When your child has asthma, the right medication can make all the difference. But if the inhaler isn’t used correctly, that medication might as well be wasted. Studies show that asthma inhaler technique for kids under 8 is often done wrong - and that’s why so many children still struggle with symptoms, even when they’re on daily treatment. The truth? It’s not the medicine that’s failing. It’s the method.
Most kids can’t coordinate pressing the inhaler and breathing in at the same time. That’s where a spacer with a face mask comes in. It’s not optional. It’s essential. Without it, only 10-20% of the medicine reaches the lungs. With proper technique, that jumps to 70-90%. That’s the difference between a child who can play soccer and one who can’t even run to the swings without wheezing.
Why a Spacer and Mask Are Non-Negotiable
A metered-dose inhaler (MDI) sprays medicine as a fine mist. But kids - especially those under 5 - don’t have the timing or lung strength to catch it. They might breathe in too early, too late, or not deep enough. The result? Medicine sticks to the mouth and throat. It doesn’t reach the lungs where it’s needed. That’s why the American Lung Association, Johns Hopkins, and the Global Initiative for Asthma all say the same thing: for children under 8, always use a spacer with a face mask.
A spacer is a plastic tube that holds the medicine after it’s sprayed. The mask fits snugly over the nose and mouth. When you press the inhaler, the medicine sits in the spacer. Your child then breathes in slowly, naturally, over several breaths. No timing needed. No pressure. Just breath.
Studies confirm this works. One 2022 trial found that kids using a spacer with a mask delivered 78.3% of the medicine to their lungs. Those without? Only 12.7%. That’s a six-fold difference. And it’s not just theory - real kids in real homes see fewer emergency visits, fewer missed school days, and better sleep when technique is right.
Step-by-Step: How to Use an Inhaler with Spacer and Mask
Here’s the exact process, broken down into simple steps. Do this every single time - even if your child seems fine. Consistency is what keeps asthma under control.
- Shake the inhaler. Shake it hard for 5-10 seconds. Don’t skip this. The medicine settles. If you don’t shake it, you might get a weak puff or none at all.
- Attach the inhaler to the spacer. Push the metal canister firmly into the rubber end of the spacer. Make sure it’s secure. A loose connection leaks medicine.
- Place the mask on your child’s face. Press it gently but firmly over their nose and mouth. The edge should sit from the bridge of the nose to just below the chin. No gaps. No wrinkles. If you can see their cheeks puffing out, the seal is bad.
- Press the inhaler once. One click. One puff. Don’t press more than once at a time. Wait for the next puff.
- Let your child breathe normally. For infants and toddlers (under 3), have them take 5-10 slow, quiet breaths. Don’t force deep breaths. Just let them breathe like they normally do. For preschoolers (3-8), 6 breaths is enough. Watch the valve in the spacer move - that means they’re breathing in the medicine.
- Wait 30-60 seconds. Don’t rush. Let the medicine settle. If your child coughs or sneezes, start over. The medicine doesn’t stick if they move too soon.
- If a second puff is needed, wait 1-3 minutes. Never give two puffs back-to-back. Wait at least a full minute. For some medications, like corticosteroids, waiting 3 minutes is better. Always check your doctor’s instructions.
- Remove the mask and clean your child’s face. Wipe their mouth and chin with a damp cloth. This prevents rash and mouth thrush, especially with steroid inhalers.
- Wash the spacer once a week. Use warm water and a drop of mild dish soap. Don’t scrub. Don’t towel dry. Just let it air dry upside down. Static builds up in plastic spacers - and static kills medicine delivery. Washing removes it. Some brands say you don’t need to wash, but research shows washed spacers deliver 28% more medicine.
Age Matters: What Changes as Your Child Grows
There’s no one-size-fits-all. What works for a 2-year-old won’t work for a 7-year-old.
Under 3 years: Always use the mask. Tidal breathing (5-10 normal breaths) is best. Your child doesn’t need to hold their breath. Just let them breathe naturally. Use a spacer with a volume of 150-500 mL. Too big? It’s harder to hold the seal. Too small? The medicine doesn’t stay long enough.
3 to 5 years: Still use the mask. You can start practicing single-breath technique: have them take one big breath in, hold for 5 seconds, then breathe out. But don’t force it. If they resist, go back to tidal breathing. Many kids this age still can’t hold their breath long enough.
5 to 8 years: This is the transition window. Some kids can switch to the mouthpiece - no mask. But only if they can seal their lips tightly around the spacer and take one deep breath, hold it for 10 seconds, then breathe out. If they puff out their cheeks or leak air, go back to the mask. Don’t rush this. A 2023 study found kids over 5 using a mouthpiece delivered 68.9% of medicine - but only if they did it right. If they didn’t, it was worse than using a mask.
Once your child is 8 or older, most doctors will move them to a mouthpiece without a spacer - but only if they’ve shown they can use it correctly. Many teens still need spacers. Don’t assume they’re ready just because they’re older.

Common Mistakes (And How to Fix Them)
Parents make the same errors over and over. Here are the top five - and how to avoid them.
- Not shaking the inhaler. 42.7% of parents skip this. Shake it like you’re trying to get the last drop out. Ten seconds. No excuses.
- Bad mask seal. This happens in over 60% of attempts. The mask must cover the nose and chin without pressing into the cheeks. Use your fingers to press the edges down. If you can see light around the edges, it’s not sealed.
- Too many puffs at once. Pressing the inhaler twice before your child finishes breathing means half the medicine is lost. One puff. Wait. Then the next.
- Not washing the spacer. Static charge builds up after just a few uses. It grabs the medicine like a magnet. Wash it weekly. Air dry. No towels.
- Using the wrong mask size. A mask too big covers the eyes. Too small doesn’t seal. Measure: it should go from the bridge of the nose to the bottom of the chin. No overlap on the cheeks. Most brands have sizing guides on the box.
What to Do When Your Child Resists
Most kids hate the mask. It feels strange. It’s cold. It blocks their face. Resistance is normal. But it’s not a reason to skip treatment.
Here’s what works:
- Use a mask with their favorite character. 57% of parents report success when the mask has Spider-Man, Elsa, or Paw Patrol on it.
- Turn it into a game. Say, “Let’s blow out birthday candles!” before you give the puff. That gets them to exhale fully - which makes room for the medicine. Or, “Can you make the spacer whistle?” (Some spacers make a sound when you breathe in.)
- Practice without medicine. Do a dry run. Put the mask on their face. Let them hold the spacer. Let them press the inhaler (without the canister). Make it fun. No pressure.
- Let them help. Give them the spacer to hold. Let them put the mask on your face first. Kids feel in control when they’re part of the process.
- Stay calm. If you’re frustrated, they feel it. Take a breath. Wait. Try again later.
One parent on a pediatric asthma forum said: “We tried the ‘blow out candles’ trick. My 2-year-old started doing it on his own. Now he asks for his ‘candle game’ before we give his medicine.” That’s the goal.
When to Call the Doctor
Even with perfect technique, asthma can flare up. But if your child’s symptoms aren’t improving - or they’re getting worse - it’s not always because the medicine isn’t strong enough. It might be technique.
Call your pediatrician or asthma specialist if:
- Your child needs their rescue inhaler more than twice a week (not counting exercise).
- They wake up at night because of coughing or wheezing.
- They’re using more puffs than prescribed.
- You’re unsure if you’re doing it right.
Doctors can watch you do it. Many now offer video visits where you show them your technique. A 2023 study showed that when parents submitted videos of their inhaler use, emergency visits dropped by 47%. That’s huge.
And if your child has been labeled “steroid-resistant” - stop. That’s often just bad technique. One study found 68% of kids thought to be resistant were actually just using the inhaler wrong.
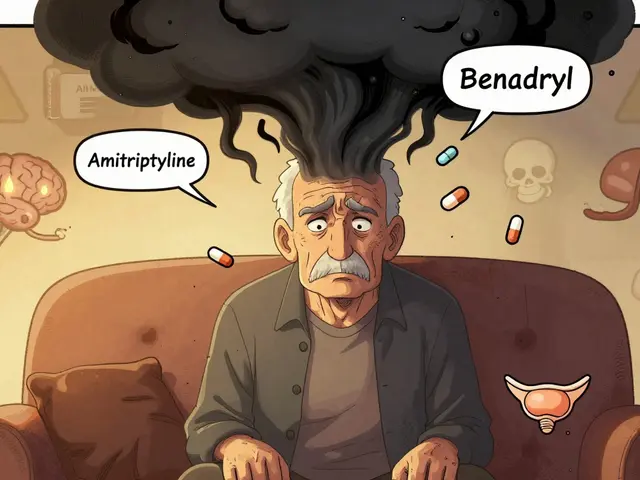
What’s New in 2025
Technology is helping. Smart spacers are now FDA-approved. These devices have sensors that listen to your child’s breathing and give audio feedback - like “Breathe slower” or “Good job!” - through a small speaker. One model, the Halo system, showed a 32% improvement in technique after just 4 weeks of use.
More clinics are using video coaching. You record yourself giving the inhaler, send it to your provider, and they give you feedback. No in-person visit needed. This is becoming standard in 2025.
But here’s the bottom line: none of this matters if you don’t do the basics right. No smart spacer replaces shaking the inhaler. No app replaces a good mask seal.
Final Tip: Keep a Technique Log
Write down when you give the inhaler. Note if your child coughed, if the mask slipped, if you washed the spacer this week. After a month, you’ll see patterns. Maybe you forget to shake it on weekends. Maybe your child only resists in the morning. That’s data. And data helps you fix the problem.
Asthma doesn’t have to control your child’s life. But it takes more than a prescription. It takes practice. Patience. And perfect technique.
Can my child use an inhaler without a spacer?
For children under 8, no - not reliably. Without a spacer and mask, less than 20% of the medicine reaches the lungs. Even older kids often need a spacer if they can’t coordinate breathing with the puff. If your child is over 8 and can seal their lips tightly around a mouthpiece, take one deep breath, and hold it for 10 seconds, they may switch. But always check with your doctor first.
How often should I wash the spacer?
Once a week. Use warm water and a drop of mild dish soap. Don’t scrub or use a towel. Let it air dry upside down. Static builds up in plastic spacers and blocks medicine delivery. Washing removes it. Some brands say you don’t need to wash, but studies show washed spacers deliver nearly 30% more medicine.
My child cries when I put the mask on. What do I do?
Resistance is normal. Try these: use a mask with their favorite character, practice without medicine, turn it into a game like “blow out birthday candles,” or let them hold the spacer and press the puff themselves. Stay calm. Don’t force it. Try again later. Many kids adjust within a few days with consistent, gentle practice.
Is it okay to use a spacer with a dry powder inhaler?
No. Dry powder inhalers (like Diskus or Twisthaler) require a strong, fast breath to pull the powder into the lungs. Spacers slow down airflow, so the powder won’t reach the lungs. These are only for older children and adults who can inhale forcefully. If your child is under 8, they’ll need a metered-dose inhaler with a spacer - not a dry powder one.
How do I know if the mask fits right?
The mask should cover the nose and mouth, with the bottom edge resting just below the chin. It should not overlap the cheeks or press into the eyes. If you can see light around the edges, or if your child’s cheeks puff out when they breathe, the seal is bad. Most spacer brands include a sizing guide - use it. A mask that’s too big or too small won’t work.
Can I use a homemade spacer, like a bottle?
Yes - but only as a last resort. Doctors have used cut plastic bottles as spacers in emergencies. But they’re not tested for safety or delivery efficiency. A proper spacer is designed to hold the right amount of medicine and reduce static. If you’re using a bottle, it’s because you can’t get a real one. Get a proper spacer as soon as possible. A 2023 study showed even a washed plastic bottle could deliver 80% of medicine - but only if the seal was perfect. Don’t rely on it long-term.



Sakthi s
This is the kind of info every parent needs. My kid was wheezing every week until we started using the spacer with the mask. No more ER visits. Just calm breaths and a little game time. Seriously, do the 5 breaths. It works.
Victor T. Johnson
They say its the technique but what if its the medicine itself? Who controls the pharmaceutical supply chain? Why are spacers so expensive when a plastic bottle works just fine? 🤔 Maybe the system wants you dependent on overpriced gear. I used a cut 2L bottle for 3 months. My kid breathed better. Coincidence? I think not. 🧪
Julia Jakob
lol i totally forgot to shake the inhaler for like 6 months. thought i was being efficient. turns out my kid was just getting a puff of air and a taste of chemicals. now i shake it like im trying to wake up a sleeping bear. 10 seconds. no excuses. 🙃
Robert Altmannshofer
Man, this post is gold. I’ve been a pediatric nurse for 12 years and I still see parents skipping step 1 - shaking. It’s wild. And the mask seal? So many moms and dads press it like they’re trying to smother a pillow. Gently. Just gently. And yeah, the character masks? Total game-changer. My niece asked for ‘Paw Patrol’ last week and cried when we didn’t have it. She’s 4. We’re all just trying to keep them breathing. Thank you for laying this out so clearly.
Sophia Lyateva
smart spacers? really? they’re listening to my kid’s breathing? who’s got access to that data? next they’ll be tracking how often we wash the spacer and sending it to insurance companies. i’m not letting some algorithm judge my parenting just because i forgot to air dry it once. this feels like surveillance in a mask
Kathleen Koopman
Wait so dry powder inhalers don’t work with spacers?? I’ve been using one for my 6-year-old because it looked ‘easier’ 😅 I’m gonna switch back to the MDI with spacer ASAP. Thanks for the clarity! 🙏
Rachel Nimmons
I’ve been using the same spacer for 2 years. Never washed it. Just wiped it with a tissue. My kid’s asthma hasn’t changed. Maybe it’s not the technique. Maybe it’s the medicine. Or the air. Or the schools. Or the vaccines. I don’t know anymore.
AARON HERNANDEZ ZAVALA
My daughter used to hate the mask. Then we got one with Elsa. Now she puts it on herself and says ‘I’m ready for my magic breath’ 🤍 I didn’t think it’d work but… it did. Just remember: patience. Not perfection. You’re doing better than you think.