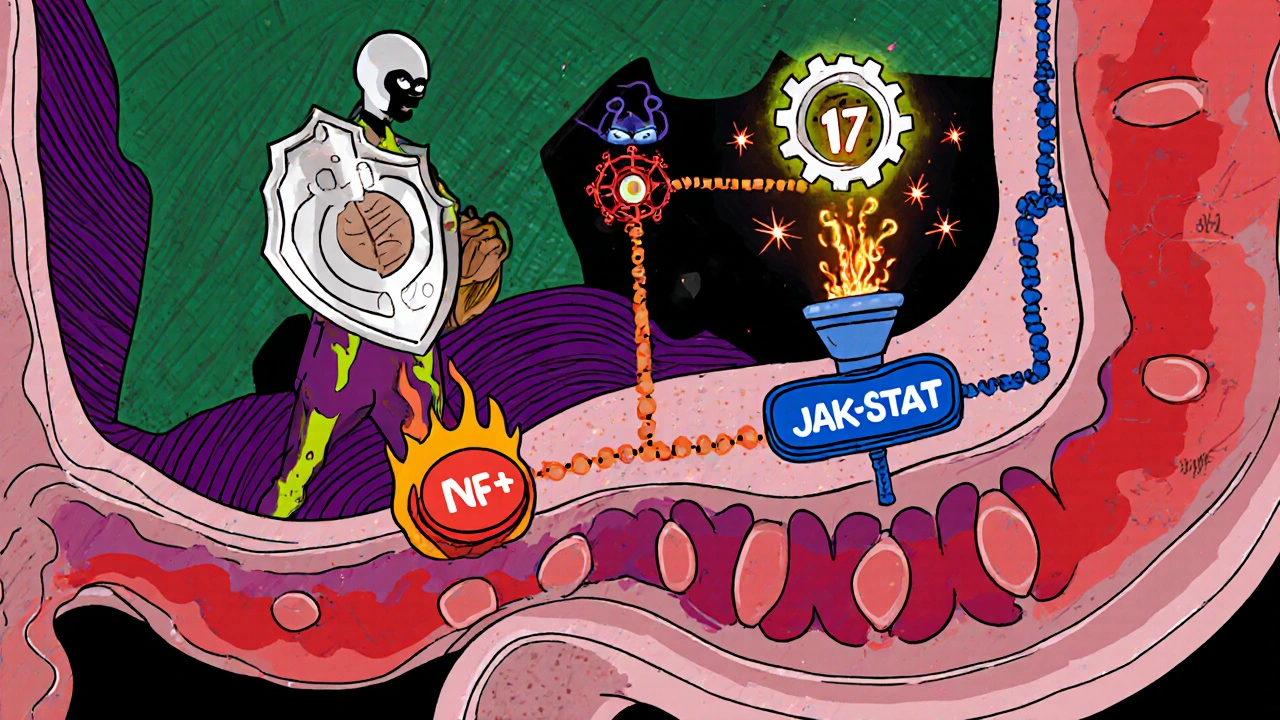
How Inflammation Drives the Disease
The core problem in UC is a dysregulated immune response. When the gut lining is breached, immune cells release a cocktail of cytokines that amplify the attack. Two cytokines dominate the picture: TNF‑alpha and interleukin‑6 (IL‑6). Both act as messengers that summon more immune cells, increase vascular permeability, and damage the epithelial barrier.
When this cycle persists, the colon’s protective mucus thins, ulcers form, and bleeding starts. Researchers estimate that high levels of TNF‑alpha correlate with a 2.3‑fold increase in flare severity.
Key Inflammatory Pathways in UC
- NF‑κB pathway: Activated by bacterial components, it turns on genes that produce TNF‑alpha, IL‑6, and other pro‑inflammatory mediators.
- JAK‑STAT signaling: Critical for transmitting signals from cytokines like IL‑6 into the cell nucleus, leading to more immune cell recruitment.
- Th17 cell axis: Th17 cells release IL‑17, which further weakens the mucosal barrier and promotes chronic inflammation.
Understanding these pathways helps clinicians choose targeted therapies that interrupt the cascade rather than merely suppressing symptoms.
Diagnosing Inflammation: What the Tests Show
Accurate assessment starts with a colonoscopy. During the procedure, doctors look for the classic “continuous erythema with ulceration” pattern and take biopsies for histology.
Lab tests add quantitative data:
| Marker | What It Indicates | Typical Range (Healthy) |
|---|---|---|
| C‑reactive protein (CRP) | Systemic inflammation | <5 mg/L |
| Fecal calprotectin | Intestinal neutrophil activity | <50 µg/g |
| Erythrocyte sedimentation rate (ESR) | Chronic inflammation | 0‑20 mm/hr |
| Serum cytokines (TNF‑α, IL‑6) | Specific immune activation | Variable, often elevated in flares |
Elevated fecal calprotectin is especially useful because it rises before symptoms worsen, allowing early intervention.
Managing Inflammation: From First‑Line to Advanced Therapies
Therapeutic goals are simple: induce remission, maintain it, and minimize steroid exposure.
| Drug Class | Mechanism | Onset of Action | Typical Use | Major Side Effects |
|---|---|---|---|---|
| 5‑ASA (mesalamine) | Topical anti‑inflammatory | Weeks | Mild‑to‑moderate UC | Nausea, headache |
| Corticosteroids | Broad immune suppression | Days | Acute flares | Weight gain, osteoporosis |
| Biologics (anti‑TNF) | Neutralize TNF‑alpha | Weeks | Moderate‑to‑severe UC | Infection risk, injection reactions |
| JAK inhibitors | Block JAK‑STAT signaling | Weeks | Refractory disease | Thromboembolism, lipid changes |
| Vedolizumab (integrin blocker) | Prevent immune cells from entering gut | Weeks | Patients not responding to anti‑TNF | Joint pain, nasopharyngitis |
While 5‑ASA is the first line for many, about 30 % of patients eventually need biologics or JAK inhibitors to keep inflammation under control.
In addition to drugs, lifestyle tweaks matter. A low‑FODMAP diet, regular moderate exercise, and stress‑reduction techniques (like mindfulness) can lower CRP by up to 15 % in some studies.
Emerging Therapies Targeting the Gut Microbiome
The gut microbiome is a hot research area. Dysbiosis-a shift toward harmful bacteria-feeds the inflammatory loop. Probiotics, fecal microbiota transplantation (FMT), and next‑generation microbial consortia are being tested in Phase II trials.
Preliminary data show that FMT can achieve clinical remission in roughly 30 % of patients with refractory UC, comparable to some biologics, but the long‑term safety profile is still unclear.
Quick Checklist for Controlling UC‑Related Inflammation
- Schedule a colonoscopy at diagnosis and then every 1‑3 years based on disease extent.
- Track fecal calprotectin monthly during remission; act if it rises above 150 µg/g.
- Start 5‑ASA early; add a short‑course steroid only for documented flares.
- Consider anti‑TNF or JAK inhibitor if steroids become needed more than twice a year.
- Incorporate a personalized diet plan-low‑FODMAP, adequate fiber, limited processed foods.
- Maintain regular exercise (150 min/week) and stress‑management practice.
- Discuss microbiome‑based therapies with a gastroenterologist when conventional meds fail.
Frequently Asked Questions
Can inflammation be completely cured in ulcerative colitis?
UC is a chronic condition, so the goal is remission-not a permanent cure. Effective anti‑inflammatory therapy can keep the gut quiet for years, but occasional flares are common.
What is the best blood test to monitor inflammation?
C‑reactive protein (CRP) is quick and inexpensive, but fecal calprotectin is more specific for intestinal inflammation and predicts relapses earlier.
Are biologics safe for long‑term use?
Long‑term data show a modest increase in infection risk, especially respiratory and skin infections. Regular screening and vaccinations mitigate most concerns.
How does stress affect UC inflammation?
Stress spikes cortisol, which can dysregulate gut barrier function and heighten cytokine release. Mind‑body practices have reduced flare frequency in several small trials.
Is FMT a viable option for everyone with UC?
Not yet. Current guidelines reserve FMT for patients who have failed standard biologics and steroids, and it should be performed in a specialized center.
Understanding how inflammation fuels ulcerative colitis gives you clear targets-both drug‑based and lifestyle-to keep the disease under control. By monitoring biomarkers, using the right medication ladder, and staying alert to new microbiome therapies, many people achieve long periods of remission and a better quality of life.
If you or a loved one is navigating UC, discuss the inflammation markers and treatment options outlined here with a gastroenterologist. Early, personalized action is the most powerful tool against chronic gut inflammation.



Mike Peuerböck
Understanding the inflammatory pathways in ulcerative colitis can be empowering for patients and clinicians alike. When the NF‑κB cascade lights up, it drives the production of cytokines that ravage the gut lining. Similarly, the JAK‑STAT route translates IL‑6 signals into relentless immune cell recruitment. These mechanisms underline why targeting them with biologics or small molecules yields remission. A patient who starts mesalamine early often avoids the need for steroids. If disease activity spikes, a short course of prednisone can tame the flare. However, repeated steroid bursts increase bone loss and weight gain. That is why clinicians consider anti‑TNF agents once steroids become frequent. Agents such as infliximab neutralize TNF‑α and restore mucosal healing. For those who cannot tolerate anti‑TNF, JAK inhibitors block downstream signaling. Emerging microbiome therapies aim to reset the bacterial ecosystem that fuels inflammation. Fecal calprotectin monitoring can warn of an impending flare before symptoms appear. Patients should track this marker monthly during remission. Lifestyle adjustments like low‑FODMAP diet and regular exercise shave CRP levels. Stress reduction through mindfulness can further dampen cytokine release. Together, these strategies provide a comprehensive arsenal against ulcerative colitis.
Simon Waters
The pharma giants profit from every new biologic they push onto the market. They hide the long‑term risks while advertising miracle cures. Trusting only the data released by independent labs is the safer route.
Celeste Flynn
Fecal calprotectin is a non‑invasive marker that rises before clinical symptoms. Regular testing can catch subclinical inflammation early. Combining this with colonoscopy findings creates a robust assessment. Patients should discuss testing intervals with their gastroenterologist. Early intervention often reduces the need for aggressive biologics.
CASEY PERRY
Targeted inhibition of JAK1/3 attenuates STAT phosphorylation, curtailing IL‑6 mediated transcription. Pharmacokinetic profiles of tofacitinib show rapid absorption and hepatic metabolism via CYP3A4. Dose titration based on trough concentrations optimizes efficacy while minimizing thrombosis risk. Current trials evaluate selective TYK2 inhibitors as next‑generation agents.
Jennell Vandermolen
You're doing great by staying informed about your condition. Keep tracking your biomarkers and share the trends with your doctor. Small lifestyle tweaks can make a big difference over time. Remember that remission is achievable with consistent effort.
Vikas Kumar
India's ancient herbs outperform those synthetic pills you trust.
Shan Reddy
Totally agree that stress management helps keep the gut calm. I try a quick breathing exercise whenever I feel a rumble. It’s amazing how a few minutes can lower my CRP reading.
Naomi Shimberg
While anecdotal breathing techniques are popular, they lack rigorous randomized control data. Reliance on such methods may delay initiation of proven pharmacotherapy. A disciplined adherence to evidence‑based regimens remains paramount.
kenny lastimosa
Inflammation is the body's language of distress, reminding us that health is a negotiated balance. When we silence that message with drugs, we must ask what silence costs. Perhaps the true cure lies not in suppression but in understanding the underlying disharmony.