Methoxsalen Dose Calculator
Methoxsalen Dose Calculator
Calculate your correct oral methoxsalen dose for PUVA therapy based on your body weight. The standard dose is 0.5 mg/kg body weight.
When you hear the name methoxsalen linked to a flaky, itchy scalp, you might wonder what the connection is. This article walks you through exactly how this photosensitizing drug fits into modern management of seborrheic dermatitis, what you can realistically expect, and how it stacks up against the more familiar creams and shampoos.
What is Methoxsalen?
Methoxsalen is a synthetic furanocoumarin that acts as a photosensitizer, making skin cells more responsive to ultraviolet A (UVA) light during PUVA therapy. Originally developed for vitiligo and psoriasis, its ability to modify DNA replication under controlled UV exposure has made it a niche option for other inflammatory skin disorders.
Understanding Seborrheic Dermatitis
Seborrheic dermatitis is a chronic, relapsing skin condition that primarily affects oily areas like the scalp, eyebrows, and chest and is characterized by erythema, greasy scales, and occasional itching. The exact cause is multifactorial: overgrowth of the yeast Malassezia, an abnormal immune response, and a compromised skin barrier all play a role.
How Methoxsalen Helps Manage Seborrheic Dermatitis
Think of methoxsalen as a catalyst for the skin’s own repair mechanisms. When taken orally (or applied topically in some protocols) and followed by a controlled dose of UVA light, the drug temporarily slows the proliferation of keratinocytes and reduces the inflammatory cascade that fuels flaking. The result is a smoother, less inflamed surface that stays calm longer than with topical steroids alone.
Treatment Protocol: Dosing and UVA Exposure
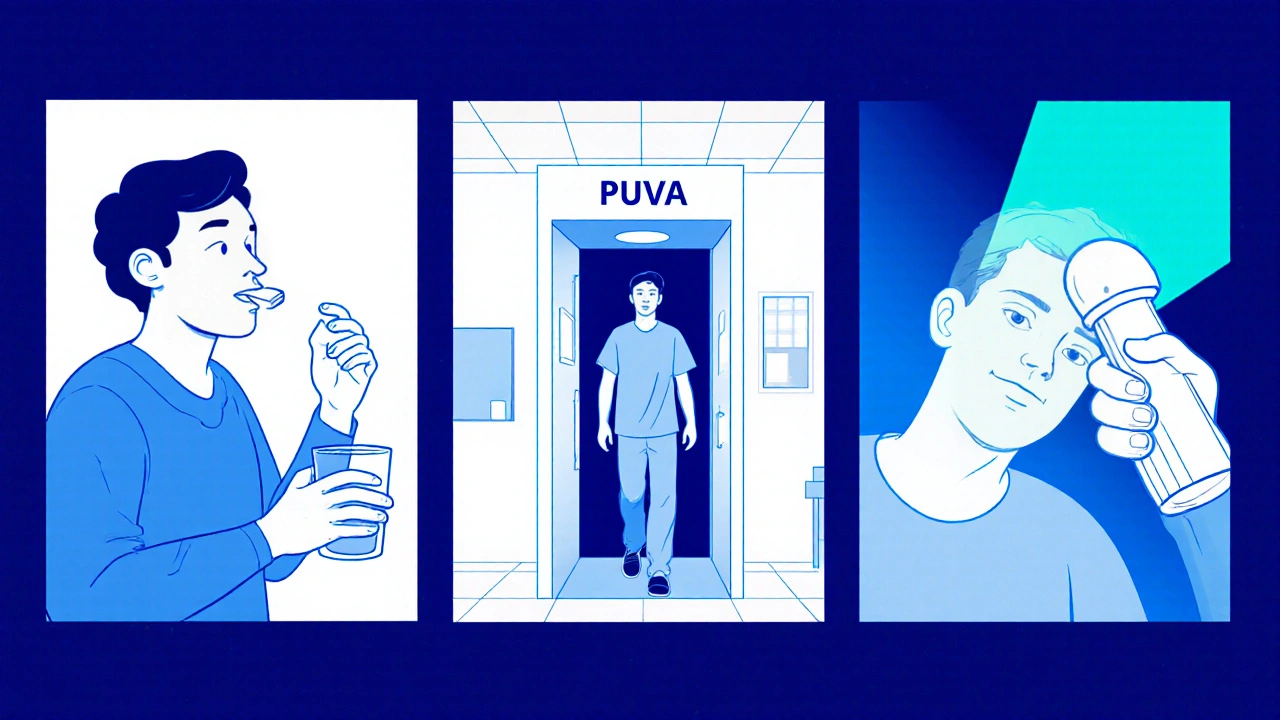
The typical regimen looks like this:
- Take a low oral dose of methoxsalen (usually 0.5mg/kg) about 30 minutes before entering the treatment booth.
- Expose the affected skin to UVA light ranging from 1 to 3J/cm², depending on skin type and prior response.
- Repeat the session 2-3 times per week for 4-6 weeks, then shift to a maintenance schedule of once every 2-4 weeks.
For scalp‑only disease, many dermatologists prefer a PUVA protocol that combines oral methoxsalen with a hand‑held UVA lamp targeting the scalp. This minimizes exposure to uninvolved skin and reduces the risk of phototoxic side effects.
Benefits and Risks
Every treatment has trade‑offs. Here’s a quick rundown of what patients typically report:
- Benefits: Longer remission periods (often 3‑6months), reduced need for daily steroid shampoos, and improvement in both scaling and redness.
- Common side effects: Transient redness after exposure, mild nausea if the oral dose is taken on an empty stomach, and temporary increased skin sensitivity to sunlight.
- Serious concerns: Long‑term PUVA has been linked to a modest rise in skin cancer risk, especially in fair‑skinned individuals. Regular dermatologic screening is a must.
Because the therapy hinges on controlled UV exposure, patients should avoid tanning beds and wear protective clothing on days they aren’t receiving treatment.
How Methoxsalen Stacks Up Against Other Options
Below is a side‑by‑side look at the most common approaches for seborrheic dermatitis. The table focuses on effectiveness, safety, ease of use, and cost.
| Treatment | Typical Effectiveness | Safety Profile | Convenience | Average Cost (AU$) |
|---|---|---|---|---|
| Methoxsalen+PUVA | High (60‑80% clear‑skin after 6weeks) | Moderate - phototoxicity, monitor for skin cancer | Clinic visits 2‑3×week, then maintenance | 1,200‑1,800 (initial series) |
| Topical Steroids | Medium (30‑50% improvement) | Generally safe; risk of skin thinning with long‑term use | Apply daily at home | 150‑300 |
| Antifungal Shampoos | Low‑to‑Medium (20‑40% relief) | Very safe; occasional scalp irritation | Use 2‑3×week, then as needed | 80‑200 |
| Phototherapy (UVA alone) | Medium (40‑60% improvement) | Similar to PUVA but without photosensitizer - lower cancer risk | Clinic visits 2‑3×week | 900‑1,200 |
In plain language, methoxsalen‑PUVA offers the strongest punch but demands more oversight. If you’re looking for a low‑maintenance, side‑effect‑light routine, topical steroids or antifungal shampoos might be your first line, reserving PUVA for stubborn cases.
Practical Tips for Patients Considering Methoxsalen
- Schedule an initial consultation with a dermatologist who has PUVA experience.
- Ask about a baseline skin examination to document any pre‑existing lesions.
- Take the oral dose with food to reduce nausea.
- Wear sunglasses during and after treatment to protect eyes from UV exposure.
- Keep a simple diary of flare‑ups, side effects, and treatment dates - this helps fine‑tune the regimen.
Remember, the goal isn’t a one‑time cure but a longer stretch between flare‑ups. Combining methoxsalen with a gentle, non‑comedogenic cleanser and occasional moisturizer can extend the benefits.
Frequently Asked Questions
Is methoxsalen safe for long‑term use?
Long‑term PUVA does carry a modest increase in skin cancer risk, so most clinicians limit the total number of sessions and schedule regular skin checks. For most patients, a 6‑week course followed by maintenance every few months balances safety and benefit.
Can I use methoxsalen at home?
Home administration is possible with a portable UVA device, but it requires strict dosing guidelines and a prescription. Most practitioners prefer in‑clinic treatment to control UV dose precisely.
How quickly will I see results?
Many patients report noticeable reduction in redness and scaling after 2-3sessions, with near‑clear skin by the end of the 4‑week series. Individual response varies based on severity and skin type.
Are there alternatives if I’m afraid of UV exposure?
Yes. Topical corticosteroids, calcineurin inhibitors, and antifungal shampoos are all UV‑free options. They tend to be less potent for severe cases but have a simpler safety profile.
Do I need to stop other skincare products while on methoxsalen?
Avoid retinoids, benzoyl peroxide, or any other photosensitizing agents during treatment, as they can amplify UV reactions. A gentle cleanser and fragrance‑free moisturizer are safe choices.



Miriam Rahel
While methoxsalen demonstrates notable efficacy in refractory seborrheic dermatitis, the attendant phototoxicity and oncogenic potential necessitate vigilant monitoring.
Malia Rivera
In the grand tapestry of dermatologic therapy, the interplay of ultraviolet photons and a sensitizing molecule like methoxsalen mirrors humanity’s quest to harness nature’s fire, yet we must temper ambition with prudence. Our nation’s medical community should champion such innovations while safeguarding the skin of its citizens.
lisa howard
I have been tracking the evolution of photochemotherapy for years, and methoxsalen’s reemergence in seborrheic dermatitis feels like a dramatic encore on a stage once thought closed.
The drug’s furanocoumarin backbone, once the darling of vitiligo clinics, now steps into the greasy, flaky arena of Malassezia‑driven inflammation.
When patients ingest the modest 0.5 mg/kg dose, the bloodstream becomes a sensitized canvas awaiting the precise brushstroke of UVA light.
The subsequent photochemical reaction temporarily arrests keratinocyte hyperproliferation, granting the epidermis a reprieve from its own overzealous turnover.
This reprieve translates clinically into reduced erythema, softened scales, and a calming of the relentless itch that haunts many sufferers.
Of course, the protocol demands strict timing-half an hour after the pill, the patient steps into the PUVA booth, eyes shielded, skin exposed.
Sessions repeat two to three times weekly, a rhythm that can feel demanding but ultimately builds a longer remission than steroid shampoos alone.
The long‑term specter of photocarcinogenesis looms, reminding clinicians that cumulative UVA doses must be tracked with the same diligence as any chemotherapy.
In practice, I advise my patients to maintain a skin‑cancer screening calendar, noting each PUVA encounter on a dedicated diary.
Moreover, the convenience factor cannot be ignored; clinic visits twice weekly can clash with work schedules, especially for those without flexible hours.
Some dermatologists mitigate this by employing hand‑held UVA lamps focused on the scalp, sparing the rest of the body from unnecessary exposure.
The cost, while higher than over‑the‑counter shampoos, often proves justified when patients break free from the cycle of monthly flare‑ups.
Anecdotally, I have observed patients who, after completing a six‑week series, enjoy three to six months of clear skin before any resurgence.
Yet, not every individual responds; skin type, baseline disease severity, and even genetic factors modulate the ultimate outcome.
Ultimately, methoxsalen represents a potent weapon in the dermatologist’s armamentarium, but it must be wielded with precision and respect for its double‑edged nature.
As always, shared decision‑making between physician and patient remains the cornerstone of safe and effective therapy.
Cindy Thomas
Even though the drama around methoxsalen’s UV tango is captivating, the data still suggest that many patients achieve comparable relief with simpler antifungal shampoos 😊. It’s hard to justify the clinic visits and potential skin‑cancer risk when a low‑cost ketoconazole wash can calm most flares :-) . Still, I acknowledge that severe cases may need that extra punch, but the trade‑off feels disproportionate.
Kate Marr
Methoxsalen + PUVA is a bold move, 🇺🇸 style, bringing high‑tech care to stubborn scalp issues. The results can be impressive, but remember the sun‑safety game is real 🌞. If you’re ready to commit to the schedule, the payoff might just be worth the effort.
James Falcone
Look, if we’re talking about cutting‑edge skin care, the US knows how to push forward, but we shouldn’t forget cheaper home remedies that work for most folks. Those clinic trips can drain wallets fast.
Frank Diaz
One could argue that the very act of sensitizing skin to UV light is a metaphor for humanity’s willingness to invite danger for fleeting beauty; yet, embracing methoxsalen without rigorous follow‑up betrays a hubristic disregard for long‑term health.
Nickolas Mark Ewald
I get your point, and I think using methoxsalen works if the doctor watches the patient closely.
Chris Beck
It’s good!It works!But many ignore the risks!!!You need real data, not hype.
Winston Bar
Honestly, the hype around methoxsalen is overrated-most people could just stick to cheap shampoos and be fine.
Russell Abelido
I hear you, but for those battling relentless flares, that “just shampoo” line can feel like a punch in the gut 😢. A well‑managed PUVA course has actually changed lives, giving someone back weeks of confidence. Let’s not dismiss the option for folks who need that extra relief.