For many people, a stuffy nose that won’t go away isn’t just annoying-it’s exhausting. If you’ve had nasal congestion, facial pressure, or a lost sense of smell for more than three months, despite trying decongestants or antibiotics, you might be dealing with chronic sinusitis. Unlike a regular cold or acute sinus infection that clears up in a couple of weeks, chronic sinusitis lingers. And it’s not just about being congested. It can mess with your sleep, your focus, even your mood. The good news? We know more now than ever about what causes it and how to treat it effectively.
What Exactly Is Chronic Sinusitis?
Chronic sinusitis, also called chronic rhinosinusitis, isn’t one single problem. It’s a group of conditions where the lining of your sinuses-those hollow spaces around your nose, eyes, and forehead-stays swollen and inflamed for 12 weeks or longer, even with treatment. The key difference from acute sinusitis? It doesn’t just flare up and disappear. It sticks around. According to the European Position Paper on Rhinosinusitis and Nasal Polyps (EPOS) 2020, you likely have it if you’re dealing with at least two of these symptoms for more than three months: blocked nose, thick nasal discharge (front or back), facial pain or pressure, and trouble smelling things.
Doctors don’t always know the exact trigger, but they’ve figured out the main players: inflammation, structural blockages, and immune responses. It’s rarely just a bacterial infection, even though many people assume it is. In fact, about 70% of chronic cases have little to no active bacteria involved. Instead, it’s your body’s own immune system overreacting-often because of allergies, polyps, or environmental irritants like smoke or pollution.
The Three Main Types
Chronic sinusitis isn’t one-size-fits-all. There are three main subtypes, and knowing which one you have changes your treatment plan.
- Chronic sinusitis without nasal polyps: This is the most common form. Symptoms are persistent congestion, discharge, and pressure, but no visible growths in the nasal passages.
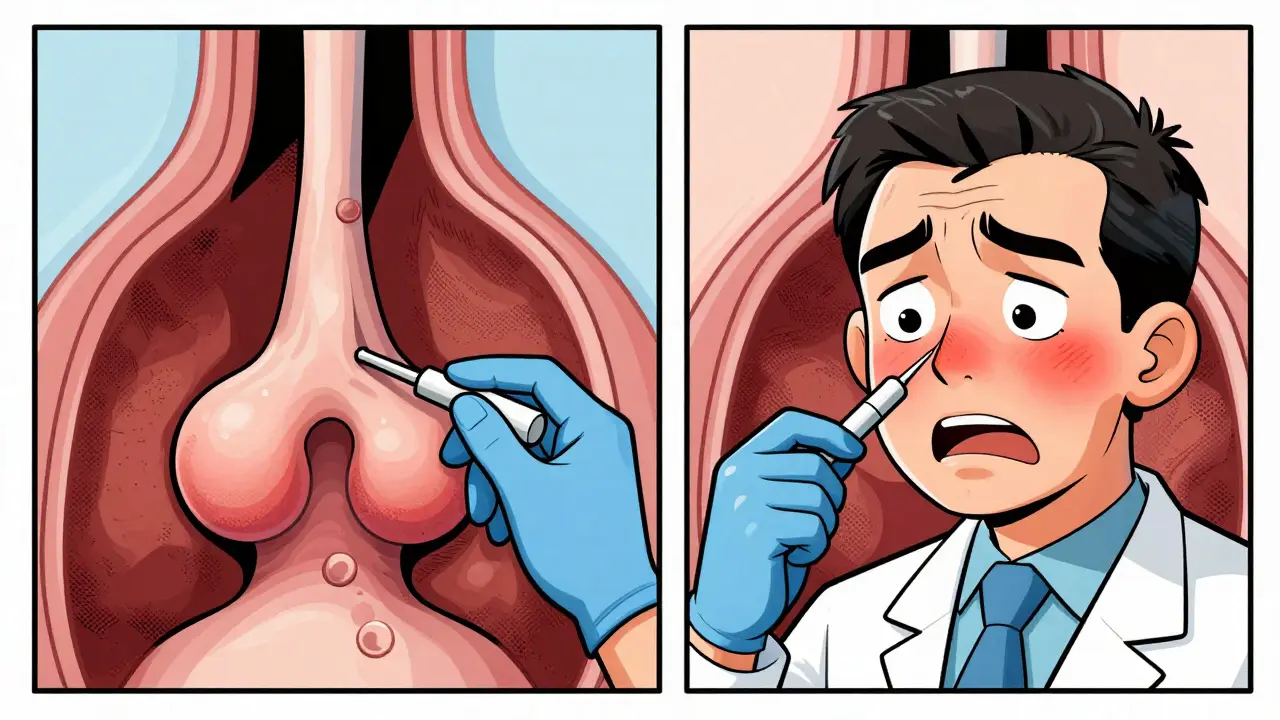
- Chronic sinusitis with nasal polyps: About one in four people with chronic sinusitis have these soft, noncancerous growths inside the nose. They’re like tiny balloons of swollen tissue that block airflow and mucus flow. People with this type often also have asthma or sensitivity to aspirin.
- Allergic fungal rhinosinusitis: This happens when your immune system reacts strongly to common fungi in the air, especially in humid climates. It’s less common but often more stubborn. You’ll typically see thick, sticky mucus and sometimes dark fungal debris in the sinuses.
Doctors use nasal endoscopy or a CT scan to tell them apart. That’s why getting a proper diagnosis matters-treating polyps the same way you’d treat simple inflammation won’t work.
What Triggers It? Allergies, Irritants, and More
Allergies are a major driver. If you have hay fever, dust mite allergies, or pet dander sensitivity, your risk of chronic sinusitis jumps by 2.5 times. Why? Because allergic reactions make the nasal lining swell and produce excess mucus, which then gets trapped. Over time, this leads to chronic inflammation.
Asthma is another big link. People with asthma are three to four times more likely to develop chronic sinusitis. The same inflammatory pathways that cause wheezing also affect the sinuses. This is why many patients need care from both an allergist and an ENT specialist.
Environmental irritants play a role too. Smoking or being around secondhand smoke increases your risk by 35%. Air pollution, strong perfumes, and even dry indoor air from heating systems can keep the sinuses irritated. In places like Perth, where summer heat and low humidity are common, dry sinuses become a real issue. That’s why many patients find relief just by using a humidifier at night.
And then there’s anatomy. A deviated septum, narrow sinus openings, or even a history of nasal trauma can physically block drainage. These structural issues don’t go away on their own-and they make medical treatments less effective.
First-Line Treatment: It’s Not What You Think
Most people reach for antibiotics when their nose won’t clear up. But that’s usually the wrong move. The American Academy of Allergy, Asthma & Immunology says antibiotics rarely help in chronic cases because bacteria aren’t the main problem.
The real first step? Nasal saline irrigation and intranasal corticosteroid sprays. These aren’t flashy, but they work. Saline rinses flush out mucus, allergens, and irritants. Corticosteroid sprays like fluticasone (Flonase), mometasone (Nasonex), or budesonide (Rhinocort) calm down the inflammation deep in the nasal lining.
Studies show 60-70% of patients see improvement with these two tools alone. But here’s the catch: you have to use them every day, for weeks. Many people stop after a few days because they don’t feel immediate results. That’s why adherence is such a problem-only about 60% of patients stick with it long enough to benefit.
If allergies are the main cause, antihistamines like loratadine or cetirizine can help reduce sneezing and runny nose. But they don’t fix the swelling. That’s why they’re usually paired with steroid sprays, not used alone.
When Medication Isn’t Enough: Biologics and New Hope
If you’ve tried nasal sprays for 12 weeks and still feel blocked, smelly, or constantly congested, you might be a candidate for biologic therapies. These are newer, targeted injections that stop specific parts of the immune system from overreacting.
Dupilumab (Dupixent) was approved by the FDA in 2019 specifically for chronic sinusitis with nasal polyps. In clinical trials, it cut polyp size by 50-60% and improved breathing and smell in 30-40% of patients. It’s not a cure, but for many, it’s life-changing. Other biologics like omalizumab (Xolair) and mepolizumab (Nucala) also help, especially for those with severe asthma and polyps.
There’s also aspirin desensitization for the small group with Samter’s triad-asthma, nasal polyps, and aspirin sensitivity. After controlled exposure to aspirin under medical supervision, 70-80% of these patients see major symptom reduction. It’s not for everyone, but for those who qualify, it’s one of the most effective long-term options.
Emerging research is looking at probiotics and microbiome therapy. Early studies at Johns Hopkins suggest certain good bacteria may help reduce inflammation in the sinuses. While not standard yet, it’s a promising direction.
Surgery: When It’s Time to Consider It
Surgery isn’t the first option-but it’s often the right one when medical treatment fails. The gold standard is functional endoscopic sinus surgery (FESS). It’s minimally invasive. An ENT uses a thin camera and tiny tools to open blocked sinus passages and remove polyps or scar tissue. No external cuts. No overnight stay.
Success rates? Between 75% and 90% of patients report better breathing and fewer infections after FESS. Recovery is usually quick-most people are back to normal in 7-10 days. But surgery doesn’t fix the root cause. If allergies or inflammation continue, polyps can come back. That’s why surgery is almost always followed by ongoing steroid sprays and saline rinses.
For some, a less invasive option called balloon sinuplasty works. A tiny balloon is inflated inside the blocked sinus to widen it. Recovery is faster-often just 3-5 days. But it’s not as effective for severe polyps or complex blockages. It’s better for mild to moderate cases.
If you have a deviated septum, your doctor might combine FESS with a septoplasty. That fixes the crooked cartilage that’s blocking airflow. Studies show 65-75% of patients get major relief when both are done together.

Long-Term Management: It’s a Lifestyle
Chronic sinusitis rarely goes away completely. But it can be managed well. The goal isn’t to be symptom-free every day-it’s to reduce flare-ups and keep your quality of life high.
- Use a saline rinse daily-morning or night, whichever works for you.
- Keep your home humidified, especially in winter or dry climates.
- Avoid smoke, strong chemicals, and known allergens.
- Stay hydrated. Thick mucus is harder to clear.
- Stick with your steroid spray, even when you feel fine.
- See your allergist regularly. Allergy testing can reveal hidden triggers.
And don’t ignore the mental toll. Constant congestion, fatigue, and trouble sleeping can lead to anxiety or depression. Talk to your doctor if you’re feeling down. Chronic illness isn’t just physical-it’s emotional too.
What Happens If You Ignore It?
Most people won’t develop serious complications. But untreated chronic sinusitis can lead to infections spreading to the eyes, bones, or even the brain-though this happens in less than 0.5% of cases. More commonly, it just wears you down. You stop sleeping well. You lose your sense of taste and smell. You avoid social events because you’re always congested. You feel tired all the time.
That’s why early, consistent care matters. Waiting for it to get worse only makes treatment harder.
When to See a Specialist
If you’ve had symptoms for more than 12 weeks, or if your symptoms keep coming back after antibiotics, it’s time to see an ENT or allergist. Primary care doctors can start treatment, but specialists have the tools and experience to find the real cause.
Ask for a nasal endoscopy. Ask about allergy testing. Ask if you have polyps. Don’t settle for “just a bad cold.” You deserve better.



Rich Robertson
Been dealing with this for years. Saline rinses saved my life. I used to think antibiotics were the answer, but nope. Just kept making it worse. Started doing twice-daily rinses with a neti pot and a steroid spray - took about 6 weeks, but now I can actually sleep through the night. No more 3 a.m. head pressure. Best decision I ever made.
Sarthak Jain
bro i had this for 4 yrs n thought it was just allergies… turns out i had polyps n didnt even know it. doc did endoscopy n was like ‘yo these are huge’. got dupixent last year and my sense of smell came back like magic. i could smell coffee again lmao. also stopped eating dairy, weirdly helped too. idk if it’s placebo but i feel 10x better.
Daniel Thompson
While I appreciate the clinical overview presented, I must emphasize that the medical establishment’s overreliance on pharmacological interventions continues to obscure the root causes of chronic inflammation. The systemic dysbiosis hypothesis, particularly regarding the sinonasal microbiome, remains underexplored in mainstream protocols. Pharmaceutical companies have a vested interest in maintaining the status quo.
Daniel Wevik
Let me tell you something - if you’re still taking antibiotics for chronic sinusitis, you’re wasting time and money. The science is crystal clear: it’s inflammation, not infection. Saline irrigation + steroid spray is the gold standard. No fluff. No hype. Just do it daily. And if you’re not seeing results after 12 weeks, see a specialist. Don’t wait until you’re breathing through your mouth at night.
Natalie Koeber
They don’t want you to know this, but the FDA approved dupixent because Big Pharma made a deal with the WHO to replace natural remedies with expensive biologics. Your sinuses are meant to drain naturally - humidifiers, steam, and garlic oil have been used for centuries. Now they want you on monthly injections costing $30,000 a year. Wake up.
Rulich Pretorius
This is one of the most balanced, human takes on chronic sinusitis I’ve read. So many people suffer in silence thinking it’s just ‘bad allergies.’ The emotional toll is real - I lost my job because I was too tired to focus. What helped me most? Consistency. Not magic. Just rinses, sprays, and avoiding smoke. And yes - the smell came back slowly. Took 8 months. But it came. You’re not broken. You just need the right approach.
Thomas Anderson
Just started the saline rinse. It burns at first, but after a week I can actually breathe through my nose. No more waking up with my mouth dry. I used to think it was just me being lazy, but turns out I just didn’t know how to treat it. This post is legit.
Wade Mercer
People these days are too lazy to just ‘get over it.’ If you can’t handle a little congestion, maybe you’re just out of shape. I’ve never used a neti pot in my life and I’m 52. Stop treating your sinuses like they’re fragile glass. Just toughen up.
Dwayne hiers
For those considering biologics: dupilumab targets IL-4/IL-13 pathways, which are central to type 2 inflammation - the dominant endotype in polyp-associated CRSwNP. Response rates correlate with elevated blood eosinophils and IgE levels. Pre-treatment biomarker profiling is critical. FESS + post-op steroid irrigation remains the cornerstone, but biologics are transforming outcomes in refractory cases. Don’t delay referral if you’re failing medical therapy.
Jonny Moran
For anyone reading this and thinking ‘I can’t do this every day’ - you’re not alone. I skipped for weeks. Then I’d get sick again. So I set a daily alarm labeled ‘Nose Time.’ 3 minutes. That’s it. Now it’s part of my routine, like brushing my teeth. You don’t need to be perfect. Just show up. Your sinuses will thank you.
Tim Bartik
Y’all are so soft. Back in my day, we just sucked it up. Now everyone’s got a neti pot and a biologic injection. This is why America’s falling apart. If you can’t breathe through your nose, maybe you’re just fat. Go outside. Get some sun. Stop being a medical zombie. Also, fluoride in the water is why your sinuses are messed up. I know.