Lithium-NSAID Interaction Risk Calculator
This tool estimates the risk of lithium toxicity when taking NSAIDs based on medical evidence. Lithium is cleared by kidneys, and NSAIDs reduce kidney function, causing lithium to build up. Even short-term NSAID use can be dangerous.
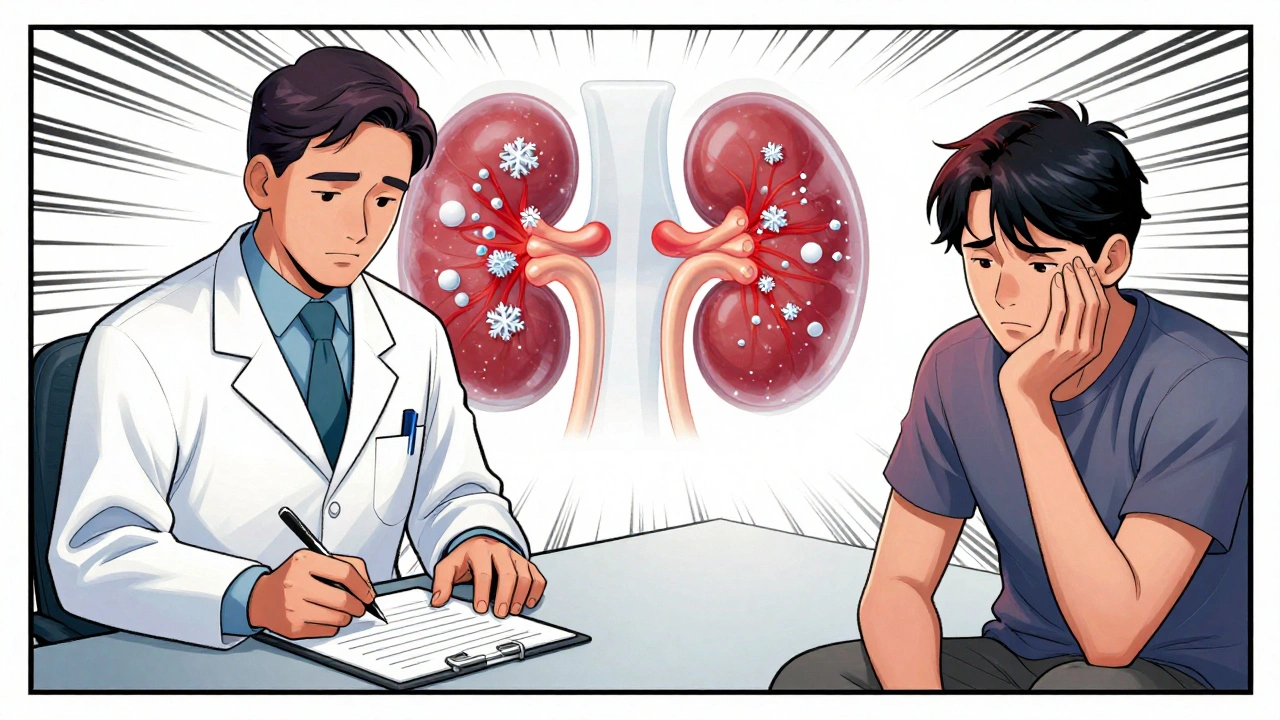
When you're taking lithium for bipolar disorder, even a common painkiller like ibuprofen can turn dangerous - and many people don’t realize it until it’s too late. Lithium has been a cornerstone treatment for decades, helping millions stabilize their moods. But when it’s paired with NSAIDs - the go-to meds for headaches, arthritis, or back pain - the risk of serious kidney damage and life-threatening toxicity skyrockets. This isn’t a rare edge case. It’s a predictable, preventable crisis happening in clinics and homes every day.
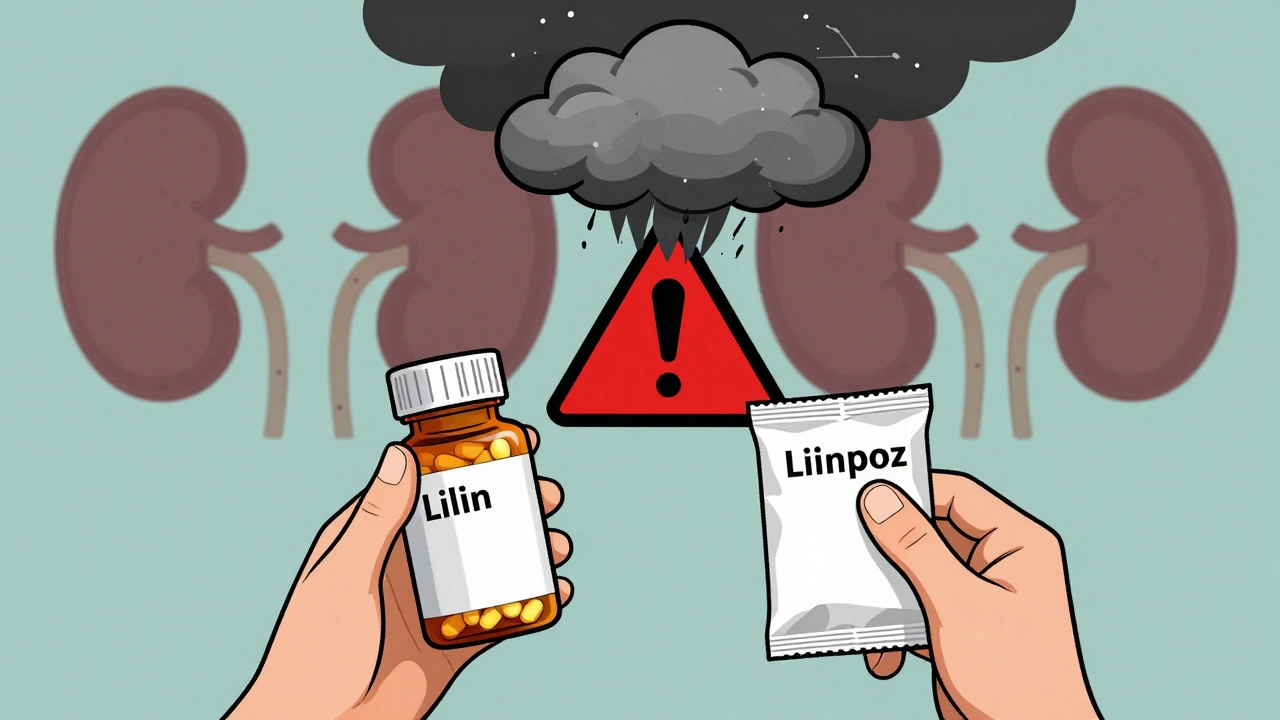
Why Lithium and NSAIDs Don’t Mix
Lithium works by balancing brain chemicals, but it’s cleared from your body almost entirely by your kidneys. That’s where NSAIDs step in and cause trouble. These drugs - including ibuprofen, naproxen, and indomethacin - block enzymes called COX-1 and COX-2. Those enzymes help your kidneys produce prostaglandins, which keep blood flowing smoothly through kidney filters. When NSAIDs shut that down, your kidneys slow down. And when kidney function drops, lithium doesn’t get flushed out. It builds up.Studies show that just a few days of NSAID use can reduce lithium clearance by 25% to 60%. That means your lithium levels could jump from a safe 0.6 mmol/L to a toxic 1.8 mmol/L or higher - all because you took an Advil for a bad back. The higher the dose of the NSAID, the worse the spike. Indomethacin is the worst offender, often pushing lithium levels up by 40-60%. Even celecoxib, sometimes called a "kidney-safe" NSAID, still increases lithium by 10-15% in people with existing kidney issues.
The Kidney Takes the Brunt
This isn’t just about lithium levels. It’s about your kidneys getting hit from two sides. Lithium itself slowly damages kidney cells over time by disrupting their internal signaling. NSAIDs make it worse by cutting off blood flow. Together, they create a perfect storm for acute kidney injury (AKI). A 2023 JAMA Network Open study found that people taking both drugs had over three times the risk of AKI compared to those on lithium alone. And the biggest spike? Within the first 30 days of starting the NSAID.For older adults - especially those over 65 - this is even more dangerous. Kidney function naturally declines with age. Add lithium and an NSAID, and you’re looking at a 52% higher chance of hospitalization for kidney failure. In one study of 478 nephrology clinics, nearly 4 out of 10 lithium-related kidney emergencies were directly tied to NSAID use. And in many cases, the patient had no idea the two drugs were risky together.
How Bad Is It Compared to Other Painkillers?
Not all pain meds are created equal when you’re on lithium. Acetaminophen (Tylenol) is the safest bet. It doesn’t affect kidney blood flow or lithium clearance. Studies show no meaningful rise in lithium levels - even at the maximum daily dose of 3,000 mg. Opioids like tramadol can cause a small increase (10-15%), mostly because they cause dehydration, but they’re still far less risky than NSAIDs.Compare that to NSAIDs: they’re responsible for a 2.8-fold increase in long-term kidney function decline. A 2022 study tracking over 12,000 patients found that those on lithium and NSAIDs lost kidney function at nearly triple the rate of those using acetaminophen. Even worse, many doctors still prescribe NSAIDs without realizing the danger. A 2023 survey showed only 58% of primary care providers knew NSAIDs were high-risk for lithium users. That means patients are often getting these prescriptions from dentists, orthopedists, or ER doctors who aren’t familiar with psychiatric meds.
Real Stories, Real Consequences
Reddit threads from r/psychiatry tell the same story over and over. One user wrote: "Took ibuprofen for a sprained ankle. Three days later, I couldn’t hold a spoon. Tremors, dizziness, blurred vision. ER said my lithium was 2.1. I spent a week in the hospital." Another said: "My psychiatrist warned me. My orthopedist didn’t. I ended up with permanent kidney damage. My eGFR dropped 45%."Case studies back this up. In one 2022 report, 17 patients were hospitalized for lithium toxicity. Fourteen of them had taken NSAIDs. Six developed permanent kidney damage. That’s not a fluke. It’s a pattern. And the cost? In the U.S. alone, lithium-NSAID related hospitalizations cost $48.7 million a year. Each episode averages over $18,000. Most of it preventable.
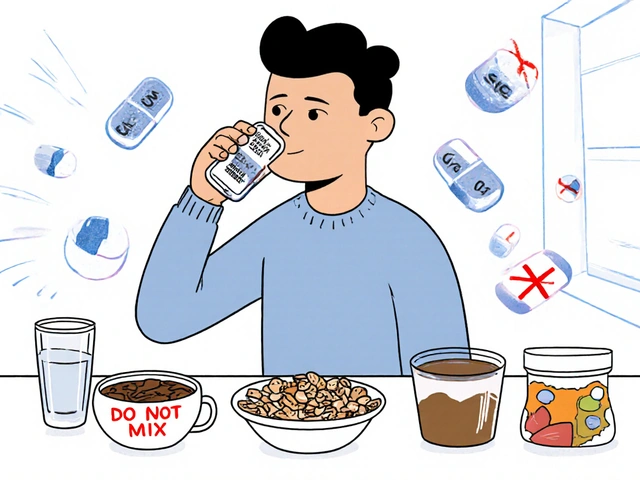
What Should You Do Instead?
If you’re on lithium and need pain relief, here’s what works:- Start with acetaminophen. Up to 3,000 mg per day is generally safe. Don’t exceed it - liver damage is a risk at higher doses.
- If that’s not enough, try tramadol. It’s a weak opioid. Start low (25 mg daily) and increase slowly. Watch for dizziness or constipation.
- Only use NSAIDs if absolutely necessary - and never for more than 3-5 days. If you must, drink at least 3 liters of water daily. Get your lithium level checked 48-72 hours after starting the NSAID. Your doctor should reduce your lithium dose by 25-50% preemptively.
- Never restart an NSAID after stopping it without checking your lithium level. The effect lingers for 7-10 days. A single dose after a week off can still trigger toxicity.
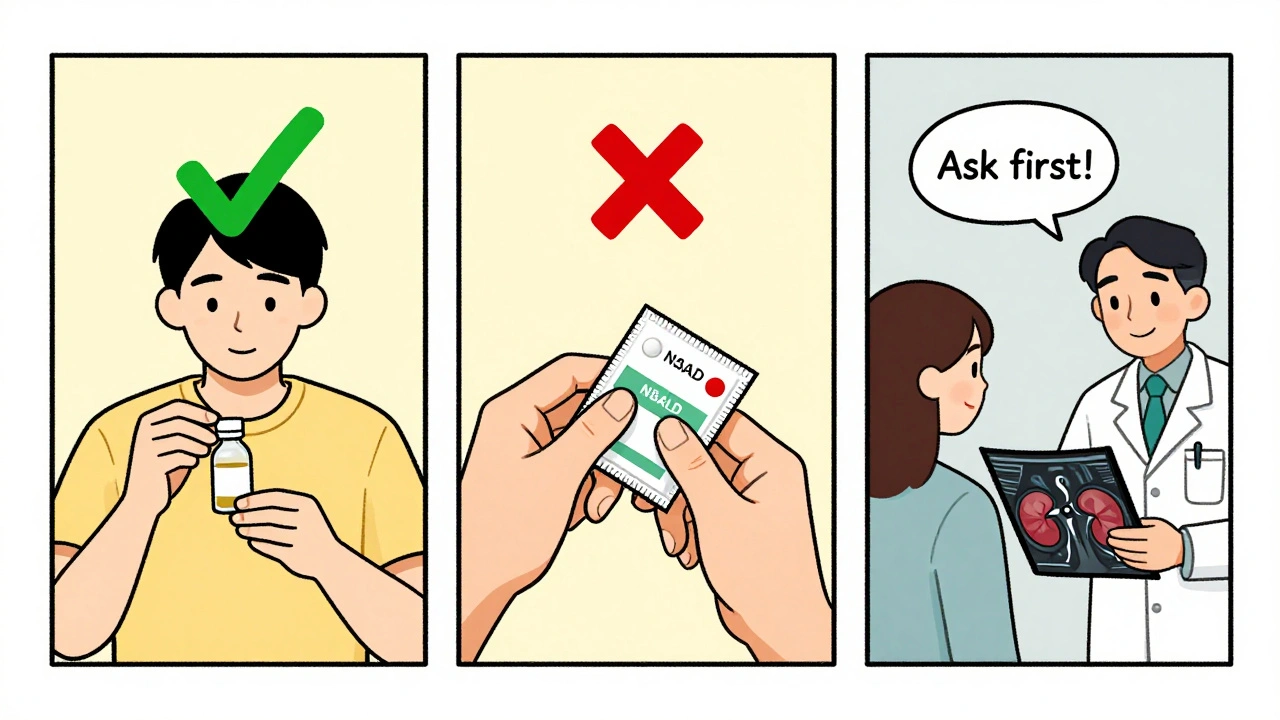
What Doctors Need to Do Better
The system is failing patients. Electronic health records have alerts for lithium-NSAID interactions - but they’re often ignored or turned off. A Kaiser Permanente program cut co-prescribing from 32% to 12% by forcing providers to complete a quick education module before prescribing NSAIDs to lithium users. The Veterans Health Administration, by contrast, saw only a minor drop - because alerts weren’t enforced consistently.The FDA now requires a boxed warning on lithium labels about NSAID risks. The European Medicines Agency is pushing for hard stops in e-prescribing systems - meaning a doctor can’t even write the prescription without a nephrologist’s note. But in the real world, these rules aren’t universal. Patients are still getting these dangerous combos because no one’s checking.
The Bigger Picture
As people live longer with bipolar disorder, more than 65% of lithium users are now over 50. Most have arthritis, back pain, or other chronic conditions. The pressure to prescribe NSAIDs is high. But the risk is too great. Some experts are now pushing for alternatives like valproate or lamotrigine, especially in older patients. But lithium still has one thing no other mood stabilizer can match: it cuts suicide risk by 44%. That’s why it’s still used - and why we need better pain solutions for those who take it.The solution isn’t to stop lithium. It’s to stop the NSAIDs. Better education, smarter alerts, and strict limits on NSAID use are the only ways forward. Until then, if you’re on lithium and reach for an over-the-counter painkiller, pause. Ask yourself: is this worth risking my kidneys - or my life?
Can I take ibuprofen if I’m on lithium?
No, ibuprofen significantly increases lithium levels by 20-30%, raising the risk of toxicity. Even short-term use can lead to tremors, confusion, kidney injury, or hospitalization. Acetaminophen is the safest pain reliever for lithium users.
How long does the lithium-NSAID interaction last?
The interaction doesn’t end when you stop the NSAID. Prostaglandin suppression can last 7-10 days, meaning lithium levels stay elevated. Never restart an NSAID after a break without checking your lithium level and consulting your doctor.
Is celecoxib safe with lithium?
No. While celecoxib is less harmful to kidneys than other NSAIDs, it still increases lithium levels by 10-15%. In patients with existing kidney problems, this can be enough to trigger toxicity. It should be avoided unless absolutely necessary and only with close monitoring.
What are the early signs of lithium toxicity?
Early signs include hand tremors, frequent urination, nausea, dizziness, and mild confusion. As it worsens, you may develop slurred speech, muscle weakness, seizures, or loss of coordination. If you experience any of these while taking an NSAID, stop the NSAID and seek medical help immediately.
Should I get my kidney function checked regularly if I’m on lithium?
Yes. All lithium users should have their kidney function (eGFR) and lithium levels checked every 3-6 months. If you’re taking NSAIDs, even occasionally, you need monitoring every 1-2 weeks during and after use. Older adults and those with existing kidney issues need even more frequent checks.
Are there any painkillers that are completely safe with lithium?
Acetaminophen (Tylenol) is the only commonly used painkiller with no significant interaction. Opioids like tramadol carry a small risk due to dehydration, but are safer than NSAIDs. Avoid all NSAIDs - including aspirin, naproxen, diclofenac, and meloxicam - unless under strict medical supervision.



Doug Hawk
Man i had no idea ibuprofen could wreck lithium levels like that. I’ve been popping Advil for my back since i started on lithium 3 years ago. Guess i’m switching to tylenol tomorrow. Scary how common this is.
Carolyn Woodard
The pharmacokinetic interplay here is profoundly underappreciated. Prostaglandin suppression leads to reduced renal perfusion, which in turn diminishes lithium’s glomerular filtration and tubular secretion. The result isn’t just elevated serum levels-it’s a cascade of tubular epithelial stress and eventual fibrotic remodeling. We’re talking about iatrogenic chronic kidney disease masked as "acute toxicity."
Saket Modi
bro why are we even talking about this?? just take tylenol. its literally the only thing that doesnt kill you. 😅
Chris Wallace
I’ve been on lithium for 11 years now. My nephrologist and psychiatrist both warned me about NSAIDs, but I didn’t realize how many doctors just don’t know. My ortho prescribed me naproxen last year for a herniated disc. I didn’t connect the dots until I started shaking at work. Had to get an ER visit and a 3-day hospital stay. Now I keep a list of safe meds on my phone. Everyone on mood stabilizers should do the same.
william tao
It is an egregious failure of the medical-industrial complex to permit such a well-documented, preventable, and statistically significant interaction to persist unmitigated in primary care settings. The absence of mandatory e-prescribing constraints constitutes a systemic dereliction of duty. One must ask: who profits from this negligence?
Sandi Allen
THIS IS WHY THE GOVERNMENT IS LYING TO YOU!! They don’t want you to know that Big Pharma pays doctors to push NSAIDs!! They know lithium saves lives, but they don’t want you to have safe pain relief because then you wouldn’t need MORE drugs!! I’ve seen the documents!! They’re hiding the truth!!
John Webber
my doc gave me naproxen last month and i felt weird but i thought it was just stress. now i think it was lithium toxicity. i’m gonna call him tomorrow. tylenol for life. no more dumb pills.
Shubham Pandey
tylenol works. done.
Elizabeth Farrell
If you’re on lithium and you’re reading this, please don’t feel guilty. You’re not alone. So many of us have been caught off guard by this. But now you know. And knowledge is power. Start a conversation with your provider. Bring this article. Ask for a lab check. You’re not being dramatic-you’re being smart. And you deserve to manage your pain without risking your kidneys. You’ve already survived so much. Don’t let a simple painkiller undo it.
Sheryl Lynn
Oh darling, it’s not just the NSAIDs-it’s the entire biomedical paradigm’s utter failure to integrate psychiatric pharmacology with geriatric nephrology. The clinical indifference is positively Victorian. One might argue that the medical establishment views bipolar patients as statistically acceptable collateral damage in the pursuit of pain management metrics. How quaintly cruel.
Paul Santos
So basically, we’re living in a world where your brain stabilizer is more dangerous than your painkiller? 😅 Classic. I mean, I get it-lithium’s the OG mood stabilizer. But maybe it’s time we stopped treating it like some sacred relic and started prioritizing safety over tradition. Tylenol > ibuprofen. Tramadol > naproxen. And if your doc doesn’t know that… maybe it’s time to find a new one.
Eddy Kimani
This is why I always check drug interaction databases before taking anything new. Even if it’s OTC. I’ve been on lithium for 8 years and I’ve never taken an NSAID. I keep a printed list in my wallet. My wife calls me obsessive. I call it survival. If you’re on lithium, do yourself a favor and make your own list. Save your kidneys. Save your life.
Chelsea Moore
I just got diagnosed with stage 3 kidney disease last month. My eGFR is 42. My ortho prescribed me meloxicam. My psychiatrist didn’t know. My PCP didn’t know. I thought I was just getting older. Now I’m terrified. I cried for an hour. I’m not mad at anyone-I’m just so, so scared. I didn’t know this could happen from a pill. Please, if you’re reading this… please, please, please ask your doctor. Don’t wait until it’s too late.
John Biesecker
Just want to say thank you for writing this. I’ve been on lithium since I was 19. Now I’m 47. I’ve had 3 hospitalizations from lithium toxicity-all because of NSAIDs. I thought I was just unlucky. Turns out, I was just uninformed. I’ve been telling everyone I know now. This isn’t just medical advice-it’s a lifeline. 🙏