When you’re on antibiotics, your gut knows it. The good bacteria, the ones that help you digest food, keep your immune system in check, and even influence your mood-they get wiped out along with the bad guys. That’s why so many people end up with diarrhea, bloating, or yeast infections after a course of antibiotics. But here’s the thing: taking probiotics at the same time doesn’t fix it. In fact, if you take them together, you’re probably wasting them.
Why Timing Matters More Than You Think
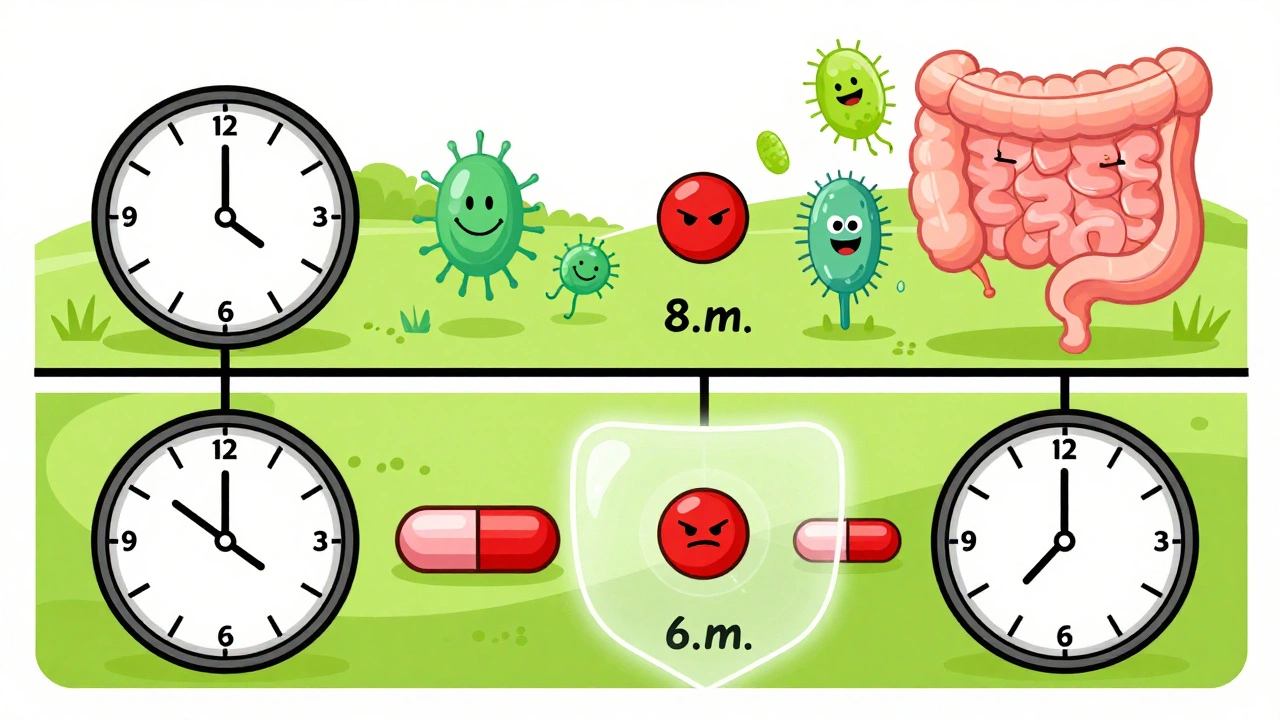
Antibiotics don’t pick and choose. They kill bacteria-period. That includes the live cultures in your probiotic supplement. If you swallow a pill with 20 billion CFUs of Lactobacillus right after your amoxicillin, those bacteria won’t survive long enough to do anything. Studies show that without proper spacing, probiotic viability drops by 78% to 92%. That’s not just a small loss-it’s almost total failure. The fix isn’t complicated: space them out by at least two hours. This gives your body time to process the antibiotic before the probiotic enters the mix. Think of it like this: antibiotics move fast through your gut. By the time they’ve passed through the upper intestine, most of them are already out of the system. That’s your window.How to Actually Do It
Let’s say your doctor prescribed amoxicillin twice a day-at 8 a.m. and 8 p.m. Here’s what your schedule should look like:- Take your probiotic at 6 a.m. and 6 p.m.
- Or, if that’s easier, take it at 10 a.m. and 10 p.m.
Not All Probiotics Are the Same
You can’t treat all probiotics the same. There are two main types: bacterial and yeast-based. Bacterial strains like Lactobacillus rhamnosus GG and Bifidobacterium are sensitive to antibiotics. They need that two-hour gap. But Saccharomyces boulardii is a yeast. It’s not affected by antibiotics at all. That means you can take it at the same time as your antibiotic without losing effectiveness. In fact, it’s one of the most studied strains for preventing antibiotic-associated diarrhea. Here’s what the data says about effectiveness:- Saccharomyces boulardii (20 billion CFU/day): 52% lower risk of diarrhea
- Lactobacillus rhamnosus GG (10-20 billion CFU/day): 47% lower risk
Dosing: How Much Do You Actually Need?
It’s not just about timing-it’s about how much you take.- Mild cases (short antibiotic course, no prior gut issues): 5-10 billion CFU per day
- Diarrhea or moderate disruption: 10-20 billion CFU per day
- Long-term antibiotics (14+ days) or existing gut problems: 20-40 billion CFU per day
What About Probiotic Foods?
Yogurt, kefir, sauerkraut-they’re great. But they’re not enough. A serving of yogurt might have a few billion CFUs, and those strains aren’t always the ones proven to work with antibiotics. Plus, the bacteria in fermented foods aren’t always stable or guaranteed to survive stomach acid. If you’re serious about protecting your gut, rely on a high-quality supplement during and after antibiotics. Use food as a bonus, not your main defense.Common Mistakes (And How to Avoid Them)
Here’s what most people get wrong:- Taking probiotics right after antibiotics → You’re killing them before they start.
- Stopping probiotics when antibiotics end → You’re leaving your gut vulnerable.
- Choosing a cheap, no-name brand → Only 32% of probiotic products on the market list the exact strain. If you can’t find the strain name, you can’t know if it’s effective.
- Assuming more strains = better results → Science says no. Stick to LGG or S. boulardii.
What the Experts Say
The International Scientific Association for Probiotics and Prebiotics (ISAPP) says: start probiotics as soon as possible after beginning antibiotics-within 1-2 days-and keep going for 7-14 days after. Harvard Medical School agrees: probiotics can cut diarrhea risk by up to 50%. The NIH confirms: LGG and S. boulardii are the two best-studied strains with the strongest evidence. One expert, Dr. Emeran Mayer from UCLA, warns that for broad-spectrum antibiotics like ciprofloxacin, it might be safer to wait until after the course ends. But that’s an exception, not the rule. For most people, starting early works best.
What’s Next? The Future of Probiotics
Researchers are working on time-release capsules and acid-resistant coatings that might one day let you take probiotics with antibiotics without spacing. Companies like Seed and Pendulum are already testing these. But as of late 2024, none have been approved for mainstream use. Until then, the two-hour rule is still the gold standard-backed by 27 out of 31 major medical institutions. It’s simple, it’s proven, and it’s free of side effects.FAQ
Can I take probiotics and antibiotics at the same time?
Only if the probiotic is yeast-based, like Saccharomyces boulardii. Bacterial probiotics like Lactobacillus and Bifidobacterium will be killed by antibiotics if taken together. For those, you need at least a two-hour gap.
How long should I take probiotics after antibiotics?
Continue for 7 to 14 days after your last antibiotic dose. Studies show this helps restore your gut microbiome to near-normal levels. Stopping sooner reduces recovery by up to 26%.
What’s the best probiotic strain to take with antibiotics?
Lactobacillus rhamnosus GG and Saccharomyces boulardii are the two most effective. LGG is best for bacterial probiotics, and S. boulardii is the only yeast strain proven to work alongside antibiotics without spacing.
Do I need a high CFU count?
Yes. For most people, 10-20 billion CFU per day is the sweet spot. Lower doses (under 5 billion) rarely show benefit. Higher doses (20-40 billion) are recommended for long antibiotic courses or if you already have gut issues.
Can I get enough probiotics from yogurt or fermented foods?
No. Fermented foods contain far fewer live cultures than supplements, and the strains aren’t always the ones proven to prevent antibiotic-related diarrhea. Use them for general gut health, but rely on a supplement during and after antibiotics.
What if I forget to space them?
Don’t panic. Just take your probiotic as soon as you remember, and wait two hours before your next antibiotic dose. Missing one or two doses reduces effectiveness, but it doesn’t ruin everything. Just get back on schedule.
Are multi-strain probiotics better?
No. Multiple studies show no significant advantage over single-strain probiotics for preventing antibiotic-associated diarrhea. Stick with proven strains like LGG or S. boulardii instead of paying more for unproven blends.
Can probiotics cause side effects with antibiotics?
Rarely. The most common side effect is mild bloating or gas, especially at first. Serious reactions are extremely uncommon. If you’re immunocompromised, talk to your doctor before starting any probiotic.




Arjun Deva
So you're telling me Big Pharma doesn't want us to know this? Of course they don't-they profit off gut disasters, then sell us $40 bottles of 'probiotics' that are just sugar and lies!!! Two hours? HA! They probably want you to take them together so you keep coming back for more antibiotics!!!
Inna Borovik
While the two-hour spacing guideline has some empirical support, the clinical significance of microbiome recovery metrics remains contested. Many studies suffer from small sample sizes and lack of longitudinal follow-up. Also, CFU counts are not standardized across assays-this entire framework feels like over-interpretation of preliminary data.
Jackie Petersen
Oh great, now I have to plan my probiotic intake like a military operation? I'm not a robot. I take my meds when I remember. If I get diarrhea, I'll just take Imodium. It's cheaper, faster, and doesn't require a PhD in gut microbiology.
Annie Gardiner
But what if the real problem isn't the antibiotics? What if it's the entire industrial food system that's destroyed our gut flora before we even take the pills? We're treating symptoms while ignoring the disease of modernity. Probiotics are just a Band-Aid on a severed artery. We need to reconnect with the earth, eat wild fermented foods, and stop trusting scientists who wear lab coats like armor.
Rashmi Gupta
Two hours? In India, people take probiotics with antibiotics and never have issues. Maybe this is a Western overcomplication. Our grandmothers never measured CFUs-they just ate yogurt with meals. Maybe the answer isn't science… it's tradition.
Max Manoles
There's a subtle but critical flaw in the assumption that probiotic viability equals clinical benefit. Even if 90% of the bacteria die, the remaining 10% may still trigger immune modulation or release beneficial metabolites. The dead bacteria themselves may act as prebiotics. This entire argument hinges on a reductionist view of gut ecology that ignores the complexity of microbial signaling.
Katie O'Connell
One must exercise considerable discernment when evaluating the methodological rigor of the cited studies. The majority of randomized controlled trials referenced exhibit significant heterogeneity in strain characterization, dosage metrics, and endpoint definitions. To assert a 'gold standard' based on such a fragmented evidence base is, frankly, premature and potentially misleading to the lay public.
Kumar Shubhranshu
Just take S. boulardii anytime. Done. No stress. No math. No money wasted on fancy bottles. You're welcome.
Mayur Panchamia
Western science thinks it knows everything! In India, we've been using curd and neem for centuries-no lab tests needed! You think your 20 billion CFUs are better than our grandma's kitchen wisdom? HA! Your probiotics are probably made in China and full of toxins! Trust your roots, not some white-coated pharma puppet!
Nava Jothy
I've been on 12 different antibiotics since 2018… and I've tried EVERYTHING. Probiotics? No. Prebiotics? Meh. FMT? I cried. I'm just saying… if your gut can't handle antibiotics, maybe you shouldn't be taking them in the first place? Who gave you the right to poison your body like this? 😔
brenda olvera
This is so helpful!! I started taking S. boulardii with my amoxicillin and I felt like my insides finally stopped screaming. I didn't even know yeast probiotics were a thing. Thank you for making this feel doable, not scary. Your post gave me hope. 🌱💛
Myles White
Actually, I think the real issue here is that we're approaching gut health with a mechanistic, reductionist mindset-treating it like a plumbing system where you just flush out the bad stuff and replace it with good stuff. But the microbiome isn't a collection of discrete organisms; it's a dynamic, self-organizing ecosystem shaped by diet, stress, sleep, circadian rhythms, even social interaction. The two-hour rule might help, but if you're still eating processed food, sleeping 4 hours a night, and scrolling TikTok at 2 a.m., you're just putting a bandage on a hemorrhage. We need to stop optimizing symptoms and start healing the conditions that made us sick in the first place. I've been reading up on polyphasic microbial succession models-turns out, the timing of probiotic intake is just one tiny variable in a vast, nonlinear system that we barely understand. Maybe the real answer isn't in spacing, but in surrendering control and letting the gut rewild itself.