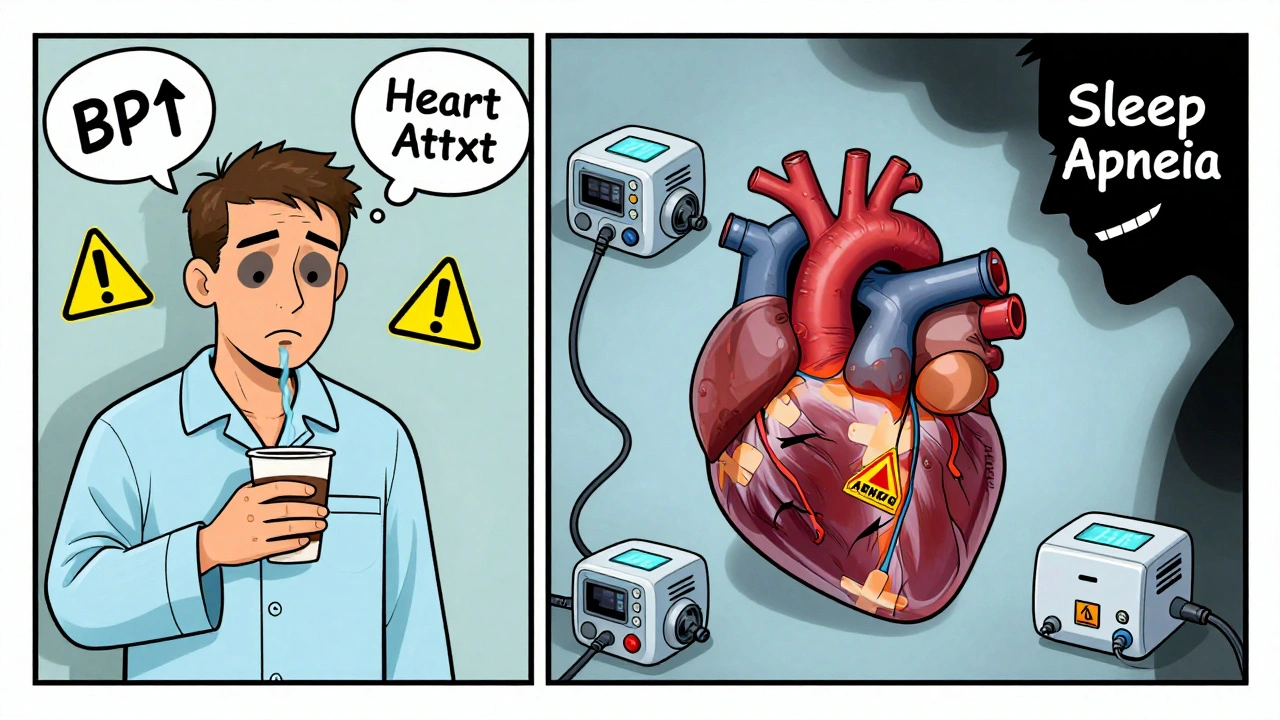
When you stop breathing for 10 seconds-dozens of times a night-you’re not just snoring. You’re putting your heart at serious risk. Sleep apnea isn’t just a nuisance; it’s a silent driver of high blood pressure, heart attacks, and strokes. And most people don’t even know they have it.
What Sleep Apnea Actually Does to Your Body
Sleep apnea means your airway collapses or your brain stops telling your body to breathe while you sleep. Obstructive sleep apnea (OSA), the most common type, happens when throat muscles relax too much and block airflow. This isn’t just about feeling tired in the morning. Every time you stop breathing, your oxygen drops. Your heart races. Your blood pressure spikes. And this cycle repeats-sometimes 30, 50, or even 100 times an hour.
The body reacts like it’s under attack. Stress hormones flood your system. Your sympathetic nervous system goes into overdrive, pumping out adrenaline and noradrenaline at two to four times the normal rate during sleep. That’s not normal. That’s your body screaming for air. And over years, this constant stress rewires your cardiovascular system.
Why Your Blood Pressure Won’t Go Down
If you’ve been told your blood pressure is high-and nothing seems to help-it might not be your diet or stress. It might be sleep apnea.
Up to 80% of people with resistant hypertension (blood pressure that stays high even after taking three different medications) have undiagnosed sleep apnea. That’s not a coincidence. In fact, people with moderate to severe sleep apnea are two to three times more likely to develop high blood pressure within just four to five years.
What makes it worse? Your blood pressure doesn’t drop at night like it should. In healthy people, blood pressure falls 10-20% during sleep. But in 70-80% of sleep apnea patients, it barely drops at all-or even rises. This is called non-dipping, and it’s one of the strongest predictors of heart damage and stroke. Your heart never gets a break. It’s working overtime, all night, every night.
Heart Attacks and the Midnight Window
Heart attacks don’t just happen randomly. In people with sleep apnea, 26.5% of heart attacks occur between midnight and 6 a.m.-nearly 10 percentage points higher than in people without the condition. Why then? Because that’s when apnea episodes peak. Oxygen levels crash. Blood pressure surges. The heart is under maximum strain.
People with moderate to severe sleep apnea have a 30% higher chance of having a heart attack. The risk of dying from coronary disease jumps by 60%. And the worse the apnea, the higher the risk. One study found that those with an Apnea-Hypopnea Index (AHI) of 15 or more had a 1.6 times greater risk of fatal heart events.
This isn’t theoretical. It’s measured in real people. A 2024 analysis of nearly 10,000 adults showed that sleep apnea doesn’t just add risk-it accelerates heart disease, especially in younger adults. People aged 20 to 40 with sleep apnea were 45% more likely to have high blood pressure and 25% more likely to have metabolic syndrome than their peers without it. For older adults, the effect was much smaller. Sleep apnea isn’t just aging-it’s accelerating it.
Heart Failure, Stroke, and the Silent Link
Heart failure and sleep apnea are a dangerous pair. Nearly half of all heart failure patients also have sleep apnea. And if you have sleep apnea, your chance of developing heart failure jumps by 140%. It’s a two-way street: your heart weakens, which worsens breathing, which weakens your heart even more.
Stroke risk is even more alarming. Sleep apnea increases your chance of having your first stroke by 2.5 times. If you’ve already had one, your risk of another goes up by 3.2 times. And the more your oxygen drops at night, the deadlier it becomes. If your oxygen saturation falls below 90% for more than 12% of your sleep, your risk of dying from stroke triples.
And then there’s atrial fibrillation-the most common irregular heartbeat. People with sleep apnea are two to four times more likely to develop it. In fact, nearly half of all patients with intermittent AFib have undiagnosed sleep apnea. And here’s the kicker: if you have AFib and sleep apnea, your chances of a successful ablation drop by 30%. Your heart rhythm won’t stabilize until you treat the root cause: your breathing.
Why CPAP Isn’t a Magic Bullet
Continuous Positive Airway Pressure (CPAP) is the most common treatment. It keeps your airway open with gentle air pressure. It works. But not always the way people expect.
CPAP lowers blood pressure-only by 2 to 3 mmHg on average. That’s not much. But it’s not about the number. It’s about what it prevents. CPAP reduces stroke recurrence by 37%. It improves heart failure outcomes. It makes AFib treatments more effective. It lowers inflammation, improves blood vessel function, and reduces oxidative stress-all of which damage your heart over time.
But here’s the problem: only 46% of people using CPAP actually stick with it. They don’t wear it enough. They don’t use it long enough. If you’re not using it at least four hours a night, seven nights a week, you’re not getting the benefit. And your heart keeps paying the price.
Who Should Be Screened-And When
If you have any of these, you should be tested for sleep apnea:
- High blood pressure, especially if it’s hard to control
- Heart failure
- Atrial fibrillation
- Stroke or TIA (mini-stroke)
- Coronary artery disease
- Obesity
- Snoring, gasping at night, or daytime exhaustion
Doctors are starting to use simple tools like the STOP-Bang questionnaire. It asks about snoring, tiredness, observed breathing pauses, high blood pressure, BMI, age, neck size, and gender. It catches 84% of moderate-to-severe cases. It’s fast. It’s free. And it’s now recommended by cardiologists everywhere.
And if you’re under 40 and you’re overweight and tired all the time? Don’t brush it off as stress or laziness. Sleep apnea is likely the real culprit-and it’s already damaging your heart.
The Bigger Picture
One in five adults has moderate to severe sleep apnea. And it’s rising-by 5% every year-mostly because of obesity. Yet 80% of those cases go undiagnosed. That means millions of people are walking around with a ticking time bomb in their chest, unaware.
This isn’t just a sleep problem. It’s a cardiovascular emergency. Your heart doesn’t care if you think you’re just a loud snorer. It feels every drop in oxygen. Every surge in pressure. Every spike in stress hormones.
Treating sleep apnea isn’t optional if you have heart disease. It’s part of the treatment plan. Just like taking your blood pressure meds or quitting smoking. If you’re not being screened, you’re not getting full care.
The good news? Fixing your breathing can reverse some of the damage. Blood vessels can heal. Inflammation can drop. Your heart can rest. But only if you act.
Don’t wait for a heart attack. Don’t wait for your doctor to ask. If you’re tired, snore, or have high blood pressure-get checked. Your heart will thank you.




Jessica Baydowicz
Okay but like… have you ever tried CPAP? It’s not as bad as people make it sound. I was skeptical too-until I started using it and suddenly I wasn’t waking up gasping like a fish on a dock. My husband said I stopped sounding like a chainsaw in the bedroom. Best. Sleep. Ever.
Now I actually look forward to bedtime. Who knew?
Also, my blood pressure dropped without me even trying. Magic? Nah. Just oxygen.
Shofner Lehto
It’s staggering how many people with resistant hypertension are never screened for sleep apnea. This isn’t a niche issue-it’s a systemic blind spot in cardiology. The data is overwhelming. We’re treating symptoms while ignoring the root cause, and it’s costing lives. Screening should be standard, not optional.
Yasmine Hajar
I’m a nurse and I’ve seen this firsthand. A 38-year-old guy came in after a mini-stroke. No diabetes. No smoking. No family history. Just loud snoring and ‘always tired.’ We tested him-AHI of 42. He cried when he found out it wasn’t just ‘being lazy.’
He started CPAP. Three months later, he ran his first 5K. I cried too.
You think it’s just snoring? It’s your heart screaming for help. Listen.
And if you’re reading this and you’re tired all the time? Get checked. Please.
Karl Barrett
The pathophysiology here is fascinating. The intermittent hypoxia triggers a cascade of sympathetic overactivation, endothelial dysfunction, and systemic inflammation-all of which are biomarkers for accelerated cardiovascular aging. The non-dipping circadian pattern isn’t just a clinical curiosity; it’s a predictor of target organ damage at the microvascular level.
What’s underappreciated is the role of oxidative stress in remodeling the left ventricle over time. CPAP doesn’t just improve compliance-it modulates redox balance. This isn’t anecdotal. It’s molecular.
Jake Deeds
Wow. So people who snore are basically just… lazy? And now we’re blaming their heart disease on not wearing a mask to bed? I mean, I get it, but let’s not pretend this is some grand medical revelation.
Also, if you’re overweight and tired, maybe don’t eat 12 tacos a day and then blame your breathing? Just a thought.
CPAP is expensive and uncomfortable. Maybe the real solution is… not being a couch potato?
val kendra
Snoring isn’t cute. It’s not funny. It’s not just your husband being loud.
It’s your body failing to keep you alive while you sleep.
My dad died of a heart attack at 52. He snored. He had high BP. He never got tested.
Don’t be him.
Get checked.
Now.
And if you’re scared of CPAP? Try a mouthpiece first. Or lose weight. Or both.
Your heart doesn’t care how you feel about it.
It just wants to keep beating.
Give it a chance.
Isabelle Bujold
As someone who’s lived with moderate sleep apnea for over a decade, I want to add something the article doesn’t emphasize enough: the mental toll. It’s not just the physical strain-it’s the exhaustion that makes you snap at your kids, forget appointments, lose motivation to exercise, and feel like you’re drowning even when you’re lying down.
CPAP saved my marriage. My wife said I stopped being a zombie at 8 p.m.
And yes, it’s annoying. The mask leaks. The hose tangles. The machine beeps. But it’s the difference between surviving the day and actually living it.
If you’re on the fence-try it for a week. Even three nights. You’ll know.
And if your doctor won’t refer you? Go to a sleep clinic yourself. They’ll test you. No referral needed in Canada.
Your future self will thank you.
George Graham
I used to think sleep apnea was just for older, overweight guys. Then my sister-32, fit, yoga instructor-got diagnosed after passing out at work. Turns out, her neck was just shaped differently. Her airway collapsed even though she wasn’t overweight.
It’s not about looks. It’s about anatomy. And it’s not rare. It’s just ignored.
If you’re tired, even if you’re ‘healthy,’ get checked. It’s not weakness. It’s wisdom.
John Filby
Just got my sleep study results last week-AHI 28. Was in denial for years. Thought I just needed more coffee. 😅
Started CPAP 3 nights ago. Slept like a baby. Woke up without my head feeling like a lead balloon.
Also, my girlfriend said I stopped sounding like a dying walrus. That’s a win.
Still hate the mask but… worth it.
Anyone else feel like a robot with a hose?
Elizabeth Crutchfield
i had no idea this was a thing until my bro had a stroke at 41. he snored so loud the neighbors complained. he thought he was just a heavy sleeper. turns out he was barely breathing. now he uses cpap and its like a whole new person. dont wait til its too late.
Ben Choy
My mum had sleep apnea and didn’t know it for 15 years. She thought she was just ‘getting old.’ Then she had a mini-stroke. Turns out her oxygen was dipping below 80% for minutes at a time.
She’s on CPAP now. She laughs more. Walks farther. Remembers names.
It’s not glamorous. But it’s life-changing.
If you’re reading this and you’re tired all the time? Please. Get tested.
Love you.
❤️
Emmanuel Peter
Let’s be real-this is just another way for the medical-industrial complex to sell you a $2,000 machine you don’t need. Most people who snore are fine. You’re just scared of the word ‘apnea.’
Have you considered that maybe you’re just a bad sleeper? Or stressed? Or drinking too much?
CPAP is a band-aid. Sleep hygiene is the cure.
Also, your ‘heart attack risk’ stats are cherry-picked. I’ve seen the studies. They’re correlational, not causal.
Stop fearmongering.
Ashley Elliott
…I just realized I’ve been ignoring my own snoring for 8 years.
My partner left me a sticky note last week: ‘You sound like a foghorn with a headache.’
And I laughed.
Now I’m scared.
I’ll make the appointment tomorrow.
Thanks for this post.
Really.
Thank you.