Anticoagulant Rifampin Interaction Calculator
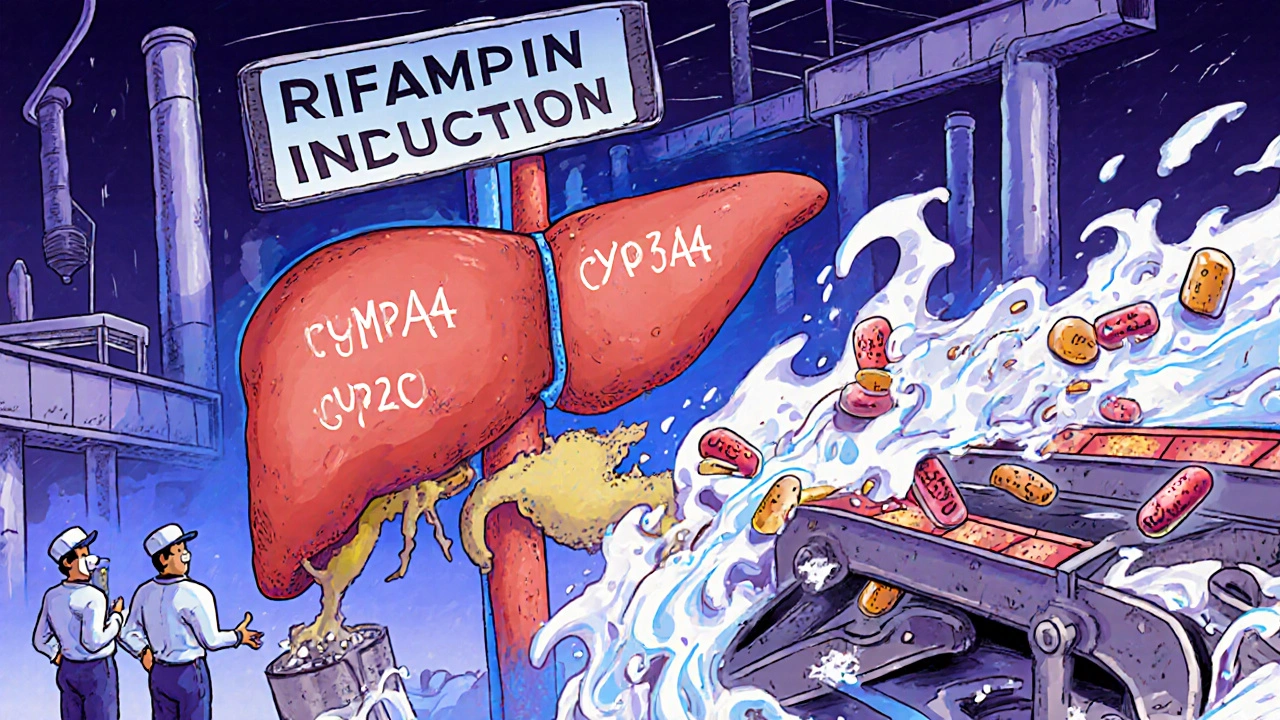
Rifampin is a strong inducer of liver enzymes (CYP3A4 and CYP2C9) that process anticoagulants. This calculator shows you the estimated reduction in drug levels based on your current medications and duration of rifampin treatment.
Remember: This is for educational purposes only. Always consult your doctor before making any medication adjustments.
When you’re on rifampin for tuberculosis or to prevent meningitis, you might not think about how it’s quietly changing the way your other medications work. But for people taking anticoagulants like warfarin or direct oral anticoagulants (DOACs), or even some antivirals, rifampin can be a silent threat. It doesn’t just kill bacteria-it rewires your body’s ability to process other drugs. And that can mean the difference between being protected from a clot and facing a stroke or pulmonary embolism.
How Rifampin Changes Your Body’s Drug Processing
Rifampin is one of the strongest known inducers of liver enzymes, especially CYP3A4 and CYP2C9. These enzymes are like factory workers that break down drugs so your body can get rid of them. When rifampin shows up, it tells your liver to make more of these workers-fast. Within 24 to 48 hours, enzyme levels start rising. By day five to seven, they’re at peak output. Even after you stop rifampin, it takes two to three weeks for those extra enzymes to break down and disappear.
This isn’t just about speed-it’s about volume. Studies show rifampin can slash the concentration of sensitive drugs by 50% to 80%. That means if you’re taking a blood thinner, your body is clearing it out so quickly that it never reaches the level needed to work. The mechanism? Rifampin activates the pregnane X receptor (PXR), a switch in your liver cells that turns on genes responsible for making drug-metabolizing enzymes. It’s not a direct effect-it’s a genetic command.
Warfarin and Other Vitamin K Antagonists: A Dangerous Drop
Warfarin has been the go-to anticoagulant for decades, and it’s especially vulnerable to rifampin. About 70% of warfarin is broken down by CYP2C9, and rifampin turns that enzyme into a hyperactive machine. A systematic review found that rifampin reduces warfarin’s blood levels by 15% to 74%. The more potent S-warfarin isomer drops even more than the R-form.
What does that look like in real life? A 57-year-old woman with a mechanical heart valve was stable on phenprocoumon, another vitamin K antagonist. When she started rifampin for suspected endocarditis, her INR-her blood clotting measure-plummeted into the normal range. She wasn’t bleeding, but she wasn’t protected either. Her doctors had to switch her to heparin injections until 15 days after rifampin ended, when her INR finally crept back up. That’s not rare. It’s textbook.
Some patients need to triple or even quintuple their warfarin dose just to stay in range while on rifampin. But even then, it’s a tightrope walk. INR levels can swing wildly. One day you’re safe, the next you’re at risk. That’s why the American College of Chest Physicians recommends switching from warfarin to low molecular weight heparin (LMWH) during rifampin treatment. It’s not ideal-shots every day are inconvenient-but it’s predictable. LMWH doesn’t rely on CYP enzymes, so rifampin can’t touch it.
Direct Oral Anticoagulants (DOACs): No Safety Net
DOACs like apixaban, rivaroxaban, dabigatran, and edoxaban were supposed to be easier than warfarin. No regular blood tests. Fewer food interactions. But rifampin doesn’t care. It hits them just as hard.
Studies show:
- Dabigatran: 50-60% drop in blood levels
- Apixaban: 50-67% drop
- Rivaroxaban: 50-67% drop
- Edoxaban: 35% drop, but its active metabolites increase slightly-no real safety net
The European Heart Rhythm Association says combining DOACs with rifampin is generally not recommended. Why? Because unlike warfarin, you can’t check their levels with a simple blood test. You don’t know if the drug is working until it’s too late. A patient might think they’re protected because they’re taking their pill every day-until they have a clot.
One small study of six patients with prosthetic joint infections on rivaroxaban and rifampin found that simply increasing the dose didn’t fix the problem. The interaction was too complex. The researchers suggested gradual adjustments-neither jumping up the dose immediately nor stopping rifampin cold turkey. But even that’s a gamble. Most hospitals don’t have protocols for this. As of 2022, only 12% of U.S. hospitals had written guidance for managing DOAC-rifampin interactions.

Antivirals in the Crosshairs
Rifampin doesn’t stop at blood thinners. Many antivirals are also broken down by CYP3A4. That includes:
- HIV protease inhibitors (like darunavir, atazanavir)
- Direct-acting antivirals for hepatitis C (like elbasvir/grazoprevir)
- Some antivirals used for COVID-19 (like nirmatrelvir/ritonavir-Paxlovid)
For HIV patients on antiretrovirals, rifampin can drop drug levels so low that the virus rebounds. That’s why guidelines say you shouldn’t combine rifampin with most HIV meds unless you switch to a rifabutin-based regimen (a weaker inducer). For hepatitis C, combining rifampin with certain antivirals can lead to treatment failure. And for Paxlovid? The combination is contraindicated. The ritonavir component in Paxlovid is meant to boost drug levels-but rifampin overwhelms it. The result? No antiviral effect, and a higher chance of viral mutation.
What Do Guidelines Say? What Should You Do?
The advice is clear: avoid combining rifampin with anticoagulants and most antivirals if you can.
If you absolutely must use both:
- For warfarin: Switch to LMWH during rifampin therapy. Retitrate warfarin slowly after rifampin ends, checking INR daily at first.
- For DOACs: Avoid if possible. If no alternative exists, use the highest approved dose, monitor for signs of clotting (swelling, chest pain, shortness of breath), and consider anti-Xa levels if available (though they’re not standardized).
- For antivirals: Check specific guidelines. For HIV, use rifabutin instead. For Hep C, avoid rifampin entirely. For Paxlovid, do not use together.
There’s one exception: rivaroxaban. A 2021 study suggested that with careful, monitored dose increases, it might be usable in rare cases where no other option exists. But this is not standard care. It’s a last-resort experiment.
What’s Next? New Drugs, Better Safety
Researchers are already designing the next generation of anticoagulants to avoid this problem. One promising candidate, milvexian, targets factor XIa instead of thrombin or factor Xa. Early data suggests it’s less affected by CYP3A4 induction. The FDA now requires new drugs to be tested against strong inducers like rifampin before approval. That’s a big shift. It means future anticoagulants may be safer.
Meanwhile, point-of-care INR devices have improved. Modern devices are 95% accurate within ±0.5 INR units of lab tests. That helps warfarin users manage their levels better during rifampin treatment. But for DOACs? There’s still no reliable monitoring tool. That’s the biggest gap.
Bottom Line: Know the Risk, Plan Ahead
If you’re prescribed rifampin and you’re on a blood thinner or antiviral, don’t assume everything will be fine. Talk to your doctor before you start. Ask: "Is this combination safe? Do I need to switch medications? What signs of a clot should I watch for?"
This isn’t a theoretical risk. It’s happened to real people. People with heart valves, with atrial fibrillation, with cancer, with HIV. Some survived because their doctors caught it early. Others didn’t.
Rifampin is powerful. But so are the drugs it interferes with. When they clash, the body pays the price. The key isn’t just knowing the interaction-it’s planning for it before you ever take the first pill.
Can I take warfarin with rifampin?
You can, but it’s risky. Rifampin can reduce warfarin levels by up to 74%, leading to dangerous drops in INR and increased clot risk. Most experts recommend switching to low molecular weight heparin (LMWH) injections during rifampin treatment. If you must stay on warfarin, your dose may need to be tripled or more, with daily INR monitoring until stable. Always work with your doctor-never adjust on your own.
Are DOACs like apixaban or rivaroxaban safer than warfarin with rifampin?
No. DOACs are just as vulnerable to rifampin, with blood levels dropping 50-67%. The big problem? Unlike warfarin, there’s no routine blood test to check if they’re working. You won’t know you’re underdosed until you have a stroke or clot. Guidelines say combining DOACs with rifampin should be avoided. If absolutely necessary, use the highest approved dose and watch closely for signs of clotting-swelling, chest pain, trouble breathing.
Can I take Paxlovid with rifampin?
No. Rifampin makes Paxlovid ineffective. The ritonavir in Paxlovid is meant to boost nirmatrelvir levels, but rifampin shuts down the liver enzymes that hold it up. This combination can lead to treatment failure and possible viral resistance. If you need antiviral treatment for COVID-19 and are on rifampin, talk to your doctor about alternatives like remdesivir or nirmatrelvir without ritonavir, if available.
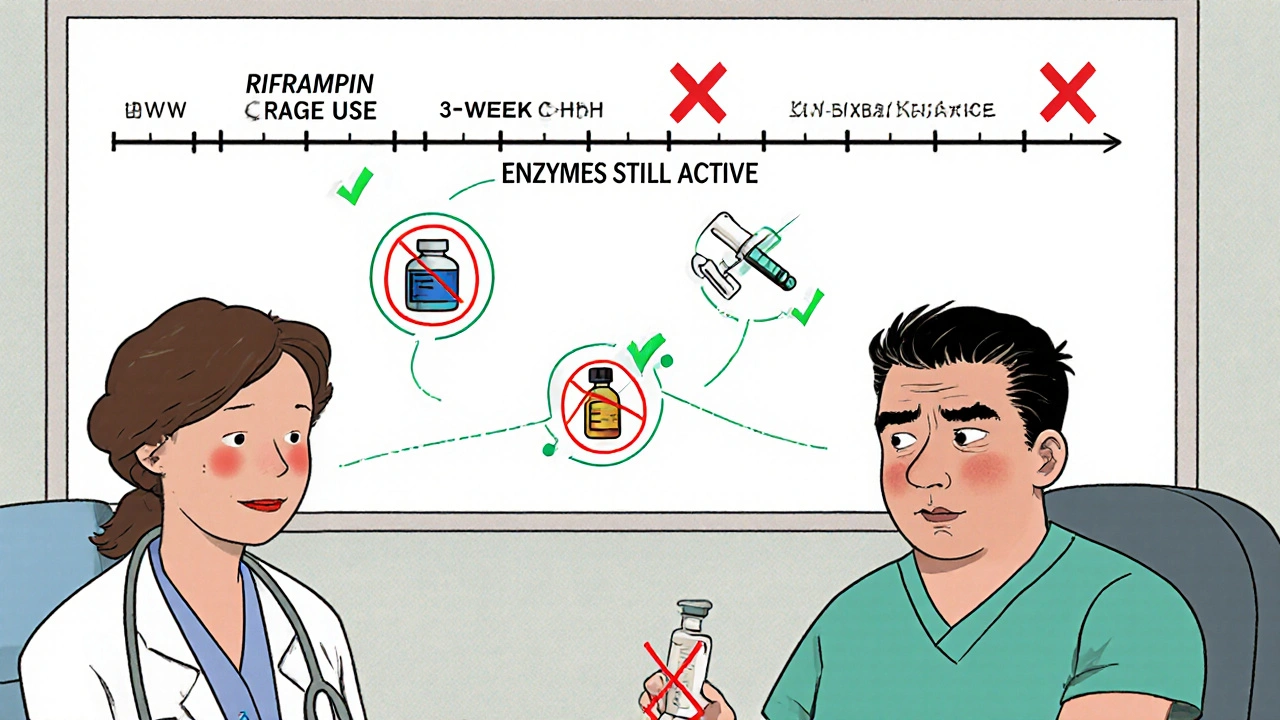
How long does rifampin’s effect last after I stop taking it?
The enzyme-inducing effects of rifampin can last 2 to 3 weeks after you stop taking it. Your body needs time to break down the extra CYP3A4 and CYP2C9 enzymes. That means even after you finish rifampin, your anticoagulant or antiviral doses may still be too low. Don’t assume you can go back to your old dose right away. Work with your doctor to slowly adjust medications over several weeks.
Is there a better antibiotic than rifampin for TB that doesn’t cause these interactions?
Rifabutin is a weaker inducer of CYP enzymes and is sometimes used as an alternative in HIV patients on antiretrovirals. But for tuberculosis, rifampin remains the gold standard because it’s more effective at killing the bacteria. Rifabutin is not approved as a first-line TB drug in most countries. If you need an alternative to rifampin, your doctor may consider extending treatment duration with other drugs, but this is complex and not always feasible.
Why do some people on DOACs and rifampin still not have clots?
Individual metabolism varies. Some people naturally have higher baseline levels of drug-metabolizing enzymes, so rifampin doesn’t push them as far. Others may take their DOAC at a different time of day, have different liver function, or be on lower doses. But this is luck, not safety. A 2023 study of over 2,000 patients showed that even those who didn’t have clots still had significantly lower drug levels. The absence of symptoms doesn’t mean the interaction isn’t happening.




Bob Martin
Rifampin turns your liver into a drug-eating monster and nobody tells you until you're six weeks into TB treatment and your INR is below 1.0
Guess what? Your clotting risk just went from "low" to "I should've listened to the pharmacist"
And now you're stuck on heparin shots while your doctor shrugs and says "it's just how it is"
Sage Druce
For anyone on DOACs and now told to switch to daily injections - I know it sucks but hear me out
This isn't about convenience it's about not having a stroke in your 40s
My uncle took rivaroxaban with rifampin because he didn't want needles
He had a PE two weeks later
Don't be him
Tyler Mofield
The pharmacokinetic interaction between rifampin and CYP3A4/CYP2C9 substrates is well documented in the literature
Suboptimal anticoagulation leading to thromboembolic events constitutes a class I clinical risk
Adherence to guideline-directed therapy with LMWH is not optional
It is standard of care
Patrick Dwyer
For patients managing chronic conditions like atrial fibrillation or mechanical valves - this is one of those moments where communication saves lives
Don't assume your PCP knows every drug interaction
Bring this post to your pharmacist
Ask them to run a full med review
And if they seem unsure - get a second opinion
You're not being difficult
You're being smart
Bart Capoen
so like… rifampin basically makes your body ignore your blood thinners?
and no one checks if its working for DOACs?
that’s wild
i had a friend on apixaban and got rifampin for a sinus infection
she just kept taking it and said she felt fine
turns out her drug levels were half of what they should’ve been
she didn’t clot… but she also didn’t know she was playing russian roulette
luna dream
They don’t want you to know this
Big Pharma made DOACs so you’d stop checking INR
So you’d stop going to the doctor
So they could sell more pills
And now when rifampin comes along - your body’s not even allowed to warn you
It’s all part of the control system
They don’t care if you clot
They care if you keep buying
Linda Patterson
Americans think they can just pop pills and nothing bad happens
Meanwhile in Germany they have protocols for this
In Japan they monitor drug levels daily
But here? You get a 30 second chat with a doctor who says "just take it"
That’s why we’re dying from preventable interactions
Stop being lazy and educate yourself
Jen Taylor
I just want to say - thank you for writing this so clearly.
As a nurse who’s had to explain this to three patients in the last month - I’ve been begging for a resource like this.
One patient cried because she didn’t know she was at risk.
Another thought her DOAC was "safer" so it couldn’t be affected.
Now I’m printing this out and handing it to every patient starting rifampin.
You’ve made my job easier - and maybe saved lives.
Thank you.
Really.
Thank you.
Shilah Lala
So what you're saying is… the entire medical system is just a giant game of whack-a-mole with liver enzymes?
One drug works until another drug comes along and turns your body into a drug-sucking black hole?
And the only solution is to inject yourself with chemicals every day?
Wow.
Just… wow.
Who designed this circus?