Genetic Drug Response: How Your Genes Affect Medication Effectiveness
When you take a pill, your body doesn’t just absorb it—it genetic drug response, how your unique DNA influences how your body processes and reacts to medications. Also known as pharmacogenomics, it explains why one person takes the same antidepressant as another and feels better, while someone else gets dizzy, nauseous, or worse. This isn’t luck. It’s biology. Your liver enzymes, transport proteins, and receptor sites are all coded by genes—and small differences in those genes change how fast drugs break down, how strong the effect is, or even if they work at all.
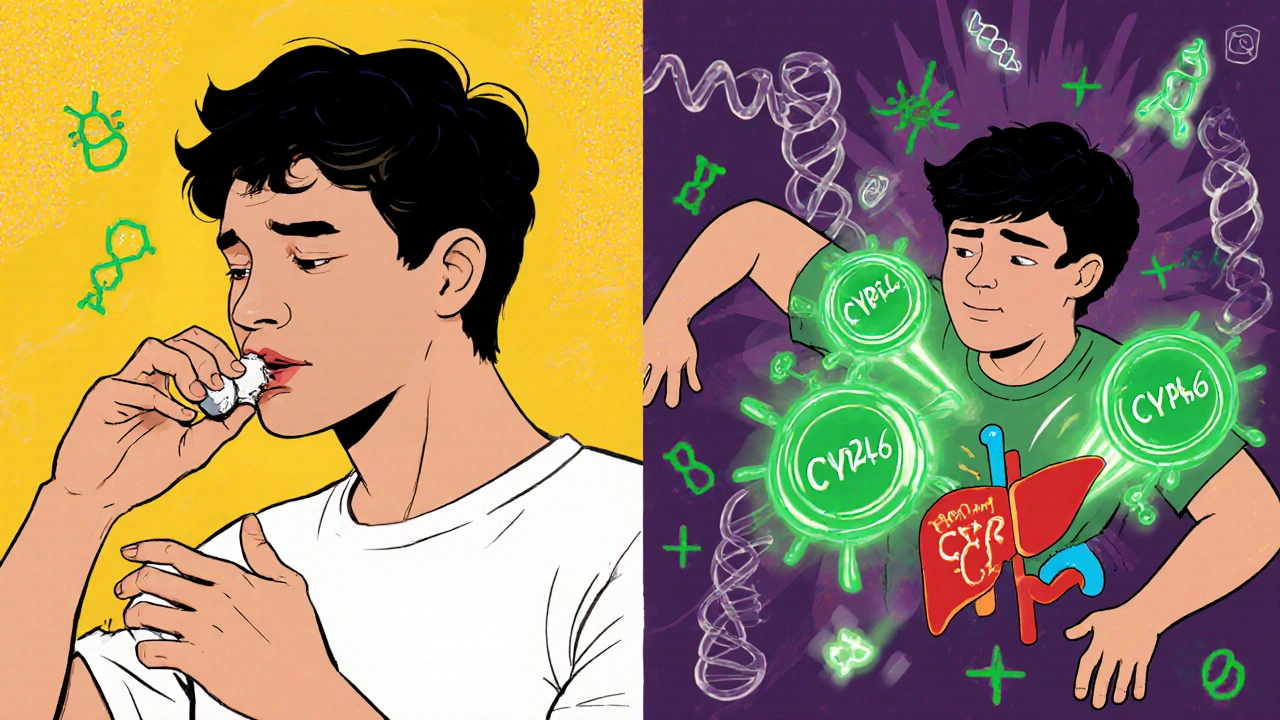
Take warfarin, a blood thinner prescribed to prevent clots. Two people on the same dose can have wildly different outcomes: one stays safe, another bleeds internally. Why? Variations in the CYP2C9 and VKORC1 genes control how quickly warfarin is metabolized. Same drug. Same dose. Totally different results. That’s why doctors are starting to test for these gene variants before prescribing. It’s not sci-fi—it’s becoming standard for heart meds, painkillers, and even some cancer drugs.
Then there’s CYP2D6, a liver enzyme that handles over 25% of common medications. Some people have extra copies of this gene and break down drugs like codeine or antidepressants way too fast—meaning the drug doesn’t work. Others have a broken version and turn codeine into morphine too slowly, or too much, risking overdose. This is why some people say, "I took that painkiller and felt nothing," while others say, "I felt like I was drugged." It’s not about tolerance. It’s about your DNA.
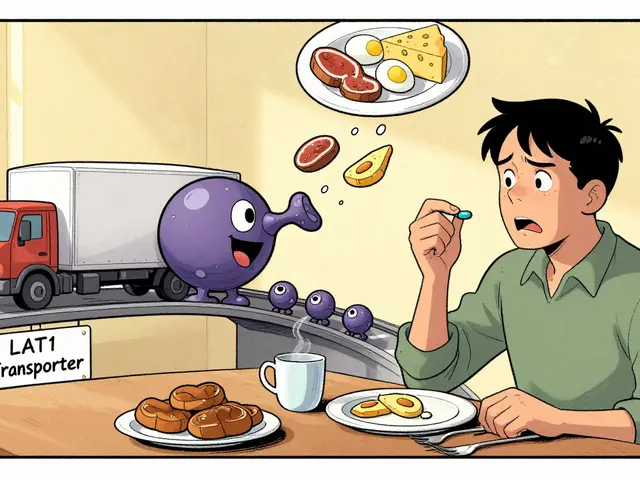
And it’s not just about side effects. Genetic drug response affects everything from asthma inhalers to cholesterol meds. If you’ve ever switched from a brand-name drug to a generic and noticed your symptoms changed, it might not be the filler ingredients—it could be your genes reacting differently to slight variations in how the drug is absorbed. That’s why pediatric switches, statin muscle pain, and antidepressant choices all tie back to this same core idea: your genes are the missing piece in your prescription.
What you’ll find in the posts below isn’t just a list of articles—it’s a map of how this science shows up in real life. From rifampin lowering anticoagulant levels to how sedating meds increase fall risk in older adults, every post connects back to one truth: medicine isn’t one-size-fits-all because people aren’t one-size-fits-all. Your genes? They’re the reason why.