Medication Risk Assessment Tool
Understanding Your Risk
This tool helps you assess your risk of developing medication-related suicidal thoughts based on factors mentioned in the article. Your information is confidential and not saved.
It’s not rare, but it’s often missed: someone starts a new medication for depression or anxiety, and within days, they feel worse-not just emotionally, but in a way that scares them. They can’t sit still. Thoughts of ending their life pop into their head, but they don’t feel like their thoughts. They feel alien, forced, out of control. This isn’t the depression coming back. This is something else.
What’s Really Happening?
Some medications, especially antidepressants, can trigger a sudden surge in agitation, restlessness, and suicidal thoughts. This isn’t the illness worsening. It’s a side effect-a rare but dangerous reaction called the activation syndrome. It happens when the brain gets overstimulated too quickly by the drug, and the person’s natural coping mechanisms get overwhelmed. The U.S. Food and Drug Administration (FDA) confirmed this link in 2007 after reviewing data from thousands of patients. Since then, all antidepressants carry a black box warning-the strongest safety alert-for increased risk of suicidal thoughts in people under 25. But the problem goes beyond antidepressants. Even antibiotics like doxycycline, painkillers like piroxicam, and even some cancer drugs have been tied to sudden suicidal urges in rare cases.The Three Key Warning Signs
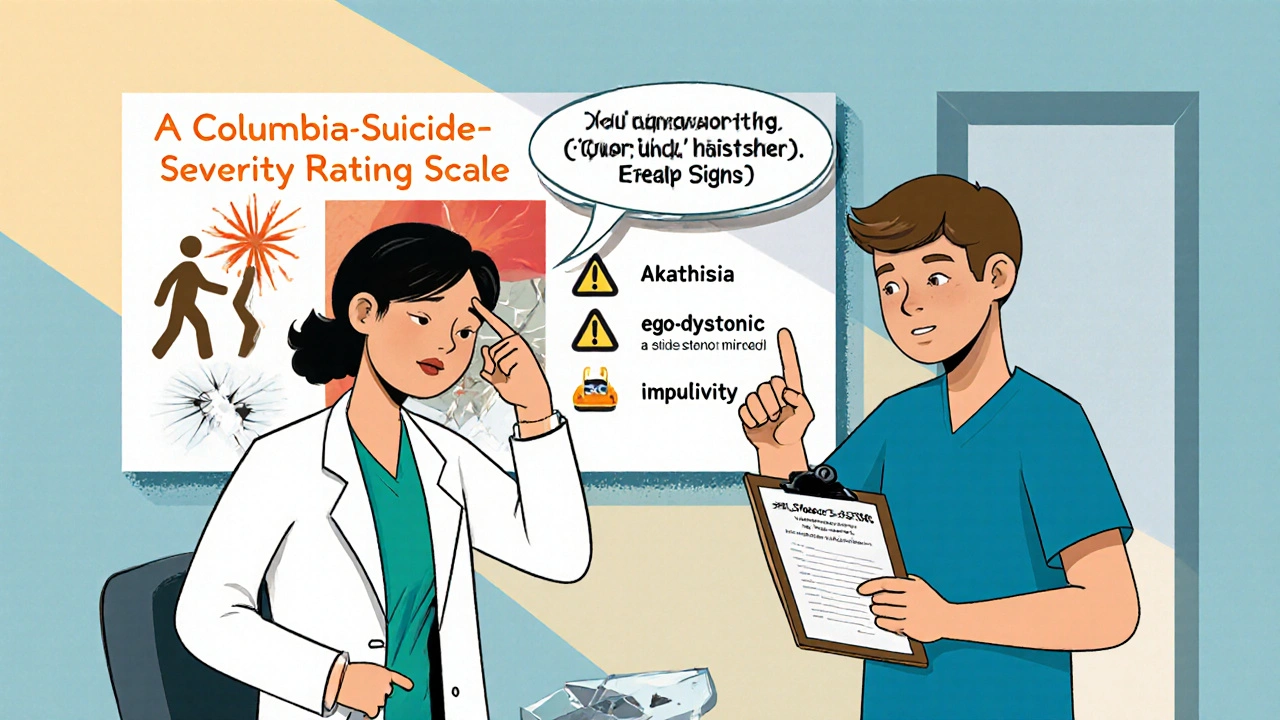
If you or someone you care about starts a new medication, watch for these three red flags, especially in the first four weeks:- Restlessness you can’t shake - This isn’t just being fidgety. It’s an intense, painful urge to move. You can’t sit still. You pace. You shift constantly. You feel like your nerves are on fire. This is called akathisia, and it’s the most common sign-found in over half of all cases. Studies show people with akathisia are far more likely to act on suicidal thoughts.
- Thoughts that feel foreign - You don’t want to die. You’ve never felt this way. But suddenly, images of suicide keep popping up. They don’t match your values, your personality, your hopes. You feel like someone else is putting these thoughts in your head. This is called ego-dystonic thinking. It’s a major red flag because it means the thoughts aren’t coming from your depression-they’re coming from the drug.
- Impulsiveness you can’t control - You make sudden, reckless decisions. You yell at people. You cancel plans. You text someone you haven’t spoken to in years. You think, “I just need this to stop,” and act on it without planning. When this combines with depression, the risk spikes.
These signs don’t always show up together. Sometimes just one is enough. And they usually appear fast-within days, rarely after a month.
Who’s Most at Risk?
Age is the biggest factor. People under 25 have 2.3 times the risk compared to adults over 24. But other factors stack the deck:- Previous suicide attempt - increases risk by 47%
- Family history of suicide - adds 32% more risk
- Anxiety disorder along with depression - boosts risk by 58%
- Starting with a high dose or increasing the dose too fast - raises risk by 63%
It’s not about being “weak” or “overreacting.” It’s biology. Some people’s brains process these drugs differently because of their genes-especially genes like CYP2D6 and CYP2C19, which control how fast the body breaks down medication. If your body processes the drug too slowly, it builds up and overstimulates your brain.
It’s Not Just Antidepressants
Most people think only antidepressants cause this. But research from 2024 shows at least nine other drugs have strong links to suicidal reactions:| Medication Class | Examples | Typical Onset |
|---|---|---|
| SSRIs | Fluoxetine, sertraline, escitalopram | 1-14 days |
| SNRIs | Duloxetine, venlafaxine | 2-14 days |
| Antibiotics | Doxycycline | 7-21 days |
| Anti-inflammatories | Piroxicam | 10-28 days |
| Cancer drugs | Paclitaxel | 1-4 weeks |
| Biologics | Adalimumab, infliximab | 2-8 weeks |
Doxycycline stands out. It’s a common antibiotic. But in rare cases, it interferes with brain chemicals tied to mood regulation. One patient developed suicidal thoughts after just 10 days on a standard dose. Their doctor didn’t connect the dots-until it was almost too late.
What to Do If You See These Signs
If you notice any of these warning signs in yourself or someone else:- Don’t wait. Call your doctor immediately. Don’t wait for your next appointment. This is an emergency.
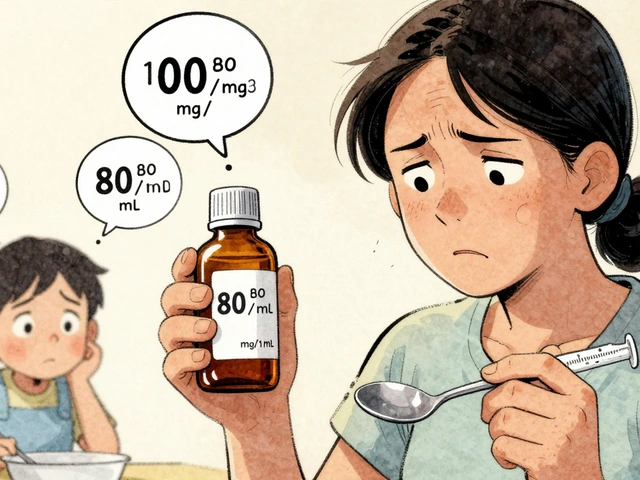
- Don’t stop cold turkey. Stopping antidepressants suddenly can cause withdrawal that feels worse than the original symptoms. But you also shouldn’t keep taking it if you’re having these reactions. Your doctor can help you taper safely.
- Get support. Call a crisis line. Stay with someone you trust. Don’t be alone.
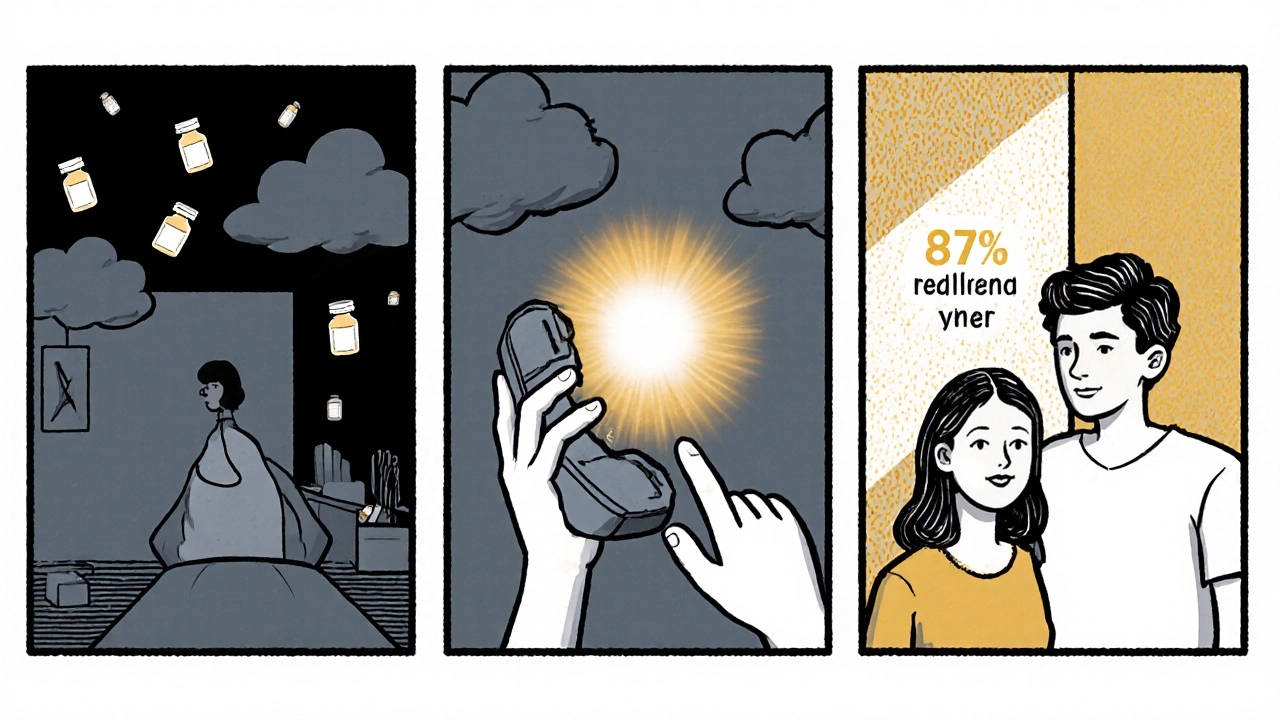
Studies show that in 87% of cases, these suicidal thoughts disappear within days of stopping the medication. That’s not a coincidence. It’s proof that the drug was the trigger-not the illness.
How Doctors Should Be Monitoring
The FDA recommends weekly check-ins during the first month of starting an antidepressant. But only 68% of doctors actually document discussing warning signs with patients during the consent process. The best tool doctors use is the Columbia-Suicide Severity Rating Scale (C-SSRS). It’s not a quiz-it’s a conversation. It asks direct questions like:- “Have you had thoughts that you’d be better off dead?”
- “Have you had thoughts of hurting yourself?”
- “Have you made any plans to end your life?”
When used properly, it catches 89% of emerging risks. But it only works if the doctor asks-and if the patient feels safe enough to answer honestly.
What You Can Do Right Now
If you’re starting a new medication:- Ask your doctor: “Could this cause restlessness or strange suicidal thoughts?”
- Ask: “What should I do if I feel like I’m losing control of my thoughts?”
- Write down the warning signs and keep them on your phone or fridge.
- Give a trusted friend or family member a copy of these signs and ask them to check in daily for the first two weeks.
- Use a mood tracker app. Many now monitor sleep, movement, and social activity-changes in these can signal trouble before you even notice it.
And if you’re already on medication and feeling off-don’t blame yourself. Don’t think you’re failing. You’re not. You’re experiencing a known, documented side effect. The fact that you’re noticing it means you’re paying attention-and that’s the first step to staying safe.
The Bigger Picture
Yes, antidepressants save lives. For most people, they work. But medicine isn’t one-size-fits-all. What helps one person can hurt another. That’s why monitoring isn’t optional-it’s essential. New tools are coming. In 2024, the FDA began requiring all new antidepressants to include activation syndrome screening in clinical trials. Researchers are now using AI to predict who’s at risk based on genetics, behavior, and health records. One pilot program in Boston already predicts high-risk patients with 82% accuracy. But until those systems are everywhere, the most powerful tool is still you-knowing what to look for, speaking up, and acting fast.Can antidepressants really cause suicidal thoughts?
Yes. While antidepressants help most people, they can trigger sudden suicidal thoughts in a small but significant number-especially those under 25. This is called activation syndrome. It’s not the depression getting worse-it’s a side effect caused by how the brain reacts to the drug. Studies show this happens in 1-4% of young adults, with symptoms appearing within the first few weeks.
What’s the difference between depression and drug-induced suicidal thoughts?
Depression-related thoughts usually feel like a natural part of your sadness-you believe you’re a burden, the world is hopeless, and you deserve to die. Drug-induced thoughts feel alien. You don’t want to die, but the thoughts keep appearing anyway. They’re intrusive, urgent, and don’t match your values. You might even say, “This isn’t me.” That’s a key sign it’s the medication, not your illness.
Is akathisia the same as anxiety?
No. Anxiety is mental-worry, fear, racing thoughts. Akathisia is physical and unbearable. It’s a deep, restless urge to move that you can’t ignore. You pace, shift, fidget constantly. It’s painful. Studies show people with akathisia are far more likely to act on suicidal thoughts because the discomfort becomes unbearable. It’s not just nervous energy-it’s a neurological reaction.
How long do these side effects last?
If caught early and the medication is stopped or adjusted, suicidal thoughts and restlessness usually go away within 3-7 days. In one 2024 study, 87% of patients saw complete resolution after discontinuing the drug. But if ignored, the risk of a suicide attempt increases sharply. Don’t wait it out-act fast.
Should I stop taking my medication if I have these thoughts?
Don’t stop abruptly. Stopping suddenly can cause withdrawal symptoms that feel worse than the original problem. But don’t keep taking it if you’re having these reactions. Call your doctor right away. They can help you taper safely or switch to a different medication. Your safety matters more than sticking to a plan.
Are there other drugs besides antidepressants that can cause this?
Yes. Antibiotics like doxycycline, painkillers like piroxicam, cancer drugs like paclitaxel, and even biologics used for autoimmune diseases have been linked to sudden suicidal urges. These aren’t listed on most labels, but research confirms the risk. If you start any new medication and feel unusually agitated or have strange suicidal thoughts, tell your doctor-even if it’s not a psychiatric drug.
Can I prevent this from happening?
You can reduce the risk. Ask your doctor about your personal risk factors-like age, past suicide attempts, or family history. Request a slow, gradual dose increase. Ask for a safety plan before starting. Tell someone you trust to check in with you daily for the first two weeks. Use a mood tracker. Knowledge and preparation save lives.




Daisy L
This is the most important post I’ve read this year-seriously. I had akathisia from sertraline and thought I was losing my mind. Pacing for hours, heart racing, thoughts screaming at me to jump out the window-except I didn’t WANT to die. I just wanted the noise to STOP. My doctor called it ‘anxiety’ and upped my dose. I almost didn’t make it to the next week. Don’t let them gaslight you. If it feels alien-it’s the drug. Not you.
Anne Nylander
thank you for sharing this!! i had no idea doxycycline could do this!! my cousin went from fine to crying in the shower and saying ‘i just wanna disappear’ after 12 days on it. her doctor said ‘it’s just stress’ but she stopped the med and boom-gone in 3 days. you’re right-this needs to be talked about more!!
Franck Emma
They don’t warn you because they’re scared of lawsuits. Not because they care about you.
Noah Fitzsimmons
Oh wow, so now we’re blaming Big Pharma for people who just can’t handle their emotions? Cute. Next you’ll say antidepressants make you gay. Look, if your brain can’t handle a little serotonin boost, maybe you shouldn’t be on meds at all. This isn’t a horror movie. It’s pharmacology.
Eliza Oakes
Wait-so you’re saying the FDA’s black box warning is somehow NOT enough? That we need a whole damn TED Talk on how to not die from a pill? Newsflash: people have been dying from SSRIs since the 90s. And yet, doctors still prescribe them like candy. This isn’t new. It’s just now you’re pretending to be surprised. Also-biologics? Really? You’re telling me my Humira is secretly trying to kill me? I’m not buying it.
Sammy Williams
Man, I wish I’d read this before I started venlafaxine. I thought I was just being ‘edgy’ for a week. Turns out I was pacing in circles at 3 a.m., texting my ex saying ‘I’m sorry I’m a burden’-and I didn’t even like her anymore. Stopped the med, called my doc, got switched to bupropion. Zero issues since. Just… talk to someone. Don’t suffer in silence. You’re not weak for noticing this.
Michael Marrale
Did you know the FDA and Big Pharma are working with the CDC to hide this? They’re using AI to flag people who search for ‘suicidal thoughts after antibiotics’ and then send them targeted ads for more meds. I saw the whistleblower docs. They’re calling it ‘Project Silent Mind.’ Your phone’s listening. Your smart fridge knows. You’re being manipulated. Don’t take another pill until you’ve checked your CYP2D6 status. I got mine tested-turns out I’m a slow metabolizer. That’s why I almost died on fluoxetine. They don’t test this stuff. Ever.
David vaughan
Thank you for posting this. I’ve been too scared to say anything out loud. I started doxycycline for acne, and by day 8, I had this voice in my head saying ‘just end it.’ I didn’t feel sad-I felt like someone was whispering it into my ear. I stopped the antibiotic and called my doctor. They didn’t believe me at first. But I sent them this post. They apologized. It’s been 5 days since I stopped. The voice is gone. I’m alive. I’m so glad I’m not alone.