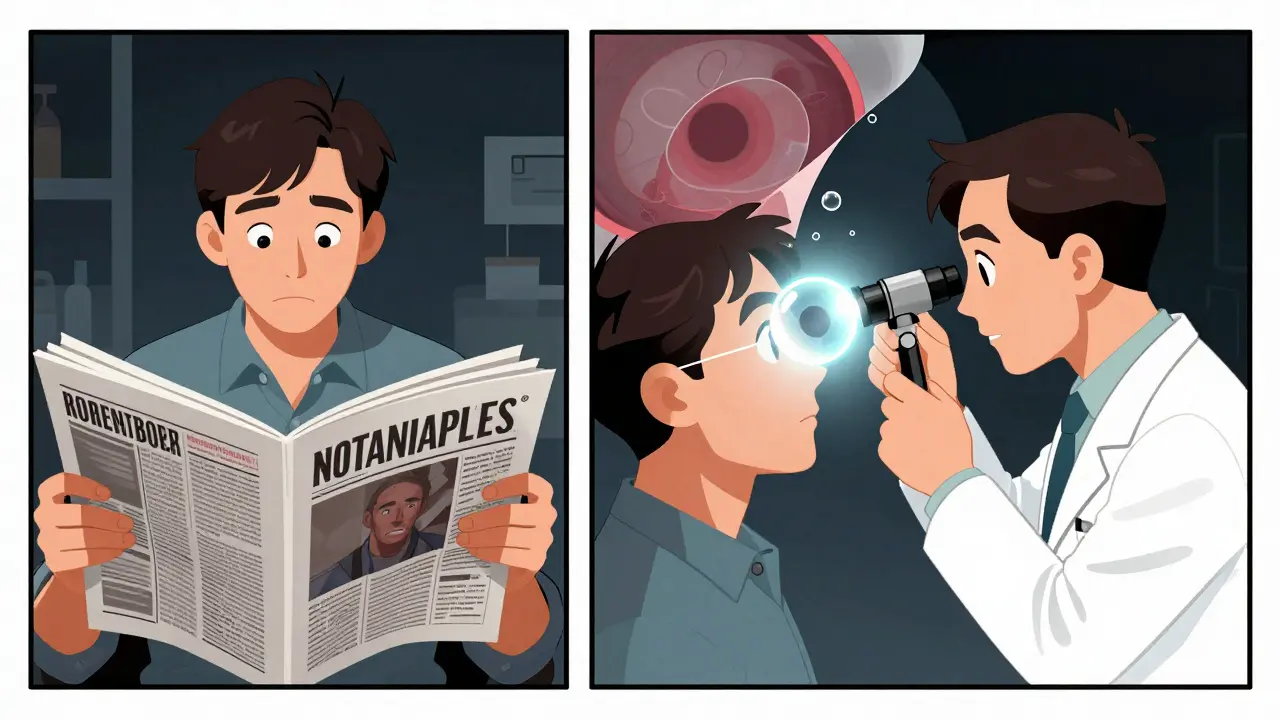
One moment your vision is clear. The next, a dark curtain is creeping across your eye like a shadow pulling over a window. You see flashes of light, like lightning in the corner of your vision, and a storm of new floaters swirls in front of you. It doesn’t hurt. There’s no redness. But something is very, very wrong. This isn’t just eye strain. It’s not aging. It’s retinal detachment - and every minute counts.
What Exactly Is Retinal Detachment?
The retina is the thin layer of tissue at the back of your eye that captures light and sends signals to your brain. Think of it like the film in an old camera - if it peels away from the wall behind it, the image goes dark. Retinal detachment happens when this layer pulls loose from its blood supply. Without immediate treatment, the light-sensitive cells start dying. Permanent vision loss can happen in hours, not days.It’s not rare. About 1 in 10,000 people experience it each year. But if you’re nearsighted (more than -5.00 diopters), have had cataract surgery, or have lattice degeneration - thin, weak spots in the retina - your risk jumps dramatically. In fact, people with lattice degeneration have a 1 in 100 chance of detachment over their lifetime. Age also plays a role: after 40, your risk doubles.
The Six Warning Signs You Can’t Afford to Ignore
Most people don’t realize these symptoms are an emergency. They think, "It’s just floaters," or "I’m tired." But here’s what you need to know:- Sudden increase in floaters - Not just one or two. Dozens. Dark spots, squiggles, or cobwebs that appear out of nowhere. The National Eye Institute says patients describe it as "a lot of new floaters" appearing in just hours.
- Flashes of light - Like camera flashes or streaks of lightning, especially in your peripheral vision. These aren’t afterimages from looking at a bright screen. They’re caused by the retina being tugged.
- A dark curtain or shadow - This is the most urgent sign. It starts at the edge of your vision and slowly moves inward, like a shade being pulled across a window. If it reaches the center, you’re losing central vision.
- Blurry or distorted vision - Words on a page look wavy. Faces look stretched. This happens in nearly 7 out of 10 cases, according to Cleveland Clinic data.
- Loss of peripheral vision - You can’t see things to your side. It’s not just tunnel vision - it’s a missing piece of your visual field.
- Sudden color changes - Colors look duller or washed out, especially if the macula (the center of the retina) is involved. This is a late but critical signal.
Don’t wait. Don’t call your optometrist tomorrow. Go to an emergency eye clinic today. A 2022 study in the Journal of VitreoRetinal Diseases found that if surgery happens within 24 hours of symptoms, there’s a 90% chance the retina can be successfully reattached. After 72 hours, your chance of regaining 20/40 vision drops from 75% to 35%.
How Doctors Diagnose It - Fast
There’s no home test. No app. You need an eye specialist with the right tools. Here’s what happens in a real emergency clinic:- Dilated fundus exam - Drops widen your pupil. The doctor uses a bright light and a special lens (like a 20D indirect ophthalmoscope) to look deep into your eye. This is the gold standard.
- B-scan ultrasound - If your eye is cloudy from cataracts or bleeding, sound waves create an image of the retina. It’s quick, painless, and tells the doctor if the retina is floating away.
- Optical coherence tomography (OCT) - This non-invasive scan takes a high-res cross-section of the retina. It shows exactly where and how far the detachment has spread.
General ophthalmologists miss about 22% of early cases. Retinal specialists get it right 95% of the time. That’s why timing matters - if your local clinic doesn’t have a retinal specialist on call, go to a hospital with an eye emergency department. Wills Eye Hospital’s protocol requires evaluation within 4 hours for macula-off detachments. Don’t waste time.
The Three Main Surgical Options - What Works Best?
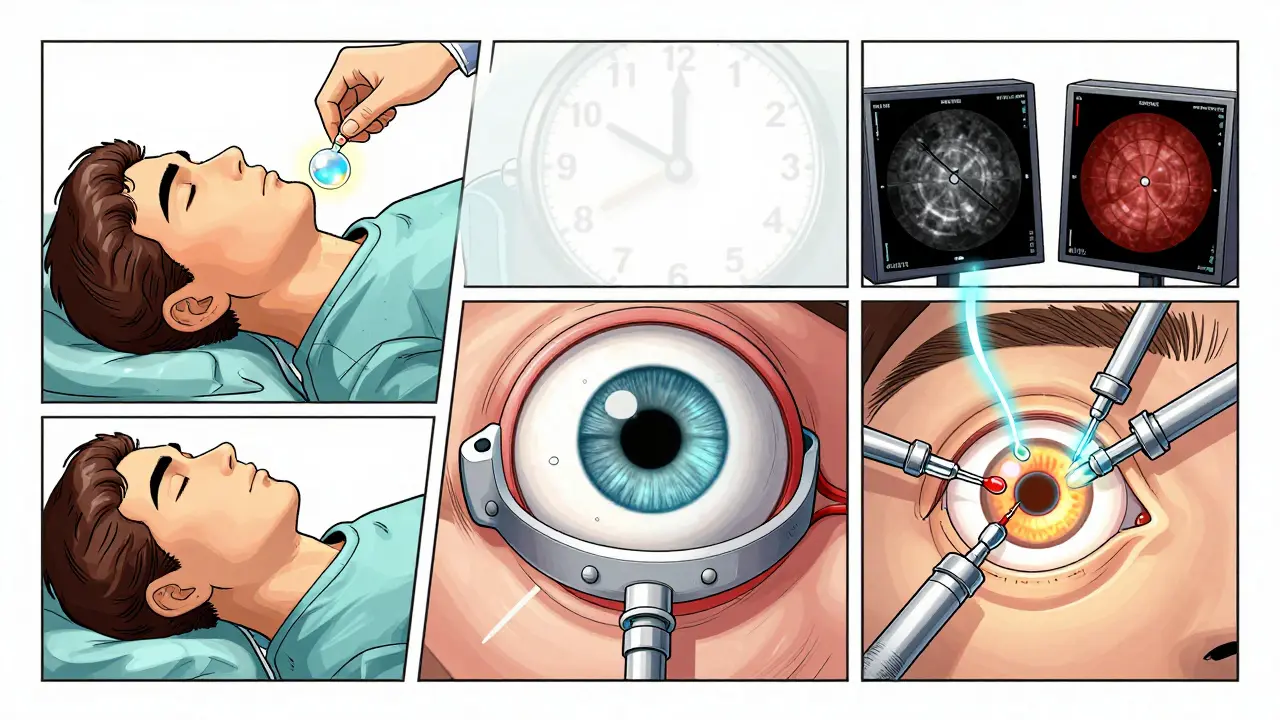
There’s no one-size-fits-all fix. The right surgery depends on where the tear is, how big it is, and whether the macula is still attached.1. Pneumatic Retinopexy
This is the least invasive. A gas bubble is injected into your eye. You’re told to lie face-down or on your side so the bubble floats up and presses the retina back into place. Then, a laser or freezing treatment seals the tear.
Best for: Single, small tears near the top of the retina in people who still have their natural lens.
Success rate: 70-80%
Downside: You have to stay in a specific position for 7-10 days - 50 out of every 24 hours. That’s hard. Many patients report back pain, neck strain, and sleepless nights. And if the tear is on the bottom of the retina, this won’t work at all.
2. Scleral Buckling
A silicone band is sewn around the outside of your eyeball. It gently pushes the wall of the eye inward to meet the detached retina. It’s like putting a belt around your eye to hold everything in place.
Best for: Younger patients, those with lattice degeneration, or detachments caused by trauma.
Success rate: 85-90%
Downside: It can cause nearsightedness (1.5-2.0 diopters), double vision, or discomfort. But it doesn’t speed up cataracts - a big plus if you’re under 50.
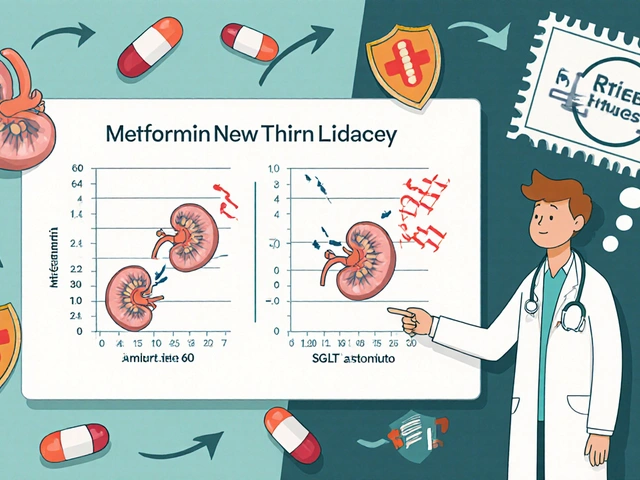
3. Vitrectomy
This is the most common surgery today. The surgeon removes the gel-like vitreous from inside your eye and replaces it with saline, gas, or silicone oil. Then they use lasers to seal the tear and reattach the retina.
Best for: Complex cases - large tears, scar tissue, or if the macula is already detached.
Success rate: 90-95%
Downside: Almost all patients who still have their natural lens will develop a cataract within two years. You’ll need cataract surgery later. But if your vision is already at risk, this is the best way to save it.
A 2022 Cochrane Review found vitrectomy gives better results than scleral buckling when the macula is involved. If you’re over 50 and your vision is fading, vitrectomy is usually the go-to.
What Happens After Surgery?
Recovery isn’t quick. You’re not just healing - you’re retraining your eye.- If you had a gas bubble, you must keep your head in a specific position for days. No lying flat. No looking up. Some patients use special pillows or even sleep in recliners.
- You can’t fly until the gas is gone. Even a small change in altitude can cause the gas to expand and damage your eye.
- Expect blurry vision for weeks. Colors may look off. Your eye might be red and swollen.
- Follow-up visits are critical. Recurrent detachment happens in 5-15% of cases, especially if scar tissue forms.
One in three patients need help at home during recovery. That’s why planning ahead matters - arrange for someone to drive you, cook for you, and remind you to stay in position.
Why Speed Is Everything
Dr. Carl Regillo from Wills Eye Hospital says, "Every hour counts." The longer the retina is detached, the more photoreceptor cells die. And those cells don’t come back.Patients who get treated within 12 hours report 92% satisfaction with their vision recovery. Those who wait 48 hours? Only 67%. One Reddit user, "VisionWarrior22," ignored symptoms for three days. His final vision was 20/100 - he couldn’t read street signs or recognize faces. He says, "I thought it was just aging. I didn’t know it could be fixed if I’d acted sooner."
And here’s the scary part: 63% of patients in one survey were first told they had "eye strain" by their primary care doctor. That’s a dangerous delay. If you have these symptoms, insist on seeing an eye specialist immediately. Don’t take "wait and see" as an answer.
What’s New in Treatment?
The field is moving fast. In January 2023, the FDA approved the EVA Platform - a 27-gauge vitrectomy system that uses smaller incisions. Less trauma. Faster healing.Surgeons now use intraoperative OCT - real-time imaging during surgery - to see exactly how well the retina is reattaching. One study showed this improved scar tissue removal by 15%.
Future treatments are even more exciting. Bioengineered retinal patches are in clinical trials. Gene therapies are being tested for inherited conditions that weaken the retina. In five years, AI tools might scan your eye photos and flag early signs of detachment before you even notice symptoms.
Who’s at Risk - And What You Can Do
You can’t prevent all detachments. But you can reduce your risk:- If you’re severely nearsighted, get annual eye exams.
- If you’ve had cataract surgery, watch for flashes or floaters - your risk is higher.
- If you have lattice degeneration, ask your doctor about preventive laser treatment. Some experts recommend it; others say the risk of surgery outweighs the benefit. Talk to a retinal specialist - don’t guess.
- Wear protective eyewear during sports or work that could cause eye trauma.
Most importantly: know the signs. If you see them - act. Don’t wait. Don’t hope it goes away. Your vision isn’t something you can afford to gamble with.
Can retinal detachment fix itself?
No. Retinal detachment cannot fix itself. The retina needs to be physically reattached through surgery. Without treatment, the detached area will continue to lose function, leading to permanent blindness in that part of your vision. Even if symptoms seem to improve, the underlying problem remains. Delaying treatment only increases the risk of irreversible damage.
Is retinal detachment painful?
No, retinal detachment is typically not painful. There’s no inflammation or pressure that causes discomfort. That’s why many people ignore the symptoms - they don’t feel sick. The only signs are visual: floaters, flashes, or a shadow. This makes it even more dangerous. You can’t rely on pain to tell you something’s wrong. Trust your vision.
How long does recovery take after retinal surgery?
Recovery varies by procedure. For pneumatic retinopexy, you’ll need to maintain a specific head position for 7-10 days. Full visual recovery can take weeks to months. Vitrectomy patients often see gradual improvement over 4-6 weeks, but it can take up to six months for vision to stabilize. Cataracts may develop within two years, requiring additional surgery. Patience and follow-up care are key.
Can I drive after retinal detachment surgery?
No, not immediately. If you had a gas bubble injected, you cannot drive until the gas is completely absorbed - which can take 2-8 weeks depending on the type. Even after the gas is gone, your vision may still be blurry or distorted. Your doctor will give you a timeline, but most patients wait at least 2-4 weeks before driving again. Never drive if your vision is impaired.
Will I need glasses after surgery?
You may. Scleral buckling can cause new nearsightedness. Vitrectomy often leads to cataracts, which require glasses or lens replacement. Even if your prescription doesn’t change, your eyes may take time to adjust. Many patients need new glasses 3-6 months after surgery, once vision stabilizes. Don’t rush into buying new lenses - wait for your doctor’s final checkup.
Can retinal detachment happen again?
Yes. About 5-15% of patients experience a recurrent detachment, especially if scar tissue forms (called proliferative vitreoretinopathy). People with high myopia or a history of trauma are at higher risk. That’s why regular eye exams are crucial - even years after surgery. Catching a new tear early can prevent another full detachment.
What to Do Right Now
If you’re reading this and you’ve noticed any of those six symptoms - even just one - don’t wait. Don’t check online forums. Don’t call your GP. Go to the nearest eye emergency department or call an ophthalmologist who specializes in retina. Bring someone with you. Write down when the symptoms started. Take a photo of your vision if you can - some clinics use it to track changes.Your eyesight is irreplaceable. Retinal detachment isn’t a "maybe." It’s a "now or never." The technology to save your vision exists. What you do in the next 24 hours could mean the difference between seeing your grandchild’s face - or never seeing it clearly again.


LALITA KUDIYA
I had a floaters scare last year. Went to the clinic thinking it was just stress. Turned out to be a tiny tear. Laser fixed it in 10 minutes. Don't wait like I did. Your eyes don't call for help. They just quit.
Rachel Steward
This post is basically a fearmongering ad for retina specialists. You know who profits when people panic? The ones charging $800 for a 15-minute OCT scan. Most floaters are harmless. Most flashes are vitreous syneresis. The medical-industrial complex thrives on ignorance. You don't need to rush to an emergency room for every flicker in your periphery. Let the system profit from your anxiety.
Anthony Capunong
I work in a VA hospital. Saw 3 cases last month alone. One guy waited 5 days because he thought it was "just old eyes." Lost 80% of his vision. We don't have time for "maybe" in this country. If you're in the US and you see that shadow? Get to a hospital. No excuses. Your vision is a national asset.
Elen Pihlap
I read this and cried. My mom lost her vision like this. She thought it was her glasses. She didn't go because she was scared of the cost. Now she can't see my kids. Don't be like her. Please.
Mina Murray
The FDA approved the EVA Platform? That's a front for Big Pharma. They want you to believe new tech saves you. But they won't tell you the gas bubbles they inject are made with proprietary compounds that degrade faster than natural vitreous. You're being sold a lie wrapped in FDA approval. Ask for the full ingredient list before surgery. No one will give it to you.
Poppy Newman
I had a vitrectomy last year 😢 It was rough. The head positioning was the worst part. I slept in a recliner for 10 days. But I can see my cat again 🐱✨ So worth it. Don't wait. Seriously.
Sai Ganesh
In India, we don't have retinal specialists in every town. Many people wait weeks. But if you're in Delhi or Mumbai, go to LVPEI or Sankara Nethralaya. They have the tech. I know a man who got treated in 14 hours. Now he drives again. It's possible. Just don't delay.
steve rumsford
I'm not even kidding. I saw a flash. Thought it was my phone glitching. Ignored it for 3 days. Then the curtain came. I was in the ER by midnight. Vitrectomy next day. Now I'm 20/25. But man. I lost 2 weeks of my life just lying face down like a confused turtle. Don't be me.
Katrina Morris
I'm so glad this was shared. My cousin is 32 and nearsighted. She didn't know she was high risk. Now she gets annual scans. I told her: your eyes are your only pair. You don't get extras. I'm just happy she's listening now. 💛
Andrew N
The 90% success rate is misleading. That's for reattachment. Not vision recovery. 70% of people who get reattached still have 20/80 or worse. The article hides that. They want you to think you'll be fine. But you won't. You'll be blurry. You'll need glasses. You'll need cataract surgery. They don't tell you that part.