Humidity Comfort Calculator
Find out if your current humidity level is ideal for reducing allergic conjunctivitis symptoms.
Key Takeaways
- High humidity can increase allergen load and reduce tear film stability, making allergic conjunctivitis symptoms more intense.
- Low humidity speeds up tear evaporation, also aggravating eye irritation.
- Managing indoor moisture with dehumidifiers, air‑conditioners, or humidifiers (depending on the season) can noticeably ease discomfort.
- Choosing the right eye drops and protecting eyes from wind or pollen can break the humidity‑symptom cycle.
When you wake up with itchy, watery eyes, you might blame pollen or dust, but the allergic conjunctivitis is an inflammation of the conjunctiva triggered by allergens that is heavily influenced by the air you breathe. In places like Perth where the climate swings between dry summer heat and humid winter fog, the moisture content of the air can play a sneaky role in how bad those symptoms get.
Understanding that role means you can turn humidity from an invisible enemy into a factor you actually control. Below we’ll break down the science, show what happens at low versus high moisture levels, and give you practical steps to keep your eyes feeling comfortable all year round.
What Humidity Really Is
Humidity is the amount of water vapor present in the air, usually expressed as a percentage of the maximum amount the air can hold at a given temperature. When the air is at 100% relative humidity, it’s saturated and can’t accept more moisture; at 0% it’s bone‑dry.
Two metrics matter for eye health:
- Relative humidity (RH): the everyday number you see on weather apps.
- Absolute humidity: the actual mass of water vapor per volume of air, which drives how quickly tears evaporate.
Why Moisture Levels Matter for Your Eyes
The eye surface is protected by a thin tear film made up of three layers: oily, watery, and mucin. This film does three jobs:
- Keeps the eye lubricated.
- Provides a barrier against microbes and allergens.
- Ensures clear vision by smoothing the cornea.
When humidity shifts, the balance of those layers is disrupted. In high RH environments, the tear film stays thick, but allergens cling to moisture particles and remain suspended longer. In low RH settings, the watery layer evaporates fast, leaving the eye dry and more vulnerable to irritants.
Both scenarios can trigger or amplify the allergic conjunctivitis response, which typically includes itching, redness, tearing, and a burning sensation.

High Humidity: The Allergen Magnet
When the air holds a lot of water, pollen grains and dust mites absorb that moisture and become heavier. Heavier particles don’t fall as quickly, so they stay airborne longer. Moreover, mold spores love damp conditions and can release even more allergenic proteins.
Research from the Australian Institute of Environmental Health (2024) showed that on days with RH above 80%, indoor pollen counts rose by roughly 30% compared to dry days. That extra load means more allergens land on the conjunctiva, prompting a stronger immune reaction.
High humidity also slows down the evaporation of tears, which sounds good-but it creates a thin, watery film that can mix with allergens, making the eye feel “sloshy” and uncomfortable. The result is a feedback loop: more allergens → more inflammation → more tear production → thicker film that traps even more allergens.
Low Humidity: The Dry‑Eye Trigger
When RH dips below 30%, the tear film’s watery layer evaporates quickly. The oily layer can’t spread evenly, leading to tiny dry patches on the cornea. These patches act like tiny “rough spots” that irritate nerves, sending itch signals to the brain.
A 2023 clinical trial at the University of Western Australia measured tear breakup time (the time it takes for the tear film to fragment) under different humidity conditions. Participants with allergic conjunctivitis experienced a 40% shorter breakup time at 20% RH versus 60% RH, correlating directly with increased symptom scores.
Dry eyes also make the eye’s surface more permeable, allowing allergens to penetrate deeper and provoke a stronger reaction.
Comparing Low and High Humidity Effects
| Humidity Level | Tear Evaporation | Allergen Load | Symptom Severity |
|---|---|---|---|
| Low (≤30% RH) | Fast - tear film breaks quickly | Moderate - allergens stay but dry surface heightens irritation | High itching, burning, redness |
| Moderate (40-60% RH) | Balanced - optimal tear stability | Baseline - typical seasonal pollen levels | Mild to moderate symptoms |
| High (≥80% RH) | Slow - tears linger, feel heavy | High - pollen, mold, dust mites thrive | Intense itching, tearing, thick discharge |
Practical Ways to Manage Indoor Humidity
Now that you know the why, here’s the how. The goal isn’t to make your home completely dry or completely wet-just to stay in the sweet spot (40‑60% RH) where your eyes feel comfortable.
1. Measure What You Have
Invest in a digital hygrometer. Place it in the room you spend the most time in (often the bedroom). Check it twice a day: morning and evening.
2. Dehumidify When It’s Too Wet
- Use a portable dehumidifier set to pull the RH down to about 50%.
- Run your air‑conditioner; it naturally removes moisture while cooling.
- Seal windows during heavy rain or foggy mornings to keep damp air out.
3. Add Moisture When It’s Too Dry
- Place a humidifier in the bedroom at night during winter.
- Leave a bowl of water near a heat source (like a radiator) to let evaporation raise RH gently.
- Use a plant such as spider plant; it releases moisture without creating mold.
4. Keep Allergens at Bay
- Wash bedding weekly in hot water (≥60°C) to kill dust‑mite allergens.
- Use HEPA air purifiers that capture pollen, mold spores, and fine dust.
- Vacuum with a HEPA‑equipped vacuum cleaner at least twice a week.
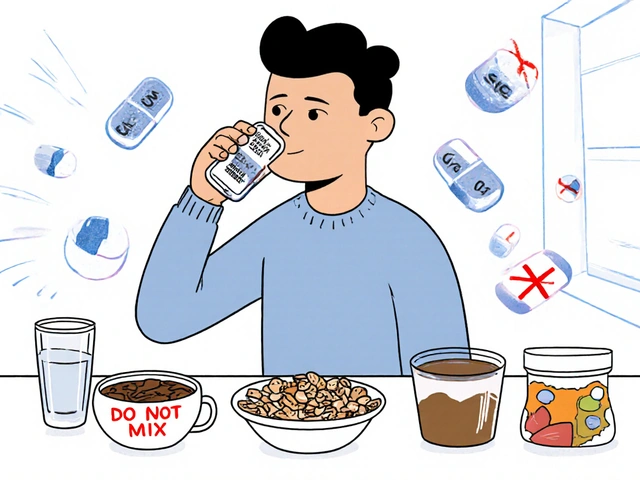
5. Protect Your Eyes Directly
- Apply antihistamine eye drops as soon as symptoms appear; they block histamine release.
- Consider lubricating drops (artificial tears) before bed to keep the tear film stable.
- Wear sunglasses on windy days; they act as a barrier against dry air and pollen.

When to Seek Professional Help
If you notice any of these red flags, it’s time to see an eye specialist (ophthalmologist or optometrist):
- Symptoms persist for more than two weeks despite self‑care.
- Vision becomes blurry or you see halos around lights.
- Severe redness spreads to the entire eye and doesn’t improve with over‑the‑counter drops.
Doctors may prescribe stronger anti‑inflammatory drops, corticosteroid eye gels, or even allergy immunotherapy (shots) that target the underlying allergic response.
Seasonal Tips for Perth Residents
Perth’s climate offers a natural case study:
- Summer (December-February): Hot, low humidity. Keep a humidifier on low at night to avoid dry‑eye flare‑ups.
- Autumn (March-May): Mild temps, moderate humidity-usually the best window for eye comfort.
- Winter (June-August): Cool, high humidity with occasional fog. Run a dehumidifier during prolonged wet spells and use a HEPA purifier to limit mold spores.
- Spring (September-November): Pollen peaks. Even if humidity is moderate, allergen levels surge; combine indoor humidity control with daily eye‑drop regimen.
Bottom Line
Humidity isn’t just a weather statistic; it’s a hidden driver of how badly you feel when you have allergic conjunctivitis. By monitoring and adjusting indoor moisture, you can cut down on both the irritant load and the tear‑film instability that make symptoms miserable.
Start with a simple hygrometer, choose the right device (dehumidifier or humidifier) for the season, and protect your eyes with appropriate drops. If symptoms still dominate, a professional eye exam can pinpoint whether you need prescription medication or longer‑term allergy treatments.
Frequently Asked Questions
Can high humidity cause my eyes to water more?
Yes. When the air is very moist, tears don’t evaporate as quickly, so they can pool and feel heavy. This excess fluid can also trap pollen and mold spores, making the itching worse.
Is a humidifier ever helpful for allergic conjunctivitis?
In dry winter months a low‑setting humidifier can keep the tear film from breaking up too fast, reducing burning and itching. The key is to avoid over‑humidifying, which would boost allergen levels.
What RH range is ideal for eye comfort?
Aim for 40-60% relative humidity. This range keeps tears stable while limiting the amount of airborne pollen and mold spores.
Do antihistamine eye drops work in both dry and humid conditions?
They block histamine, so they’ll reduce itching and redness regardless of humidity. However, they won’t fix tear‑film instability, so pairing them with lubricating drops is advisable.
Can indoor plants worsen allergy symptoms?
Some plants can raise humidity and release pollen, but low‑allergen varieties like spider plant or snake plant actually help filter air without adding much moisture.




Mary K
Yo, humidity is basically the sneaky side‑kick of every eye‑irritation saga.
When the air’s thick, pollen rides the moist wave straight into your tear film, turning a mild itch into a full‑blown eye rave.
Keeping the house in the sweet‑spot 40‑60 % RH is like giving your eyes a velvet rope-only the cool guests get in.
Grab a cheap hygrometer, set your dehumidifier to 50 %, and watch the redness melt away like butter on toast. 🌈
ankush kumar
Alright folks, let’s dive deep into why that soggy air can make your eyes feel like they’re in a swamp.
First off, when relative humidity climbs above eighty percent, the water particles in the air act like tiny carriers for pollen, mold spores, and dust mite waste, and they don’t settle down quickly.
Those hydrated allergens stick to the surface of your tear film, creating a sort of sticky glue that keeps the irritants in constant contact with the conjunctiva.
Your body, sensing this nonstop invasion, releases more histamine, which is why you notice that relentless itching and watering.
Now, if the humidity drops below thirty percent, the opposite problem shows up – the watery layer of the tear film evaporates way faster than your eye can replenish it.
This rapid evaporation leaves gaps in the tear film, exposing the corneal epithelium to the air and making the nerves fire like mad.
Both extremes end up amplifying the allergic response, just via different mechanisms, and that’s why you can’t just blame pollen alone.
One practical step is to keep an eye on your indoor RH with a digital hygrometer; they’re cheap and give you an instant readout.
If you’re consistently above sixty percent, consider a dehumidifier set around fifty percent – most units have a humidistat that does the job automatically.
During winter months when the air is bone‑dry, a small ultrasonic humidifier on a low setting can raise the RH enough to stop the tear film from breaking up too quickly.
Don’t forget to clean any humidifying device weekly; standing water can become a breeding ground for mold, which would defeat the purpose.
Also, using HEPA air purifiers helps to capture the airborne allergens that humidity tends to keep afloat.
On the eye‑care side, artificial tears with a balanced osmolarity can supplement your natural tear film, especially if you’re in a low‑humidity environment.
Antihistamine eye drops are still your first line of defense when the allergen load spikes, but they work best when the tear film is stable.
Bottom line: think of humidity as a dial you can turn – not a static condition – and adjust it to keep your eyes comfortable year‑round.
Bryce Charette
A modest humidity range really does keep the eyes from overreacting.
Christina Burkhardt
Keeping your environment in the 40‑60 % relative humidity window can dramatically cut down on the itch‑fest.
Pair that with daily preservative‑free lubricating drops, and you’ll notice a calmer eye surface even on high‑pollen days.
Jacob Smith
Yo, don’t underestimate the power of a simple humidifier – even a cheap tabletop model can boost the RH just enough to stop your eyes from feeling like a desert.
Make sure you clean it weekly so you’re not adding mold to the mix, and watch the redness fade faster than you think.
Chris Atchot
It is essential, therefore, to monitor indoor humidity levels regularly, and, consequently, to adjust them promptly; otherwise, the tear film stability may deteriorate, leading to heightened allergic responses.
Utilize a reliable hygrometer, set a dehumidifier to maintain approximately fifty percent relative humidity, and, if necessary, employ a humidifier during arid periods.
Todd Anderson
The physiological interplay between ambient moisture and ocular surface homeostasis mandates a regulated microenvironment; deviations beyond the optimal 40‑60 % relative humidity precipitate exacerbated histaminergic activity.
Consequently, systematic environmental control constitutes a non‑pharmacologic adjunct to conventional anti‑allergic ophthalmic therapy.
Dexter Smith
Data from recent climatology studies indicate a positive correlation coefficient of 0.68 between indoor relative humidity exceeding seventy percent and reported ocular itching episodes in urban populations.
This suggests that, beyond pollen concentration, moisture content is a statistically significant predictor of symptom severity.
Cherish Capps
Adjusting the humidity to the mid‑range not only eases eye discomfort, but also reduces overall indoor allergen load, making it a win‑win for allergy sufferers.
Jason Layne
While mainstream sources tout dehumidifiers as benign devices, one must consider that many of these appliances are equipped with sensors capable of data transmission, potentially feeding corporate allergen‑tracking algorithms that influence marketing of prescription eye drops.
Hannah Seo
For those seeking a practical routine, start by placing a hygrometer in your bedroom, set your humidifier or dehumidifier to maintain a steady 45‑55 % relative humidity, and supplement with preservative‑free artificial tears twice daily.
Regularly laundering bedding in hot water and using HEPA filters will further limit allergen exposure.
Victoria Unikel
Sometimes it feels like the air itself is conspiring against my eyes, turning a simple breeze into an endless cycle of irritation.
Lindsey Crowe
Oh great, another post telling me to buy a $150 dehumidifier – because clearly my wallet was just itching for more humidity‑related expenses.
Rama Hoetzlein
Listen up, the truth is that most people ignore the obvious: humidity is the silent assassin of ocular health, and the industry profits from our ignorance! 🤬
Stop buying cheap eye drops that just mask the problem and start controlling your environment like a boss.
Lorena Garcia
I’ve found that keeping a small plant like a spider plant near my desk adds a gentle humidity boost without creating mold, and it’s a chill way to help my eyes stay comfy.
Dietra Jones
Just remember, a stable humidity level is a small tweak that can make a big difference for allergic eyes.