When a cycle feels off - missed periods, heavy flow, or trouble conceiving - many first think about hormones. Yet a silent player often sits behind the scenes: Inflammation is a biological response of immune cells, blood vessels, and molecular mediators to protect tissue from injury or infection. In the reproductive system, this response can tip the delicate balance that drives ovulation and the monthly shedding of the uterine lining. Understanding that link helps women and clinicians spot hidden causes and take actionable steps.
Quick Takeaways
- Both acute and chronic inflammation can disrupt the hypothalamic‑pituitary‑ovarian (HPO) axis.
- Cytokines such as IL‑6 and TNF‑α interfere with follicle‑stimulating hormone (FSH) and luteinizing hormone (LH) release.
- Prostaglandin spikes trigger abnormal uterine contractions, leading to painful periods.
- Conditions like PCOS and endometriosis are, at their core, inflammatory disorders.
- Diet, sleep, and stress management can blunt harmful inflammation and restore regular cycles.
Inflammation: Types and Triggers
Inflammation comes in two flavors. Acute inflammation is a short‑lived, high‑intensity response that peaks within hours and resolves within days. It’s essential for ovulation because the follicle’s rupture mimics a controlled wound, releasing enzymes and inflammatory mediators that allow the oocyte to exit. By contrast, Chronic inflammation drags on for weeks or months, often at low intensity, and can scar tissue, alter hormone signaling, and impair the endometrium’s ability to rebuild after menstruation. Common triggers include obesity, persistent infections, stress, and environmental toxins.
Ovulation and Menstruation - A Hormonal Dance
Ovulation is the release of a mature egg from the dominant ovarian follicle, triggered by a surge of luteinizing hormone (LH). The process relies on a precise timing cascade: the hypothalamus releases gonadotropin‑releasing hormone (GnRH), prompting the pituitary to secrete FSH and LH, which then act on the ovary. Menstruation follows the luteal phase if fertilization does not occur; the corpus luteum regresses, progesterone falls, and the endometrium sheds. Both phases are tightly regulated, and even subtle shifts in inflammatory signals can throw the whole system off‑balance.
Inflammatory Mediators Meet the HPO Axis
The hypothalamic‑pituitary‑ovarian (HPO) axis is the master control circuit that synchronizes brain, pituitary, and ovary. Cytokines-small proteins released by immune cells-act as messengers that can cross the blood‑brain barrier and modulate GnRH neurons. For example, interleukin‑6 (IL‑6) can suppress GnRH pulse frequency, leading to lower FSH levels and suboptimal follicle development. Tumor necrosis factor‑alpha (TNF‑α) has a similar dampening effect, and elevated levels are commonly found in women with irregular cycles.
Prostaglandins are another key group. During follicular rupture, Prostaglandin E2 (PGE2) rises sharply, facilitating blood vessel dilation and matrix breakdown. However, an over‑production of prostaglandins in the uterus drives stronger uterine contractions, causing dysmenorrhea (painful periods) and sometimes excessive bleeding. The balance of PGE2 versus prostaglandin F2α (PGF2α) determines both ovulatory efficiency and menstrual comfort.
Cellular Players: Immune Cells in the Ovary and Endometrium
Macrophages infiltrate the ovarian follicle during the pre‑ovulatory phase, clearing debris and secreting growth factors that support the oocyte. When inflammation stays chronic, these macrophages shift to a pro‑inflammatory (M1) phenotype, releasing reactive oxygen species that damage DNA in the egg. In the endometrium, uterine natural killer (uNK) cells normally help remodel spiral arteries for implantation, but heightened cytokine levels can push them toward a cytotoxic stance, leading to implantation failure or early miscarriage.

When Inflammation Turns Pathological
Two common disorders illustrate the inflammation‑menstruation link.
- Polycystic ovary syndrome (PCOS) is characterized by low‑grade chronic inflammation, insulin resistance, and disrupted LH/FSH ratios. Women with PCOS often show elevated C‑reactive protein (CRP) and higher IL‑6, contributing to anovulation and irregular bleeding.
- Endometriosis involves ectopic endometrial tissue that incites a persistent inflammatory response, leading to pain, heavy periods, and infertility. Lesions produce high levels of prostaglandins and TNF‑α, which not only cause pain but also impair ovulation by altering follicular environments.
Both conditions demonstrate that addressing the inflammatory component can improve ovulatory function and menstrual regularity.
Comparison: Acute vs. Chronic Inflammation Effects on the Cycle
| Aspect | Acute Inflammation | Chronic Inflammation |
|---|---|---|
| Duration | Hours‑days | Weeks‑months |
| Key Mediators | PGE2, histamine | IL‑6, TNF‑α, CRP |
| Effect on Ovulation | Facilitates follicle rupture | Suppresses GnRH, impairs follicle growth |
| Effect on Menstruation | Normal shedding | Heavy bleeding, dysmenorrhea |
| Associated Conditions | Normal ovulatory cycle | PCOS, endometriosis, luteal phase defect |
Managing Inflammation for a Healthier Cycle
Because lifestyle can either fan the flames or douse them, practical steps are essential.
- Nutrition: Emphasize omega‑3‑rich foods (salmon, flaxseed) that lower IL‑6 and TNF‑α. Cut back on refined carbs and trans fats, which spike CRP.
- Exercise: Moderate aerobic activity 150minutes per week improves insulin sensitivity and reduces systemic inflammation markers.
- Sleep: Aim for 7‑9hours; sleep deprivation raises cortisol and IL‑1β, both detrimental to GnRH pulses.
- Stress reduction: Mind‑body practices like yoga or meditation decrease sympathetic tone, lowering catecholamine‑induced cytokine release.
- Targeted supplements: Vitamin D, curcumin, and zinc have modest anti‑inflammatory effects and may improve ovulatory rates in women with PCOS.
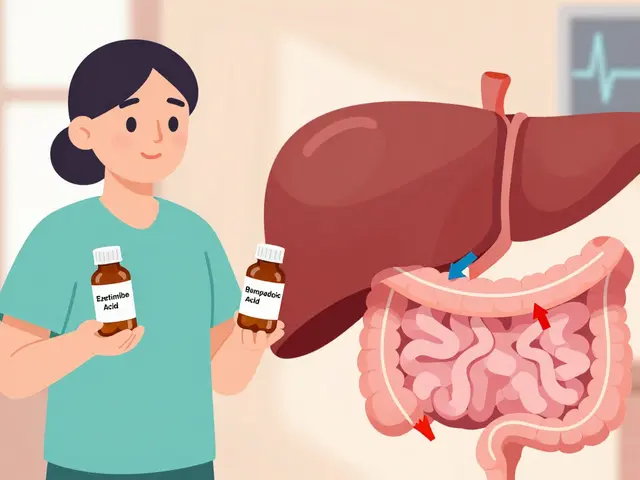
When lifestyle tweaks aren’t enough, clinicians may prescribe anti‑inflammatory agents (e.g., NSAIDs for prostaglandin‑driven dysmenorrhea) or address underlying insulin resistance with metformin, which also lowers inflammatory markers.
Related Topics to Explore
Understanding inflammation’s role opens doors to deeper subjects. The broader field of reproductive immunology examines how the immune system supports conception, implantation, and pregnancy. Narrower topics include the impact of hormonal contraception on cytokine profiles, the use of anti‑TNF biologics in severe endometriosis, and the emerging role of gut microbiome modulation in restoring hormonal balance.
Frequently Asked Questions
Can acute inflammation improve ovulation?
Yes. The brief surge of inflammatory mediators like prostaglandin E2 is a natural part of follicle rupture. It helps break down the follicular wall so the egg can be released. Problems arise only when the inflammation persists beyond the ovulatory window.
Why do women with PCOS often have high C‑reactive protein?
PCOS is linked to insulin resistance, which triggers low‑grade chronic inflammation. The liver responds by producing C‑reactive protein (CRP), a marker that reflects systemic inflammatory load. Elevated CRP correlates with disrupted LH/FSH ratios and anovulation.
How do prostaglandins cause painful periods?
Prostaglandin F2α (PGF2α) contracts uterine muscle to help shed the lining. When PGF2α levels are excessively high, the uterus contracts too strongly, compressing blood vessels and causing cramping and heavy bleeding.
Is there a link between gut health and menstrual inflammation?
A balanced gut microbiome produces short‑chain fatty acids that suppress systemic inflammation. Dysbiosis can raise circulating lipopolysaccharide (LPS), which triggers cytokine release and can disturb the HPO axis, leading to irregular cycles.
Can anti‑inflammatory medication cure endometriosis?
NSAIDs relieve pain by lowering prostaglandin synthesis, but they don’t eliminate the ectopic tissue. Definitive treatment usually requires hormonal therapy or surgery, often combined with diet and lifestyle changes to keep inflammation in check.



Adele Joablife
While the post nails the basic science, it glosses over the fact that many clinicians still ignore inflammation when treating irregular cycles. The cascade of cytokines isn’t just a footnote; it’s a major driver of the HPO dysregulation you described. Too often, patients are handed birth‑control pills without checking CRP or lifestyle factors. A more holistic work‑up would include diet, sleep, and stress assessments right off the bat. Otherwise we’re just patching symptoms instead of addressing the root cause.
kenneth strachan
Wow, so much hype about “inflammation” when the real drama is our daily caffiene‑induced cortisol spikes!
Mandy Mehalko
I love how this breaks down a tricky topic into bite‑size pieces. It’s encouraging to see that lifestyle tweaks can actually shift those cytokine levels. Even a small boost of omega‑3s may calm IL‑6 and make ovulation smoother. Keep reminding folks that consistency beats perfection-sleep a bit more, move a bit more, and don’t stress about the occasional slip‑up. The science is solid, and the optimism is definitely needed. You’re definitely on the right track, just remember to stay patient and keep experimenting!
Bryan Kopp
Interesting read, but let’s not pretend inflammation isn’t just another buzzword for “bad habits”. If we keep blaming hormones without tackling the underlying immune noise, we’ll circle back to the same problems. A bit of restraint in our rhetoric could go a long way. Maybe consider that some of the “pain” comes from our own expectations.
Patrick Vande Ven
The interplay between acute prostaglandin surges and chronic cytokine elevation is often underappreciated in clinical curricula. Acute PGE₂ facilitates follicular rupture, whereas prolonged TNF‑α exposure dampens GnRH pulsatility. Moreover, the shift from M2 to M1 macrophage phenotypes within the follicle can impair oocyte quality via oxidative stress. It is also worth noting that CRP, while nonspecific, provides a useful surrogate for systemic inflammation in the context of PCOS. Integrating these biomarkers into routine assessment could refine therapeutic strategies considerably.
Tim Giles
Delving deeper into the mechanistic pathways, one observes that the hypothalamic‑pituitary‑ovarian axis is exquisitely sensitive to peripheral inflammatory cues. Interleukin‑6, for instance, can cross the blood‑brain barrier and modulate the frequency of GnRH pulses, thereby influencing downstream FSH and LH secretion. Elevated tumor necrosis factor‑α has a comparable suppressive effect, often correlating with anovulatory cycles in women with metabolic syndrome. Chronic low‑grade inflammation, as reflected by heightened C‑reactive protein levels, also impairs insulin signaling, which further aggravates hyperandrogenism and disrupts folliculogenesis. From a cellular perspective, macrophages within the pre‑ovulatory follicle transition from a reparative M2 phenotype to a pro‑inflammatory M1 state when cytokine milieu persists, releasing reactive oxygen species that jeopardize oocyte DNA integrity. In the endometrium, uterine natural killer cells, normally essential for spiral artery remodeling, become cytotoxic under sustained inflammatory pressure, contributing to implantation failure. Prostaglandin synthesis is another critical node; an overabundance of PGF₂α relative to PGE₂ not only intensifies uterine contractions during menstruation but also hampers luteal phase support. Therapeutically, non‑steroidal anti‑inflammatory drugs attenuate prostaglandin production, offering symptomatic relief, yet they do not address the upstream immunological dysregulation. Lifestyle interventions-such as increased omega‑3 fatty acid intake, regular moderate aerobic exercise, and adequate sleep-have been shown to down‑regulate systemic IL‑6 and TNF‑α concentrations, thereby restoring a more favorable hormonal environment. Moreover, emerging evidence suggests that gut microbiota modulation through prebiotic and probiotic supplementation can reduce endotoxin‑mediated inflammation, further supporting HPO axis stability. In clinical practice, a comprehensive assessment that includes inflammatory markers, metabolic parameters, and psychosocial stressors is indispensable for tailoring individualized treatment plans. Ultimately, recognizing inflammation as a central conduit rather than a peripheral side effect can transform management strategies for conditions like PCOS and endometriosis, leading to improved ovulatory function and menstrual regularity.
Peter Jones
That was a thorough breakdown, Tim. I especially appreciate the connection between gut health and cytokine levels; it’s a reminder that we can’t treat the ovary in isolation. Adding a few probiotic‑rich foods could be a low‑risk first step for many.
Gerard Parker
From a practical standpoint, pairing dietary omega‑3s with regular low‑impact exercise tends to lower IL‑6 by about 20 % in most studies. For patients with PCOS, adding a modest dose of vitamin D (1,000–2,000 IU daily) often improves insulin sensitivity and reduces CRP. When NSAIDs aren’t enough for dysmenorrhea, a short course of low‑dose oral contraceptives can suppress prostaglandin synthesis while stabilizing the endometrium. Always remember to reassess inflammatory markers after three months to gauge response.
Thomas Burke
Great tips Gerard you nailed it with the omega‑3 and vitamin D advice it’s simple yet effective
Debbie Frapp
I love how this post ties together immunology and reproductive health in a way that’s both accessible and scientifically accurate. One thing that could be added is a quick checklist for clinicians: check CRP, assess sleep quality, evaluate diet for omega‑3 content, and screen for chronic stressors. This way, the information becomes immediately actionable. Keep up the great work!
Michelle Abbott
Honestly the post rehashes known pathways without offering any novel biomarkers – just the usual IL‑6, TNF‑α, CRP spiel.