Brand vs Generic Medications: What Really Matters for Safety and Cost
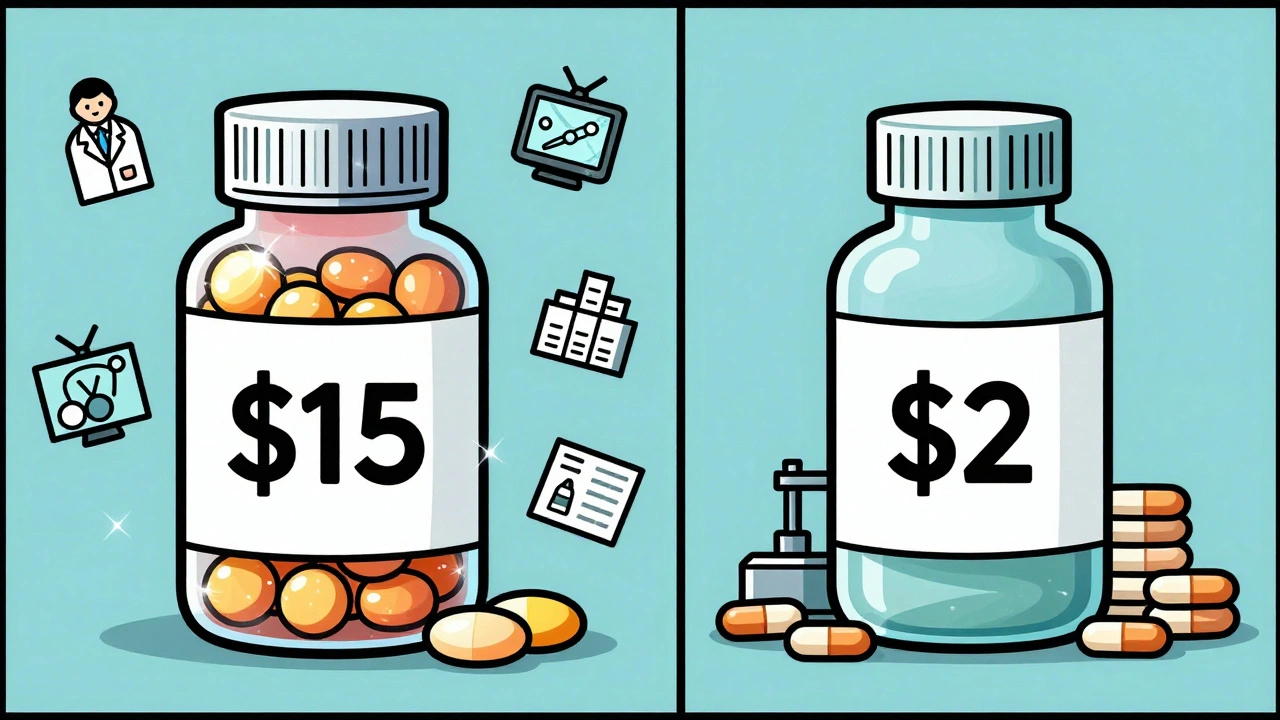
When you pick up a prescription, you might see two options: the brand name drug, a medication developed and marketed by the original pharmaceutical company under a patent. Also known as originator drug, it often costs more because the company recouped research and development expenses. Or you’ll see the generic drug, a version that contains the same active ingredient, dose, and route of administration as the brand, approved by the FDA after the patent expires. Also known as nonproprietary drug, it’s usually cheaper because manufacturers don’t repeat costly clinical trials. But here’s the thing: not all generics are created equal. For most people, they work just fine. For others—especially kids, seniors, or those on high-risk meds—the difference can be life-changing.
The FDA says generics must be bioequivalent to the brand—meaning they deliver the same amount of active ingredient into your bloodstream at the same rate. That’s true for simple pills like metformin or lisinopril. But for complex generic drugs, products like inhalers, injectables, or topical creams where delivery matters as much as dosage, that’s harder to prove. Take liposomal doxorubicin or inhaled corticosteroids: tiny changes in particle size or formulation can mean less medicine reaches your lungs or bloodstream. That’s why some patients report different side effects or reduced effectiveness after switching. The same goes for narrow therapeutic index drugs, medications where the difference between a helpful dose and a toxic one is very small. Lithium, warfarin, phenytoin, and levothyroxine fall here. Even a 10% variation in absorption can trigger toxicity or make the drug useless. That’s why doctors often recommend sticking with one version—brand or generic—and not switching back and forth.
And it’s not just about chemistry. For children with asthma or epilepsy, a switch to generic can mean more hospital visits. Parents might not notice subtle changes in behavior, seizure frequency, or breathing—until something goes wrong. In older adults, mixing generics from different suppliers can lead to confusion, missed doses, or dangerous interactions with other meds. The cost savings look great on paper, but if you end up in the ER because your seizure control slipped, the real cost skyrockets.
So what should you do? Don’t assume all generics are risky. For most common conditions, they’re safe, effective, and smart. But if you’re on a drug with a narrow therapeutic index, if you’re treating a child with a chronic illness, or if you notice a change in how you feel after switching—talk to your doctor. Ask if your med is complex. Ask if your pharmacy switches suppliers. Ask if staying on the brand is worth the extra cost. Your health isn’t a commodity. It’s personal. And when it comes to your meds, small differences matter more than you think.
Below, you’ll find real stories and science-backed insights on when brand and generic truly differ—and when they don’t. From pediatric dosing errors to FDA approval hurdles, these posts give you the facts you need to make smarter choices.