IPF Progression Calculator
Estimate Your Disease Progression
Pirfenidone can slow the decline in lung function by approximately 45%. This tool estimates how much progression might be reduced with treatment.
When doctors talk about slowing down Idiopathic Pulmonary Fibrosis (IPF), the name pirfenidone comes up a lot. Understanding why this oral medication matters can help patients, families, and clinicians make smarter choices about care.
Key Takeaways
- Pirfenidone is an antifibrotic drug that reduces scar formation in the lungs.
- Clinical trials show it can slow the decline in forced vital capacity (FVC) by ~45% compared with placebo.
- Typical dosing starts low and ramps up to 801 mg three times a day to improve tolerance.
- Common side effects are gastrointestinal and skin‑related; most can be managed with simple strategies.
- It is usually prescribed for patients with mild‑to‑moderate IPF who can tolerate oral therapy.
What Is Idiopathic Pulmonary Fibrosis?
Idiopathic Pulmonary Fibrosis is a chronic, progressive lung disease characterized by thickening and stiffening of the alveolar walls due to excessive scar tissue. The term "idiopathic" means the exact cause is unknown, but risk factors include age (most patients are over 60), smoking, and certain genetic mutations. The hallmark symptom is a persistent dry cough paired with shortness of breath that worsens over time.
How Pirfenidone Works
Pirfenidone is an oral antifibrotic agent that interferes with multiple pathways involved in scar formation. Its main actions include:
- Inhibiting transforming growth factor‑beta (TGF‑β), a key driver of fibroblast activation.
- Reducing collagen synthesis, which limits the buildup of fibrotic tissue.
- Modulating oxidative stress and inflammatory cytokines, helping keep the lung environment less hostile.
By targeting these processes, pirfenidone slows the decline in lung function rather than reversing existing damage.
Clinical Evidence Behind the Claim
The most widely cited data come from the CAPACITY and ASCEND phase III trials, which together enrolled over 1,200 patients worldwide.
- In CAPACITY, the pirfenidone arm showed a 48% reduction in the rate of decline of % predicted FVC over 72 weeks.
- ASCEND confirmed a 44% reduction in FVC decline and a 30% lower risk of disease‑related hospitalization.
- A 2023 real‑world registry from the Australian IPF Network reported a median survival advantage of 1.5 years for patients staying on pirfenidone for at least 12 months.
These results have earned the drug approval from the FDA (2014), EMA (2015), and TGA (2016), and it remains a first‑line option in most international guidelines.

Dosing and Administration
The standard regimen follows a three‑step titration to improve tolerability:
| Week | Dosage (mg per dose) | Frequency |
|---|---|---|
| 1-2 | 267 | Three times daily |
| 3-4 | 534 | Three times daily |
| 5 onward | 801 | Three times daily |
Patients should take the capsules with food and a full glass of water to reduce stomach upset. If a dose is missed, take it as soon as remembered unless it’s near the next scheduled dose-don’t double up.
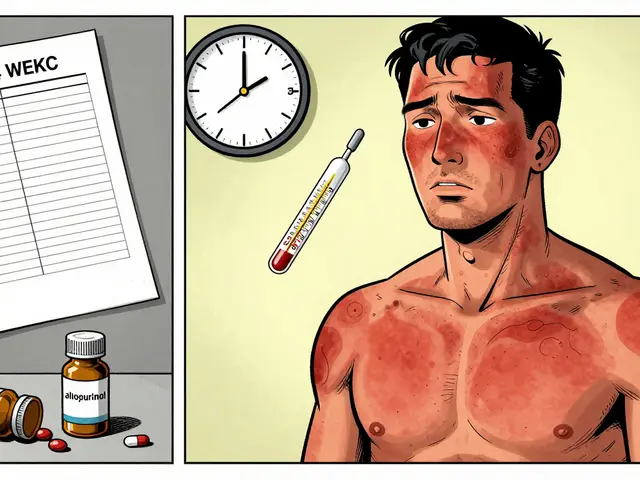
Managing Common Side Effects
Even though pirfenidone is generally well‑tolerated, up to 85% of users report some adverse effect. The most frequent issues are:
- Gastrointestinal: nausea, dyspepsia, loss of appetite. Strategies include small, frequent meals, antacid use, and taking the medication after meals.
- Skin rash or photosensitivity: sun protection (broad‑spectrum SPF 30+) and topical moisturizers help. Severe rash may require a temporary dose reduction.
- Liver enzyme elevation: baseline and quarterly liver function tests are recommended. If ALT/AST rise >3× ULN, pause treatment and re‑evaluate.
Most side effects improve after the titration phase. Open communication with the care team is key-dose adjustments can keep patients on therapy without sacrificing efficacy.
Pirfenidone vs. Nintedanib: Which Is Right for You?
Another antifibrotic, nintedanib, works by blocking multiple tyrosine kinases. Below is a quick side‑by‑side look.
| Aspect | Pirfenidone | Nintedanib |
|---|---|---|
| Mechanism | Inhibits TGF‑β, collagen synthesis, oxidative stress | Blocks VEGFR, FGFR, PDGFR tyrosine kinases |
| Typical Dose | 801 mg three times daily (total 2403 mg) | 150 mg twice daily |
| Efficacy (FVC decline reduction) | ~45% | ~50% |
| Common Side Effects | Nausea, rash, liver enzymes | Diarrhea, liver enzymes, hypertension |
| Take with Food? | Yes | Yes |
| Contraindications | Severe liver disease | Severe hepatic impairment, bleeding risk |
Both drugs slow disease similarly, but individual tolerance and comorbidities often tip the balance. Some clinicians start with pirfenidone for patients who have a sensitive gut, while others prefer nintedanib for those at higher bleeding risk.

Who Is a Good Candidate?
Guidelines suggest offering an antifibrotic to any patient with a confirmed diagnosis of IPF who has a % predicted FVC > 50% and can handle oral medication. Specific considerations include:
- Age: No upper limit, but geriatric patients may need closer monitoring for liver function.
- Comorbidities: Active peptic ulcer disease may worsen with pirfenidone; chronic liver disease may steer the choice toward nintedanib.
- Patient preference: Some prefer a capsule regimen (pirfenidone) over a tablet (nintedanib), or vice versa based on dosing frequency.
In practice, a shared decision‑making session that reviews efficacy, side‑effect profiles, and lifestyle impact leads to better adherence.
Lifestyle, Pulmonary Rehab, and Supportive Care
Medication alone won’t halt fibrosis. Complementary measures that improve quality of life include:
- Enrollment in a pulmonary rehabilitation program - improves exercise tolerance and reduces dyspnea.
- Vaccinations (influenza, COVID‑19, pneumococcal) - prevent infections that can accelerate decline.
- Smoking cessation - even low‑level exposure worsens outcomes.
- Oxygen therapy when resting saturation falls below 88% - can preserve muscle function.
- Regular follow‑up with a multidisciplinary IPF clinic - allows timely assessment of disease trajectory and therapy adjustments.
Integrating these steps with pirfenidone creates a comprehensive plan that maximizes the chance of a slower disease course.
Frequently Asked Questions
How long does it take to see a benefit from pirfenidone?
Most patients notice a stabilization of lung function within 3-6 months, although the full effect on slowing FVC decline becomes clearer after a year of continuous therapy.
Can pirfenidone be taken with other medications?
Yes, but it interacts with strong CYP1A2 inhibitors (e.g., fluvoxamine) and some antacids. Always have a pharmacist review the full medication list.
What should I do if I develop a rash?
Stop the dose temporarily, apply a gentle moisturizer, and avoid direct sun. If the rash persists, contact your doctor for a possible dose reduction.
Is there a generic version of pirfenidone?
As of 2025, patents still protect the branded formulation in most markets, so generics are not widely available yet.
Can I stop pirfenidone if my disease stabilizes?
Stopping abruptly risks a rebound acceleration of fibrosis. Any change should be done slowly under specialist supervision.
Bottom line: pirfenidone offers a proven, oral option to turn the dial down on IPF progression. Pairing it with lifestyle measures, regular monitoring, and open communication with the care team maximizes its benefit.


Ritik Chaurasia
Listen up, the drug is a game‑changer but our healthcare system makes it impossible for most patients in India to even get a prescription because of the sky‑high price tags.
Gary Marks
Honestly, I’m sick of reading the same glossy press releases that chant about "efficacy" while ignoring the brutal reality that a family in Mumbai can’t afford the monthly cost, and doctors are forced to pick between a good drug and a decent salary, which is a tragic choice that nobody should have to make, especially when the studies were funded by the very companies that set the price, making the whole narrative feel like a marketing ploy masquerading as science, and if you ask any patient they’ll tell you the side‑effects feel like a punch in the gut but the financial strain is a constant, unrelenting headache that never leaves you alone.
Vandermolen Willis
Totally get the frustration 😔. The drug does help keep lungs from deteriorating faster, but the cost‑burden is a real barrier for many. Stay strong, community! 🌟
Steven Young
Pirfenidone works but the data is filtered through pharma lenses. Keep an eye on the fine print.
Sireesh Kumar
Everyone loves to quote the CAPACITY trial, yet they forget the real world is messy-patients miss doses, liver enzymes spike, and the drama of managing side‑effects becomes a daily saga that no chart can capture. In the clinic I see people wrestling with nausea while trying to keep up with work, and the emotional toll is palpable. So yes, the drug has a place, but only if you’re ready for the relentless juggling act that follows.
Jonathan Harmeling
It is a moral imperative that we push for broader access to pirfenidone; denying patients this therapy is tantamount to abandoning them to a hopeless fate. We must advocate for insurance coverage and fair pricing.
Mary Keenan
Side effects are just a minor inconvenience compared to the disease.
Kelly Brammer
If the rash gets worse you must halt the drug and call your doctor.
Denver Bright
I tried to find a cheaper version but the patents still lock us out.
Kelli Benedik
🤦♀️ It’s infuriating how pharma keeps us at arm’s length! 😡🌞
cariletta jones
Stay hopeful, every little lung function gain matters!
Kevin Hylant
When you look at the raw numbers from CAPACITY and ASCEND, the reduction in FVC decline hovers around 45 percent, which translates into months of preserved breathing capacity for many patients. The trials enrolled over a thousand participants, giving the data a solid statistical backbone. Moreover, the real‑world registry from Australia shows a median survival advantage of about 1.5 years for those who stick with the drug beyond a year. That’s not just a number; it’s actual time spent with family, traveling, and enjoying hobbies. Side‑effects, while common, are generally manageable with practical tricks: taking the capsules with food, using antacids for nausea, and slathering on sunscreen to tame photosensitivity. Liver enzymes need monitoring, but a pause and dose tweak usually resolves elevations. Compared with nintedanib, pirfenidone offers a slightly different side‑effect profile-less diarrhea, more rash, which some patients find easier to tolerate. The dosage titration-267 mg then 534 mg before reaching 801 mg three times daily-helps the gut adjust, and most people report fewer GI complaints after the ramp‑up period. Cost remains a barrier in many countries, yet some patient‑assistance programs can offset out‑of‑pocket expenses, so it’s worth digging into those options early. In practice, a shared decision‑making session that walks through efficacy, side‑effects, lifestyle compatibility, and financial considerations leads to better adherence. Finally, pairing the medication with pulmonary rehab, vaccinations, and smoking cessation creates a synergistic effect that maximizes quality of life. All in all, pirfenidone is a proven tool in the IPF armamentarium, but its success hinges on attentive monitoring, patient education, and systemic support.