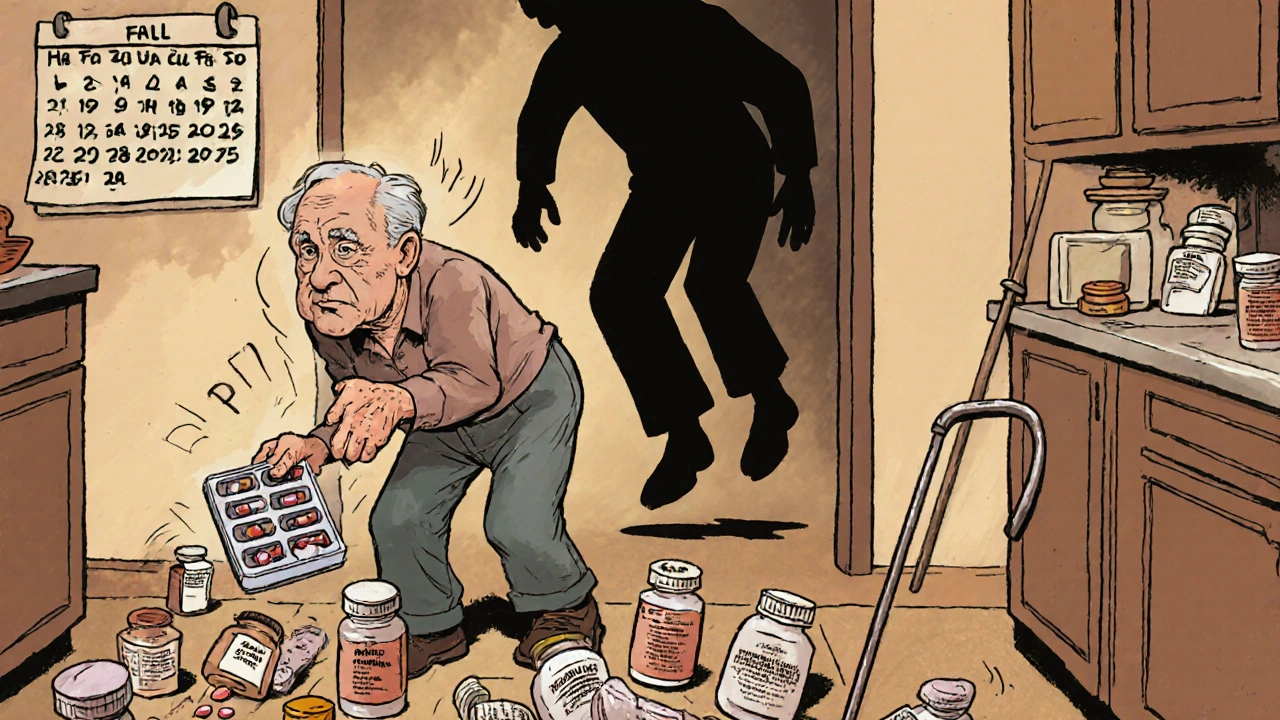
Every year, over 36 million older adults in the U.S. fall - and for many, the cause isn’t slippery floors or poor lighting. It’s a pill they’ve been taking for years. Sedating medications, meant to help with sleep, anxiety, pain, or muscle spasms, are quietly increasing the risk of falls that lead to broken hips, brain injuries, and even death. The good news? You can stop this. With the right steps, many of these falls are preventable - not by adding more safety gear, but by rethinking the meds themselves.
What Makes These Medications Dangerous?
Not all drugs are created equal when it comes to fall risk. Some medications slow down your brain, blur your vision, or make your legs feel heavy. These are called Fall Risk Increasing Drugs, or FRIDs. Common ones include:- Benzodiazepines (like diazepam or lorazepam) - used for anxiety or insomnia
- Antidepressants (especially tricyclics like amitriptyline) - can cause dizziness and drowsiness
- Opioids (like oxycodone or hydrocodone) - even low doses can impair balance
- Antipsychotics (like quetiapine or risperidone) - often prescribed off-label for sleep or agitation
- Antihypertensives - especially when doses are too high, causing blood pressure drops
- Baclofen - a muscle relaxant with the highest fall risk in its class
The STEADI-Rx Model: A Proven System
In 2018, the CDC launched STEADI-Rx - a practical, pharmacist-led system designed to cut medication-related falls. It’s not theory. It’s being used in pharmacies across the U.S. and has already prevented tens of thousands of falls. STEADI-Rx works in three steps:- Screen - Ask: Have you fallen in the past year? Do you feel unsteady? Do you take four or more medications?
- Assess - Review every medication. Look for FRIDs. Check doses. See if any can be stopped, lowered, or swapped.
- Intervene - Work with the prescriber to make changes. No guesswork. No pressure. Just clear, documented recommendations.
Why Medication Review Alone Isn’t Enough
Stopping a sedating pill helps - but it’s not a magic fix. The strongest results come from combining medication review with movement. Cochrane reviews show that exercise programs with balance, strength, and gait training reduce the number of people who fall by 15-29%. These aren’t fancy gym routines. They’re simple: standing on one foot, heel-to-toe walking, slow squats. Done 30-90 minutes, one to three times a week, for at least 12 weeks. When you pair medication review with exercise, the results jump. Falls leading to fractures drop by 61%. Falls needing emergency care drop by 43%. Vitamin D was once thought to help, but recent reviews show mixed results - it’s not a reliable standalone tool. Exercise is.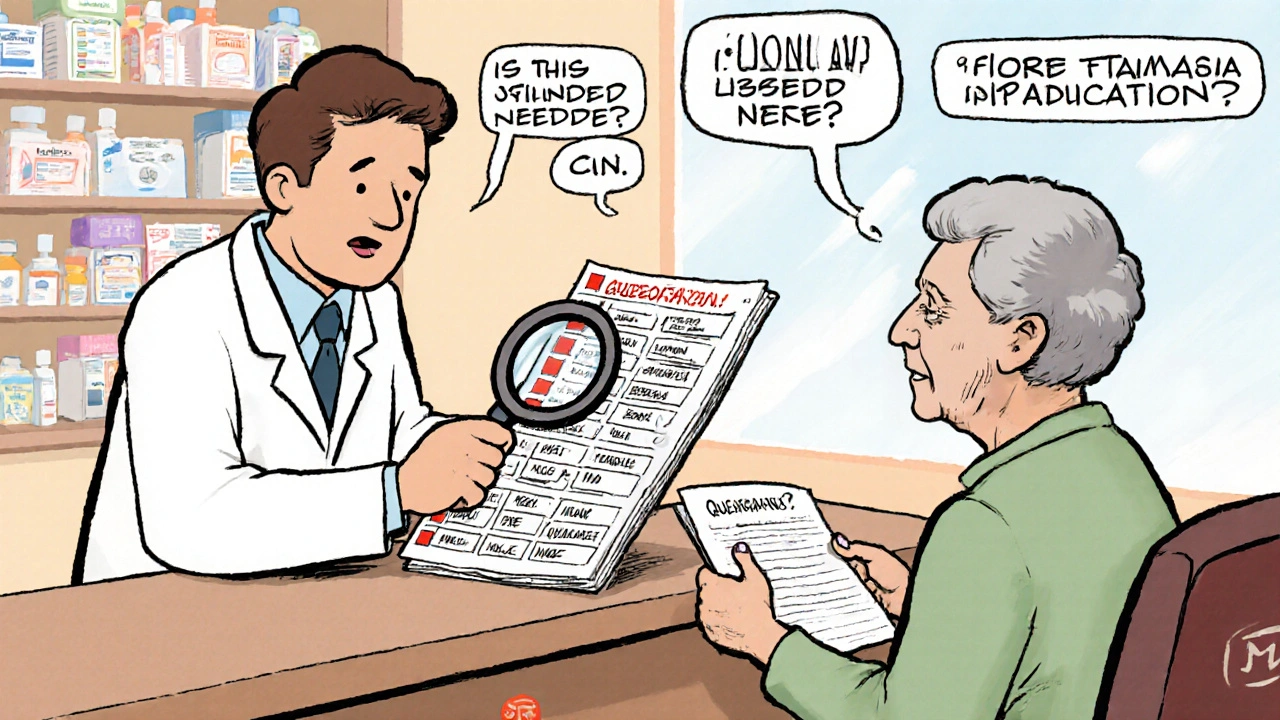
Who Should Be Doing This?
Doctors don’t always have time to review every pill. Pharmacists do. In fact, 82% of pharmacists believe medication reviews reduce fall risk - but only 45% feel they have enough time to do them right. This is where the system breaks down. Most older adults get their meds from community pharmacies - not hospitals. That’s where STEADI-Rx fits in. Pharmacists are trained to spot FRIDs, document issues, and send a simple Provider Consult Form to the prescriber. They ask three key questions:- Is this medication still needed?
- Is there a safer alternative?
- Can the dose be lowered?
The Real Barriers - And How to Beat Them
Changing meds sounds simple. It’s not. Patients often resist. They think, “This pill helps me sleep - if I stop, I’ll be back to lying awake all night.” Or, “I’ve been on this painkiller for years - my doctor said it’s fine.” A 2021 survey by the National Council on Aging found 63% of older adults struggled to reduce sedating meds due to fear of withdrawal or symptom return. Prescribers hesitate too. They worry about triggering anxiety, insomnia, or pain. The fix? Education and slow tapering. You don’t quit benzodiazepines cold turkey. You reduce the dose by 10-25% every 1-2 weeks, with close monitoring. Pharmacists can provide clear handouts: “Here’s what to expect. Here’s how to know if it’s working.” Electronic alerts in medical records also help. If a doctor prescribes a new sedative to someone already on two others, the system can flag it. That’s not nagging - it’s safety.What You Can Do Right Now
If you or someone you care for is over 65 and taking any sedating medication, here’s what to do:- Make a full list - Include every pill, patch, cream, and supplement. Bring it to the next appointment.
- Ask these questions:
- Is this drug still necessary?
- Is there a non-sedating option?
- Can the dose be lowered?
- Request a medication review - Ask your pharmacist if they use STEADI-Rx or offer medication therapy management.
- Start moving - Even 10 minutes a day of balance exercises helps. Try standing on one foot while brushing your teeth. Use a chair for support.
What’s Changing in 2025?
The landscape is shifting. In 2023, the CDC expanded its STEADI toolkit with specific deprescribing guides for benzodiazepines and opioids. The American Society of Consultant Pharmacists has certified over 1,200 Geriatric Pharmacotherapy Specialists - pharmacists with advanced training in senior medication safety. More states are allowing pharmacists to adjust certain prescriptions without a doctor’s note - a big step forward. And AI tools are being tested to flag high-risk drug combinations before they’re even prescribed. The message is clear: We can’t keep treating falls as accidents. For older adults on sedating meds, they’re a predictable, preventable outcome.Can stopping a sedating medication really prevent falls?
Yes. Studies show that carefully reducing or switching sedating medications - especially benzodiazepines, antidepressants, and opioids - can cut fall risk by up to 40%. One study found that 75% of medication changes made through the STEADI-Rx program involved switching to a safer alternative, leading to fewer falls and improved balance.
Which medications carry the highest fall risk?
Baclofen (a muscle relaxant), benzodiazepines like diazepam, tricyclic antidepressants like amitriptyline, and opioids such as oxycodone have the strongest links to falls. Even at low doses, these drugs can cause dizziness, slow reaction time, and impaired coordination. The Beers Criteria, updated annually by the American Geriatrics Society, lists these as potentially inappropriate for older adults.
Is vitamin D enough to prevent falls?
No. While vitamin D was once thought to reduce falls, recent reviews show inconsistent results. The U.S. Preventive Services Task Force recommends 800 IU daily, but a Cochrane review found no significant benefit on its own. Exercise - especially balance and strength training - is far more effective. Vitamin D may help if someone is deficient, but it shouldn’t be relied on as a primary prevention tool.
How can I talk to my doctor about changing my meds?
Be specific. Say: “I’ve noticed I’ve been unsteady lately, especially after taking [medication name]. I’m worried about falling. Can we review whether this is still necessary or if there’s a safer option?” Bring a full list of all your meds. Ask if they’re familiar with STEADI-Rx or medication therapy management. Most doctors welcome the input - especially if it comes with a pharmacist’s recommendation.
What kind of exercise helps most with fall prevention?
Balance, strength, and gait training. Examples: standing on one foot (hold onto a chair), walking heel-to-toe in a straight line, slow squats, and tai chi. Programs should last 30-90 minutes, 1-3 times per week, for at least 12 weeks. Even simple daily habits - like standing on one foot while brushing your teeth - add up over time. The goal isn’t fitness; it’s stability.
Can pharmacists really change my medications?
In most cases, no - but they can recommend changes. Pharmacists can’t legally stop or switch your prescriptions without a doctor’s approval. But they can document risks, suggest alternatives, and send a formal consultation to your prescriber. In some states, pharmacists now have limited prescribing authority for certain conditions, and this is expanding. Their role is critical in identifying problems and starting the conversation.
How long does it take to see results after stopping a sedating med?
Improvement can start within days to weeks. Dizziness and drowsiness often lift quickly after reducing a benzodiazepine or opioid. But balance and coordination take longer - up to 6-8 weeks - especially if muscle weakness has developed from inactivity. Pairing medication changes with exercise speeds up recovery. Always taper slowly under medical supervision to avoid withdrawal.


Robert Merril
So let me get this right we’re gonna stop giving old folks their sleep pills but not fix their broken stairs or install better lighting why is it always the meds not the environment
Kathy Grant
I’ve watched my mom go from falling twice a week to zero after we cut her off lorazepam and started daily chair yoga. It wasn’t easy she cried for a week but the quiet mornings now? Worth it. The body remembers balance if you give it time and stop poisoning it with midnight sedatives. No magic pill just patience and a little courage.
Georgia Green
my aunt took baclofen for 5 years and no one ever told her it was the #1 fall risk. she broke her hip and they blamed her age. it was the drug. pharmacists need to be louder about this.
Roberta Colombin
Every person deserves to age with dignity and safety. Taking a moment to review medications is not about taking away comfort-it is about restoring freedom. A simple walk without fear is worth more than a night of sleep clouded by drowsiness. Let us choose life over sedation, one pill at a time.
Ashley Unknown
They’re not trying to help us they’re trying to control us. The pharmaceutical industry doesn’t want you to know this but they’ve been pushing these drugs for decades because they make billions. Now they want you to blame the meds instead of the system. Who funds the CDC’s STEADI program? Who owns the patents on the ‘safer alternatives’? This is a distraction. They’ll replace one pill with another that costs more and comes with a new side effect. Wake up. This isn’t medicine it’s marketing dressed in lab coats.
Noel Molina Mattinez
my grandpa took 12 meds and fell every week he stopped 4 and now he walks to the mailbox every morning no more hospital visits no more drama just him and his cane and the sun
Eva Vega
The clinical utility of deprescribing FRIDs within the geriatric pharmacotherapeutic paradigm demonstrates a statistically significant reduction in fall-related morbidity. The integration of pharmacist-led MTM protocols aligns with the 2023 Beers Criteria update and is supported by Level I evidence from the Cochrane Collaboration.
Christina Abellar
My dad started balance exercises after his meds were reviewed. He says he feels like himself again. No drama. Just better.
Matt Wells
The assertion that exercise alone yields a 61% reduction in fracture-causing falls is methodologically suspect. The studies cited conflate compliance bias with causal efficacy. Without randomized double-blind control for physical activity adherence, the data remains correlational at best. One must question the epistemological foundation of such claims.
Dave Feland
They’re calling this prevention? This is just the government’s next step toward mandatory drug reduction. Next they’ll tell you what vitamins to take, what time to sleep, and whether you’re allowed to have coffee. The CDC doesn’t care about your safety-they care about controlling your body. They’ve been doing this for decades with smoking, sugar, salt. Now it’s your sleeping pills. Wake up. This isn’t medicine. It’s social engineering.