Euglycemic DKA Risk Assessment Tool
This tool helps assess your risk of euglycemic DKA when taking SGLT2 inhibitors (like Farxiga, Jardiance, Invokana). Remember: normal blood sugar doesn't mean you're safe. If you experience symptoms, check ketones immediately.
Symptom Assessment
Most doctors still think diabetic ketoacidosis (DKA) means high blood sugar. That’s the old rule. But if you’re taking an SGLT2 inhibitor-like Farxiga, Jardiance, or Invokana-and you feel sick, your blood sugar might be normal. And that’s when things get dangerous.
Euglycemic DKA isn’t rare. It’s hiding in plain sight. About 1 in 3 cases of DKA in people on these drugs happens with blood glucose under 250 mg/dL. That’s not a fluke. It’s a pattern. And it’s killing people because no one checks ketones when the glucose reading looks fine.
What Is Euglycemic DKA?
Euglycemic DKA is diabetic ketoacidosis without the high blood sugar. You still get acidosis-your blood gets too acidic. Your body still floods with ketones. But your glucose stays between 100 and 250 mg/dL. Normal range. So you, your family, even your doctor, might think you’re okay.
This isn’t theoretical. In 2015, the FDA issued a warning after 13 cases were found in U.S. clinics. Nine patients. Thirteen episodes. All on SGLT2 inhibitors. Seven had type 1 diabetes. Two had type 2. None had blood sugar above 250 mg/dL. That’s when the medical world had to change its playbook.
The problem? SGLT2 inhibitors make your kidneys flush out glucose. That lowers blood sugar. But it also tricks your body into thinking it’s starving. Your pancreas releases more glucagon. Your fat breaks down. Ketones pile up. And you’re in DKA-even if your glucose looks perfect.
Why SGLT2 Inhibitors Trigger This
SGLT2 inhibitors were designed to help type 2 diabetes by making you pee out sugar. They work. They reduce heart failure risk. They help with weight. But they also mess with your body’s fuel balance.
Here’s how it breaks down:
- You take the drug → glucose leaves through urine → blood sugar drops
- Your body thinks it’s low on fuel → glucagon rises, insulin drops
- Fat gets broken down → ketones flood your blood
- Acid builds up → metabolic acidosis sets in
Even if you’re eating normally, your liver can’t make enough glucose to keep up. The drug blocks the backup system. That’s why you can get DKA without ever being hyperglycemic.
And it’s not just people with type 1 diabetes. About 20% of cases happen in people with type 2 who’ve never had DKA before. That’s the scary part. You think you’re safe because you’re not insulin-dependent. You’re wrong.
Signs You’re in Trouble
These symptoms don’t care about your glucose meter.
- Nausea (85% of cases)
- Vomiting (78%)
- Abdominal pain (65%)
- Deep, fast breathing (Kussmaul respirations, 62%)
- Extreme fatigue (76%)
- General malaise (91%)
You might feel like you have the flu. Or food poisoning. Or a bad stomach bug. But if you’re on an SGLT2 inhibitor and you’re feeling this way, don’t wait. Don’t assume it’s just a virus. Don’t check your glucose and breathe easy because it’s 180 mg/dL.
That’s the trap. The glucose is normal. So you think, “It’s not DKA.” But DKA doesn’t need high sugar anymore. That rule is dead.
And no, you can’t rely on fruity breath. Some people have it. Many don’t. It’s not a reliable sign. Only ketone testing tells the truth.
How Doctors Miss It
Emergency rooms across the U.S. still use glucose as the gatekeeper for DKA. If it’s under 250, they don’t test ketones. They don’t check anion gap. They don’t look at bicarbonate.
A 2015 study in Diabetes Care showed that in every single case of SGLT2-related euglycemic DKA, treatment was delayed because doctors trusted the glucose reading. One patient died. Another had a cardiac arrest. All because no one thought to check ketones.
The FDA’s 2015 warning said it plainly: “Ketoacidosis can occur with blood glucose levels below 250 mg/dL.” But that warning hasn’t fully reached every ER, every clinic, every urgent care center.
Dr. Jane Jeffrie, who led the 2015 study, put it bluntly: “The absence of hyperglycemia should never rule out DKA.”
And yet, most providers still don’t test for ketones unless glucose is over 300. That’s outdated. That’s dangerous.

How to Diagnose It
If you’re on an SGLT2 inhibitor and you have nausea, vomiting, or unexplained fatigue, you need three things checked:
- Blood glucose - even if it’s normal
- Serum ketones - beta-hydroxybutyrate, not urine strips
- Arterial blood gas or venous bicarbonate - look for pH under 7.3 or bicarbonate under 18 mEq/L
Urine ketone strips? Useless. They’re slow. They’re inaccurate. They miss early ketosis. Serum beta-hydroxybutyrate is the gold standard. Levels above 3 mmol/L mean you’re in DKA.
Also check your anion gap. If it’s over 12, you’ve got metabolic acidosis. Combine that with ketones and symptoms? You’ve got euglycemic DKA.
Don’t be fooled by high white blood cell counts. That’s not infection. It’s dehydration. It’s stress. It’s the body reacting to acidosis.
Emergency Treatment: What Works
Treatment is similar to classic DKA-but with key differences.
First: fluids. Start with 0.9% saline at 15-20 mL/kg in the first hour. But don’t overdo it. You’re not dehydrated like a classic DKA patient. Your volume status is often better.
Second: insulin. Give 0.1 units/kg/hour. But here’s the twist: start glucose-containing fluids early. In classic DKA, you wait until glucose drops below 250 to add dextrose. In euglycemic DKA, you might need it after the first hour. Your blood sugar can crash fast. You don’t want to go from 180 to 50 in two hours.
Third: potassium. Almost two-thirds of these patients have low total body potassium-even if their blood level looks normal. You’ll need to replace it aggressively. Don’t wait for the lab to show low potassium. Start early.
Fourth: stop the SGLT2 inhibitor. Immediately. Don’t wait. Don’t ask. Just stop it.
And don’t forget: check for other causes. Lactic acidosis, alcohol, sepsis. They can mimic this. But if ketones are high and acidosis is present, treat for DKA first.
Who’s at Highest Risk?
It’s not just type 1 diabetes. Here’s who needs to be extra careful:
- Anyone on SGLT2 inhibitors during illness (infection, flu, COVID-19)
- People who skip meals or eat very little
- Patients preparing for surgery
- Women who are pregnant
- Those who drink alcohol
Even if you’re type 2, have no history of DKA, and feel fine-stop your SGLT2 inhibitor if you get sick. Don’t wait for symptoms. Don’t hope it’ll pass. Just stop.
And if you’re type 1? Off-label use of SGLT2 inhibitors is common. About 8% of type 1 patients are on them. DKA rates in this group? Between 5% and 12%. That’s not low. That’s a ticking clock.
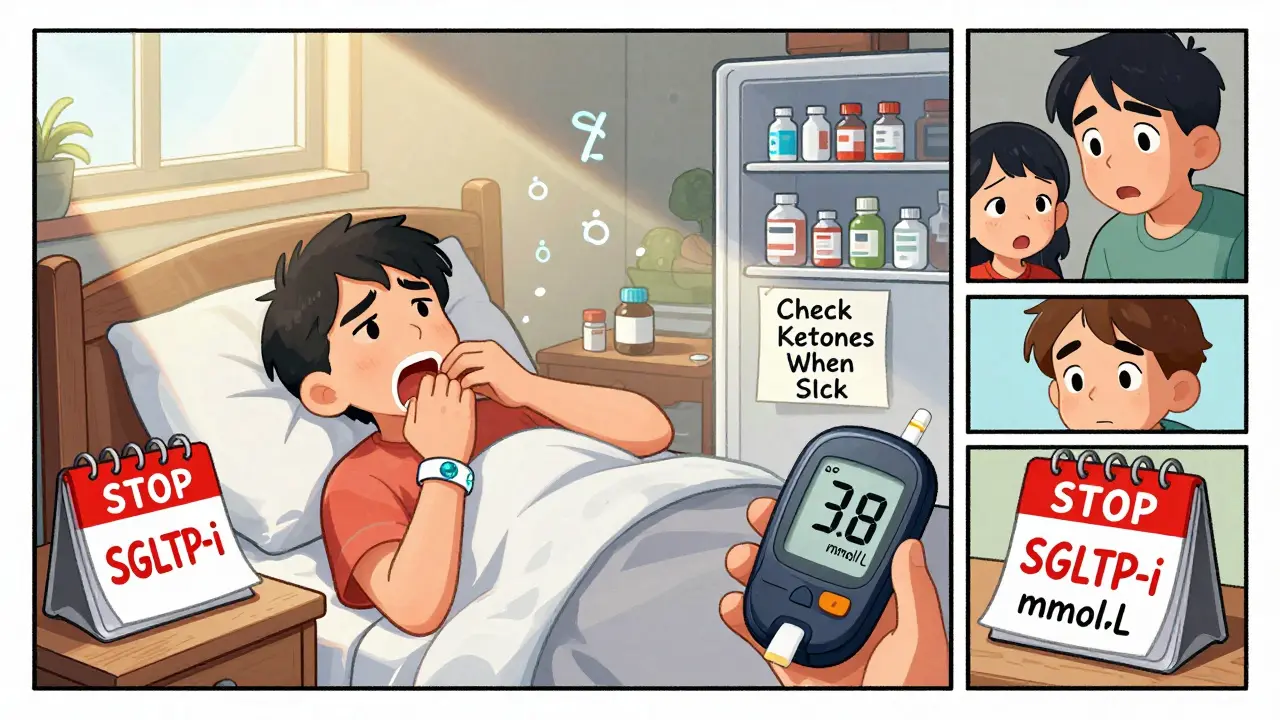
Prevention: What You Need to Do
Prevention is simple. But it’s not taught enough.
- Always check ketones if you’re sick-even if your glucose is normal.
- Stop your SGLT2 inhibitor when you’re ill, fasting, or having surgery.
- Keep eating carbs during stress. Don’t go low-carb to “help your diabetes.” That’s a recipe for disaster.
- Have ketone strips or a meter at home. Know how to use them.
- Tell every doctor you see that you’re on an SGLT2 inhibitor. Write it on your medical alert bracelet.
The FDA requires that every SGLT2 inhibitor package says: “Stop taking this medicine and get medical help right away if you have symptoms of ketoacidosis-even if your blood sugar is normal.”
But if you don’t know what those symptoms are? You won’t stop. You won’t go to the ER. You’ll wait. And that’s how people die.
What’s Changing Now?
Good news: awareness is rising. Since 2015, overall DKA cases on SGLT2 inhibitors have dropped by 32%. But here’s the catch: euglycemic DKA now makes up 41% of all cases-up from 28% in 2015. That means more people are being diagnosed correctly. But the risk hasn’t gone away.
Researchers are testing new tools. A 2023 study found that the ratio of acetoacetate to beta-hydroxybutyrate can predict EDKA 24 hours before symptoms start. That’s huge. But it’s not available yet.
Another project, the SGLT2i-EDKA Prediction Study, is tracking over 1,200 patients. Early results suggest that if your HbA1c swings a lot and your C-peptide is low, you’re at higher risk. That could lead to screening tools in the next few years.
But right now? The only tool you need is your brain. And a ketone meter.
The Bottom Line
SGLT2 inhibitors are powerful drugs. They save lives. But they can kill if you don’t know how they work.
Euglycemic DKA is real. It’s dangerous. And it’s underdiagnosed.
If you’re on one of these drugs, you must know: normal glucose doesn’t mean safe. Ketones don’t care about your meter. They care about your body’s fuel state.
Check ketones when you’re sick. Stop the drug when you’re unwell. Tell your doctors. Don’t wait for the textbook signs. The textbook changed. You have to change with it.
One more thing: if you’re a doctor-don’t assume. Test. Even if the glucose is fine. You might just save a life.
Can you get euglycemic DKA if you have type 2 diabetes?
Yes. About 20% of euglycemic DKA cases occur in people with type 2 diabetes who have never had DKA before. SGLT2 inhibitors are commonly prescribed for type 2 diabetes, and the risk exists regardless of insulin use. Normal blood sugar doesn’t protect you.
Should I stop taking my SGLT2 inhibitor if I get sick?
Yes. If you have an infection, fever, vomiting, surgery, or reduced food intake, stop your SGLT2 inhibitor immediately. Don’t wait for symptoms of DKA. Don’t assume it’s just a stomach bug. Restart only after you’re fully recovered and eating normally.
Are urine ketone strips reliable for detecting euglycemic DKA?
No. Urine strips are slow, inaccurate, and can miss early ketosis. They detect acetoacetate, not beta-hydroxybutyrate-the main ketone in DKA. Serum beta-hydroxybutyrate testing is the only reliable method. Use a blood ketone meter if you’re at risk.
Why do SGLT2 inhibitors cause DKA without high blood sugar?
SGLT2 inhibitors force your kidneys to remove glucose, lowering blood sugar. But this tricks your body into thinking it’s low on fuel. Glucagon rises, insulin drops, and your fat breaks down into ketones. Even with normal glucose, your body is in a starvation-like state, triggering ketoacidosis.
Is euglycemic DKA more dangerous than classic DKA?
It can be. Because it’s missed more often, treatment is delayed. Patients may not seek help. Doctors may not test for ketones. This leads to longer hospital stays, more complications, and higher risk of death. Early recognition is the key to survival.
Can I still take SGLT2 inhibitors if I have type 1 diabetes?
They’re not FDA-approved for type 1 diabetes, but some doctors prescribe them off-label. About 8% of type 1 patients use them. The risk of DKA is 5-12% in this group. If you’re on one, you must be extremely vigilant about ketone checks and never skip insulin. The benefits must outweigh the risks.
What should I do if I suspect euglycemic DKA?
Stop your SGLT2 inhibitor immediately. Test your blood ketones. If they’re above 3 mmol/L or you have symptoms like vomiting, deep breathing, or confusion, go to the ER. Do not wait. Bring your medication list. Tell them you’re on an SGLT2 inhibitor and suspect euglycemic DKA.
For more information, refer to the American Diabetes Association’s 2022 Standards of Medical Care in Diabetes and the FDA’s safety communications on SGLT2 inhibitors. Always consult your healthcare provider before making changes to your medication.





Siobhan K.
Let me be clear: if your doctor still waits for glucose over 250 before checking ketones, they’re operating on a 1998 playbook. This isn’t a debate-it’s a systemic failure. I’ve seen two patients nearly die because their ER didn’t test beta-hydroxybutyrate. One was on Jardiance. Glucose was 190. They sent her home. She came back in cardiac arrest. Stop trusting meters. Start trusting physiology.
Cara C
This is exactly why I carry a blood ketone meter in my purse now. I’m type 2, on Farxiga, and I had a bad stomach bug last winter. Glucose was 170. Felt awful. Thought it was food poisoning. Checked ketones anyway-3.1 mmol/L. Went to urgent care. They laughed. Then they called an endo. Saved my life. If you’re on an SGLT2i, get a meter. It’s cheaper than an ICU stay.
Michael Ochieng
As a med student in Chicago, I’ve seen this twice in the last six months. Both patients were type 2, on Invokana, came in with nausea and fatigue. Glucose normal. Anion gap sky-high. Ketones through the roof. One was a teacher who thought she just had the flu. The other was a construction worker who didn’t want to miss work. Both were admitted. Both had to stop their meds. This isn’t rare. It’s underdiagnosed because we’re still trained to see diabetes as ‘high sugar = bad.’ We need to retrain the whole system.
Meina Taiwo
Stop the drug when sick. Test ketones. Period. No excuses.
Brian Furnell
Let’s dissect the pathophysiology here: SGLT2 inhibition induces a pseudo-starvation state by promoting glucosuria, which suppresses insulin secretion and elevates glucagon via a hypothalamic-sensing mechanism. The resulting lipolysis generates free fatty acids, which undergo β-oxidation in hepatocytes, producing acetyl-CoA that exceeds TCA cycle capacity-hence, ketogenesis. But because renal glucose excretion maintains normoglycemia, the classic hyperglycemic DKA paradigm becomes irrelevant. The real diagnostic failure lies in the reliance on urine ketone strips, which detect acetoacetate, not the dominant ketone body, β-hydroxybutyrate. The latter is the true marker of metabolic derangement. Moreover, the anion gap isn’t just a number-it’s a red flag for unmeasured anions like ketones, lactate, or toxins. If you’re not checking serum β-OHB and venous bicarbonate in any patient on an SGLT2i with GI symptoms, you’re not practicing evidence-based medicine-you’re practicing negligence.
Christina Weber
Someone needs to sue every pharmaceutical company that markets these drugs without a mandatory ketone-testing alert on the prescription label. And why isn’t there a black box warning? This isn’t a side effect-it’s a life-threatening mechanism. I’ve seen patients die because their primary care doctor said, ‘It’s fine, your sugar’s normal.’ That’s malpractice. And the FDA’s warning? It’s buried in a 47-page document. No one reads it. The system is broken.
Dan Adkins
As a physician with over 20 years in clinical practice, I must say: this is not a new phenomenon. It was documented in European journals as early as 2012, before the FDA issued any warning. The issue is not the drug-it is the erosion of clinical judgment in favor of algorithmic medicine. Glucose meters are convenient, but they are not diagnostic tools. The human body does not conform to software thresholds. If you rely on a number to make a clinical decision, you are not a doctor-you are a data clerk. And yes, this is why American healthcare is failing. We outsource thinking to machines.
Grace Rehman
Normal glucose doesn't mean safe
ketones don't care about your meter
your body doesn't read labels
it just burns
Erika Putri Aldana
So let me get this straight… you’re telling me I can’t just skip my meds when I’m sick because my sugar’s fine? But I’m supposed to trust a $20 meter over my own gut feeling? And now I have to buy ketone strips? This is why I hate modern medicine. They make you pay for every damn symptom now. I’m just trying to get over a cold, not run a lab.
Orlando Marquez Jr
It is imperative to underscore that the pathophysiological mechanism underlying euglycemic diabetic ketoacidosis in the context of sodium-glucose cotransporter-2 inhibition involves a dysregulation of the glucagon-to-insulin ratio, leading to unopposed lipolysis and ketogenesis, despite normoglycemia. The clinical implications are profound: diagnostic protocols must be revised to prioritize ketone quantification over glucose thresholds. Furthermore, public health messaging must be standardized across primary care, emergency departments, and pharmacy counseling to mitigate morbidity and mortality. The current disconnect between pharmacological innovation and clinical education represents a critical gap in patient safety.
Cameron Hoover
I almost died from this. I was on Jardiance. Got a cold. Glucose was 185. Felt like I was going to pass out. Thought I was just tired. My wife made me check ketones. 4.2. We went to the ER. The nurse said, ‘That’s not DKA, your sugar’s fine.’ I screamed. They finally listened. I was in the ICU for three days. They told me I was lucky. I’m not lucky. I’m angry. Why didn’t my doctor tell me this could happen? Why didn’t the pharmacy give me a warning? This isn’t science-it’s a gamble with your life.
Jerry Peterson
I’m a nurse in a small town clinic. We don’t have a ketone meter. We have urine strips. I’ve had to call 911 for three patients on SGLT2i’s with nausea and normal glucose. One was a 72-year-old woman who thought she had the flu. She had a pH of 7.15. We didn’t have the tools. We had to wait for transport. That’s not acceptable. We need these meters in every primary care office. This isn’t just for diabetics-it’s for everyone who’s on these drugs. We’re failing them.
Jay lawch
This is all part of the pharmaceutical agenda. They sell you a drug that makes you pee sugar, then they profit off the complications. They don’t want you to know that your body is being tricked into starvation mode. They want you to keep buying the pills and then the ketone strips and then the ER visits. The FDA? They’re bought. The doctors? They’re trained to trust machines. But the truth? SGLT2 inhibitors were designed to make Big Pharma rich, not to save lives. And now you’re being told to check ketones like you’re some kind of lab technician? That’s not medicine. That’s corporate control. And if you think this is about diabetes, you’re wrong. It’s about profit. Always profit.
Southern NH Pagan Pride
they told me it was just the flu but my ketones were 5.1 and my blood sugar was 198
now i think the gov is hiding the truth
why do they want us sick?
why do they make us buy meters?
why do they not warn us?
the real enemy is the system
not the drug
not the doctor
the system
Adrian Thompson
They don’t want you to know that SGLT2 inhibitors were originally developed by a company with ties to the insulin industry. The whole ‘low sugar = safe’ thing is a distraction. They want you to think you’re healthy because your glucose is normal. But your body’s burning fat like crazy. That’s not health. That’s metabolic sabotage. And now they want you to buy a $70 ketone meter? That’s not prevention. That’s a cash grab. They profit from your ignorance. Don’t be fooled.
Meina Taiwo
Stop the drug. Check ketones. Go to ER if symptoms. No exceptions.