Protein Calculator for Parkinson's Patients
Calculate Your Protein Needs
Protein timing affects levodopa effectiveness for Parkinson's patients. Your body needs protein, but timing matters.
Enter your weight to see your ideal protein intake range.
Why This Matters
For Parkinson's patients taking levodopa, protein competes with medication absorption. The recommended range is 0.6-0.8 grams of protein per kilogram of body weight. This helps balance medication effectiveness and nutritional needs.
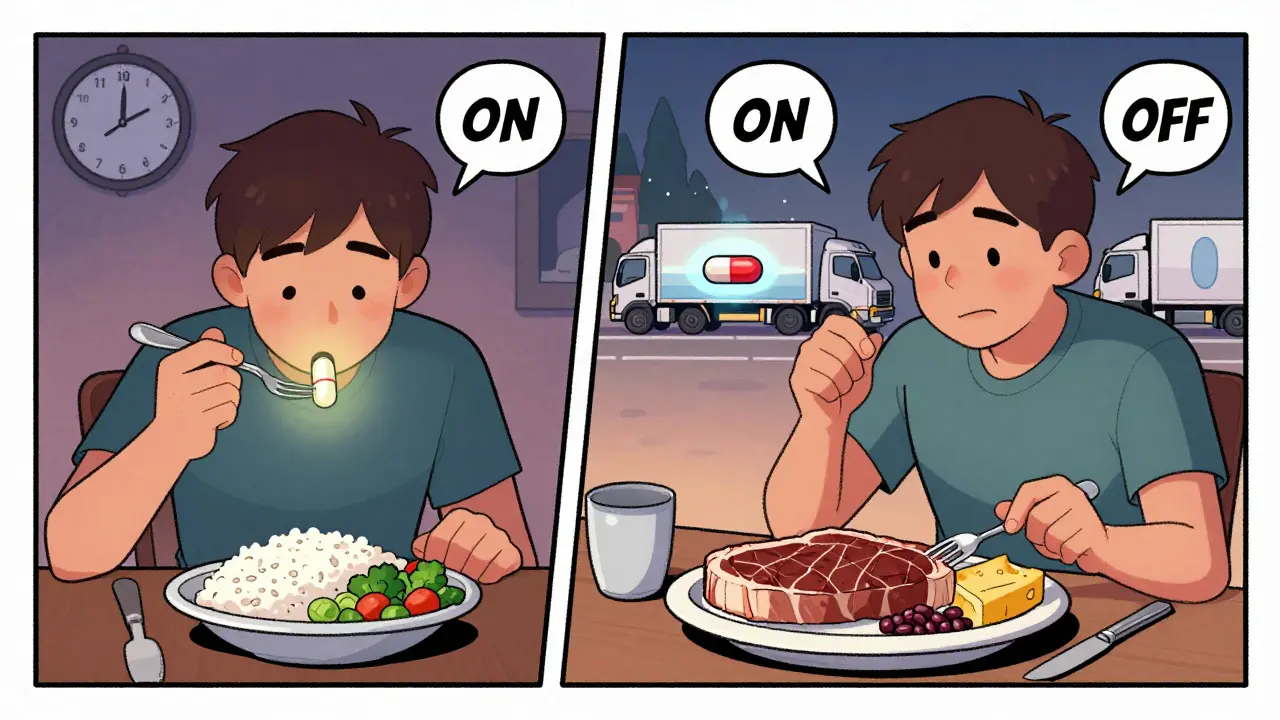
For people with Parkinson’s disease taking levodopa, what you eat can directly impact how well your medication works. It’s not just about timing your pills - it’s about what’s on your plate. A high-protein meal can make levodopa less effective, leading to sudden "off" periods where movement becomes stiff, slow, or unpredictable. This isn’t a myth or a rumor. It’s a well-documented, biological clash between food and medicine - and it affects up to half of long-term levodopa users.
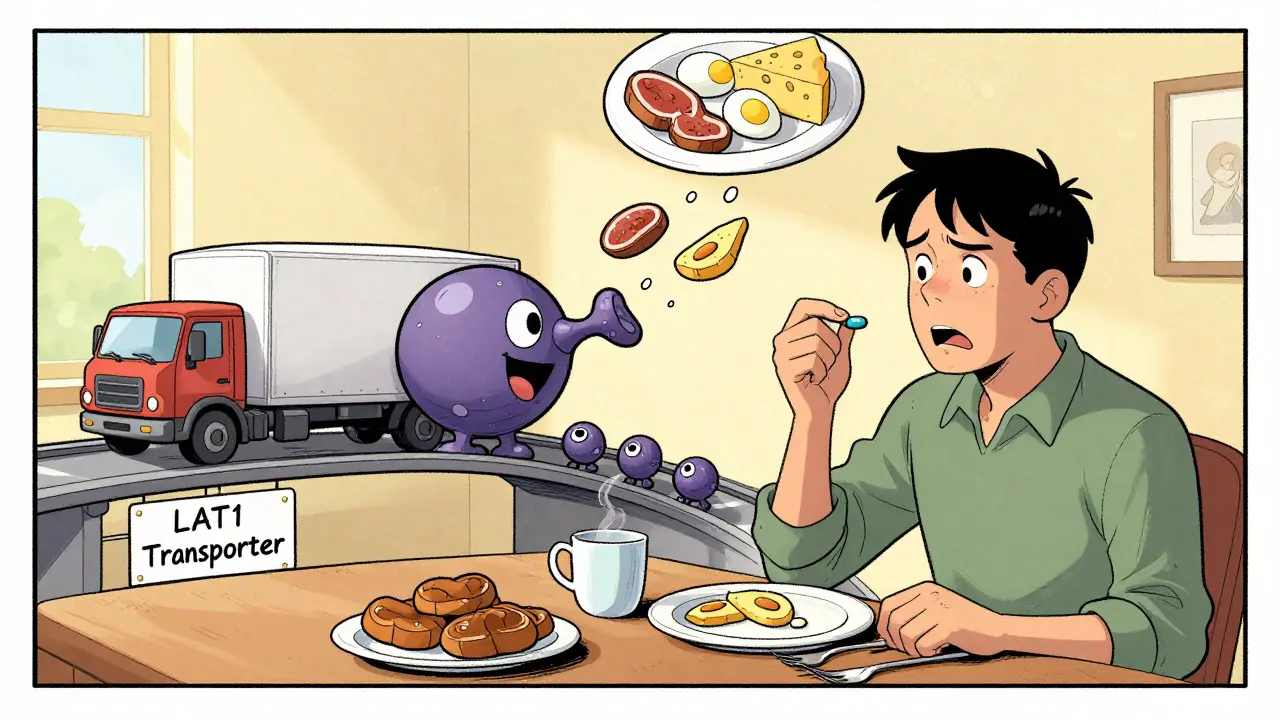
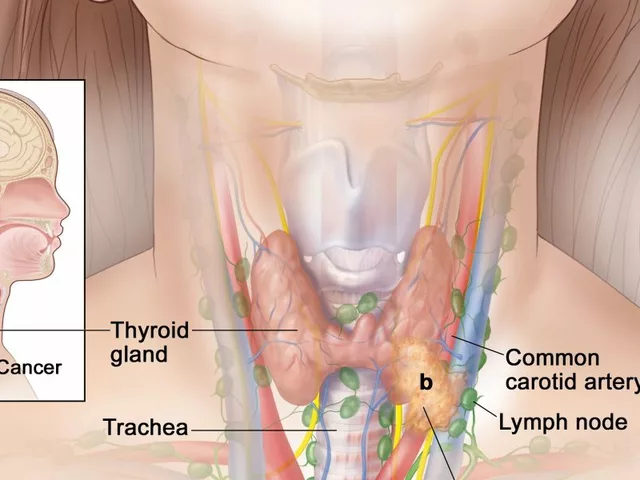
Why Protein Interferes with Levodopa
Levodopa is the gold-standard medication for Parkinson’s. It’s the molecule your brain converts into dopamine to help control movement. But here’s the catch: levodopa doesn’t just float freely into your brain. It needs help getting through the gut and across the blood-brain barrier. That help comes from a specific transporter system called LAT1 - the same one that carries large neutral amino acids (LNAAs) from digested protein.When you eat meat, eggs, beans, or dairy, your body breaks down the protein into amino acids like leucine, tyrosine, and phenylalanine. These amino acids flood your bloodstream and compete with levodopa for the same transporters. Think of it like a single-lane bridge during rush hour. Only so many cars can cross at once. If a truckload of trucks (amino acids) shows up, the car (levodopa) gets stuck waiting.
Studies show that after a high-protein meal, plasma levels of these amino acids rise by 30-50% within 30-60 minutes. That’s enough to cut levodopa absorption by 25-40% and delay its peak effect by nearly an hour and a half. The result? You take your pill, but your tremors don’t improve - or they improve much later than usual. This isn’t just inconvenient. It’s dangerous. Unpredictable motor control increases fall risk and reduces quality of life.
When Does This Problem Show Up?
Not everyone with Parkinson’s is affected. The protein-levodopa conflict usually becomes noticeable after you’ve been on levodopa for about 8 years - or roughly 13 years after motor symptoms first appear. That’s when your body’s ability to handle fluctuations starts to decline, and the transporter system becomes more sensitive to competition.By the time someone reaches Hoehn & Yahr stage 3 or 4 (moderate to severe Parkinson’s), about 40-50% experience clear motor fluctuations tied to meals. One study found that eating a high-protein lunch increased motor "off" time by 32-79%, depending on how symptoms were measured. That’s not a small difference - it’s the difference between walking across the room and needing help to stand up.
Three Dietary Strategies That Work
There’s no one-size-fits-all fix, but three approaches have shown real results:- Low Protein Diet (LPD): Limits total daily protein to 0.6-0.8 grams per kilogram of body weight. For a 70kg person, that’s about 45-55g of protein per day. This is tough. Most people eat 80-100g daily. Cutting back this much means giving up meat, cheese, eggs, and even legumes. Many people lose weight - sometimes too much. A 2022 survey found 31% of strict LPD users lost over 5% of their body weight in six months.
- Protein Redistribution Diet (PRD): This is the most effective strategy. Instead of cutting protein, you move it. You eat only 7g or less during the day (breakfast, lunch, snacks) and save 80-85% of your daily protein for dinner. Studies show PRD reduces "off" time by up to 107 minutes per day and adds 30 minutes of reliable "on" time. It works because levodopa absorption is less affected when amino acid levels are low. At night, when dopamine needs are lower and movement is less critical, the competition doesn’t matter as much.
- PRD with Low-Protein Products: Some people use special low-protein bread, pasta, and flour to make meals more satisfying. These products help, but only 22% of users say they’re significantly easier to stick with. They’re expensive and hard to find outside North America and Europe.
PRD consistently outperforms simple protein restriction. One study found it reduced motor fluctuations 35% more than LPD alone. But adherence is the biggest problem. A 2023 review found 68% of people quit PRD within a year. Why? Social meals, family dinners, cultural foods - they all get in the way.
Real People, Real Strategies
People with Parkinson’s aren’t just following clinical guidelines - they’re inventing workarounds.One Reddit user, u/ParkinsonsWarrior, reported gaining 2.5 hours of reliable mobility each day after switching to PRD under a dietitian’s guidance. Others use "protein holidays" - one high-protein meal at night, with low-protein meals the rest of the day. That approach works for 65% of users.
Many find success by timing their pills: take levodopa 45-60 minutes before eating. This gives it a head start. One study showed a 72% success rate when people took their morning dose before breakfast. But this doesn’t work for everyone. If your stomach empties slowly - common in advanced Parkinson’s - the pill might sit there, waiting, while amino acids flood in later.
Tracking helps. Nearly half of users who stick with dietary changes use apps like MyFitnessPal to log protein. Others keep a food and symptom diary. One woman in Perth noticed her hands shook badly after her weekly pasta night. She swapped regular pasta for low-protein pasta - and her tremors improved within days.
What Experts Say
There’s no universal rule. Dr. Carley Rusch, a dietitian specializing in Parkinson’s, says: "Addressing protein interactions is not a one-size-fits-all approach. We need to customize the recommendations to fit the person we are treating."Some experts, like Dr. J. Eric Ahlskog, recommend eating protein either one hour before or one hour after levodopa. Others warn against protein restriction entirely in underweight patients (BMI under 20). In fact, 22% of long-term PRD users develop deficiencies in vitamin B12 or iron. Weight loss, muscle loss, and fatigue are real risks.
The Michael J. Fox Foundation notes that only 40-50% of Parkinson’s patients have clinically significant protein interference. That means if you’re not having trouble with motor fluctuations after meals, you probably don’t need to change your diet. Testing matters. Talk to your neurologist. Track your symptoms. Don’t assume you’re affected.

What You Can Do Today
You don’t need to overhaul your life. Start small:- Check your daily protein intake. Use an app or food scale. Most people eat 80-100g. The target for PRD is 45-53g.
- Try taking levodopa 45 minutes before breakfast. See if your morning mobility improves.
- Replace one high-protein meal with a low-protein option. Swap eggs for oatmeal. Swap chicken for rice and vegetables.
- Save your meat, cheese, and beans for dinner. Make that your "protein night."
- Ask your doctor for a referral to a dietitian who specializes in Parkinson’s. People who get professional help are 78% more likely to see symptom improvement.
Don’t go too far. Protein isn’t the enemy. Your muscles, your immune system, your energy - they all need it. The goal isn’t to eliminate protein. It’s to manage the timing so your medication can do its job.
What’s Next?
Researchers are testing a new approach called "protein pacing." Instead of restricting protein or moving it to dinner, they’re giving small amounts throughout the day - like 5g every 3 hours. Early trials show 68% of participants respond well, with much better adherence than PRD. It’s still in Phase II trials, but it could be a game-changer.For now, the best advice is simple: know your body. Track your meals and your symptoms. Talk to your care team. And don’t let fear of dietary changes stop you from taking control. With the right plan, you can eat well, stay strong, and move better.
Does every Parkinson’s patient need to limit protein?
No. Only about 40-50% of people on long-term levodopa experience significant motor fluctuations due to dietary protein. If your symptoms are stable after meals, you likely don’t need to change your diet. Testing your response - by tracking symptoms before and after high-protein meals - is the best way to know if this applies to you.
Can I still eat meat and eggs if I have Parkinson’s?
Yes, but timing matters. Instead of eating them with your levodopa dose, save them for dinner. A protein redistribution diet (PRD) lets you enjoy meat, eggs, and dairy - just not during the day when your medication needs to work. Many people find this approach sustainable and satisfying.
How long does it take to see results from a protein-restricted diet?
Most people notice changes within 1-2 weeks, especially if they time their medication before meals. Full benefits - like reduced "off" time and more predictable movement - usually appear after 3-6 weeks of consistent change. Patience and tracking are key.
Is it safe to cut protein for a long time?
Not without supervision. Long-term protein restriction can lead to muscle loss, weight loss, and deficiencies in vitamin B12, iron, and other nutrients. People with Parkinson’s already face higher risks of malnutrition. Always work with a dietitian who understands Parkinson’s to ensure you’re getting enough calories and nutrients.
What if I can’t stick to a low-protein diet?
You’re not alone. Most people struggle with strict diets. The good news? Even small changes help. Try taking levodopa 45 minutes before breakfast, or swap one high-protein meal for a low-protein option. Small, consistent steps are better than perfection. Many find success with "protein holidays" - one high-protein meal a day, at night. Talk to your care team about what’s realistic for your life.
For more personalized advice, ask your neurologist about a referral to a dietitian who specializes in Parkinson’s. Many hospitals and clinics now offer these services - and they make a real difference.


Marie Fontaine
I started PRD last month and my morning tremors are WAY better. Took my pill before breakfast like they said and swapped eggs for oatmeal. No more waiting 90 mins to feel anything. Game changer. 🙌
Random Guy
so like... i tried this protein thing and honestly? i just ate a whole roast chicken at 7am and took my meds right after. i’m still here. still moving. maybe it’s all just placebo and we’re all overthinking this?
Brandon Osborne
You people are so naive. This isn’t about nutrition - it’s about Big Pharma pushing low-protein diets to sell you expensive ‘Parkinson’s pasta’ and ‘levodopa-friendly’ meal kits. They don’t want you to know the real truth: levodopa’s effectiveness drops because the FDA allows synthetic dopamine analogs to be patented, not because of amino acids. Wake up. The system is rigged.
Ryan Vargas
Let’s not reduce this to dietary minutiae. The protein-levodopa interaction is merely a symptom of a deeper ontological crisis in modern neuropharmacology. We have reduced human neurochemistry to a biochemical traffic jam, as if consciousness can be modeled by lane allocation on a single transporter highway. The real question isn’t ‘when to eat meat’ - it’s ‘why do we allow pharmaceutical intervention to dictate the rhythm of biological existence?’ The body isn’t a machine. The brain isn’t a pipeline. And levodopa? It’s just a temporary patch on a leaking vessel of meaning.
MANI V
I’ve been doing this for 12 years. You’re all doing it wrong. Protein redistribution? Pfft. The real solution is to eat zero protein until 8 PM. Zero. Not 7g. Not 10g. ZERO. And take your meds on an empty stomach with a glass of lemon water. I lost 40 lbs. My tremors vanished. Why? Because I have discipline. You people just want a quick fix. That’s why you fail.
Tasha Lake
Just FYI - LAT1 transporters have a Km for leucine of ~120μM, and plasma LNAA concentrations post-meal can hit 400-600μM. That’s a 3-5x competitive advantage. So yeah, the mechanism is solid. Also, PRD’s 107-min reduction in off-time? That’s a Cohen’s d > 1.2. Effect size is massive. Not anecdotal.
Ken Cooper
i tried the protein thing but honestly i just cant give up my morning eggs. so i started taking my levodopa 90 mins before breakfast instead. works 80% of the time. also i use myfitnesspal to log everything. its kinda addicting. like a game. ‘today i hit 43g protein’ - yes! i won. lol.
Brett Pouser
I’m from Nigeria. We eat a lot of beans and yam. My uncle has Parkinson’s. He eats beans at night, rice and veggies all day. No meat. No dairy. He’s been stable for 4 years. No fancy pasta. Just tradition + timing. Maybe the answer isn’t in Western diet science - maybe it’s in what we’ve always done.
John McDonald
I love that this post didn’t just say ‘eat less protein’ but actually gave options. PRD + timing + tracking = the trifecta. I’ve been doing all three for 6 months. My wife says I walk like a new man. Also - low-protein bread is weird. But worth it. Just don’t buy the ‘artisanal’ stuff. It’s $12 a loaf. Use the generic.
Brandon Osborne
Wow. Look at all these people patting themselves on the back for ‘doing PRD’. You think you’re so smart? You’re just following a protocol. Meanwhile, real Parkinson’s warriors are out here fighting the system - the pharmaceutical-industrial complex, the diet culture, the ableist assumption that we should ‘adjust our lives’ instead of demanding better drugs. You’re not heroes. You’re compliant.