Emergency Room Medication Safety: What You Need to Know Before It’s Too Late
When someone ends up in the emergency room medication safety, the system designed to prevent deadly mistakes when drugs are given under stress. Also known as acute care drug safety, it’s not just about giving the right pill—it’s about knowing what’s already in the body, what’s being added, and how they might react together. Every year, tens of thousands of people are rushed to the ER because a medication they were taking quietly turned dangerous. It’s not always the dose—it’s the mix.
Drug interactions, when two or more medications create an unexpected and harmful effect are one of the biggest hidden risks. Take lithium, used for bipolar disorder, and a simple ibuprofen for a headache. Together, they can crash kidney function and send lithium levels soaring into toxic range. Or consider diphenhydramine—the active ingredient in Benadryl. People think it’s harmless, but taking too much can cause seizures, heart rhythm problems, or even coma. These aren’t rare cases. They show up in ERs regularly, often because the patient didn’t tell the doctor they were taking it, or the doctor didn’t ask.
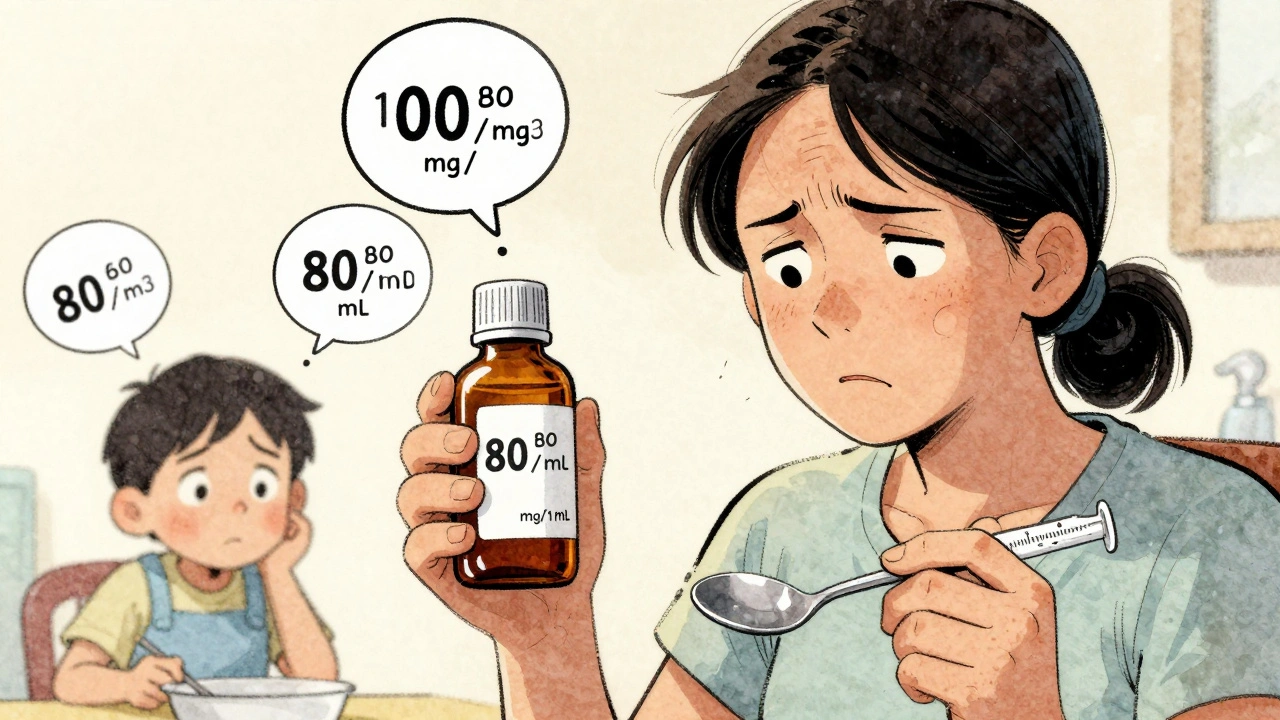
Medication overdose, when the body can’t process or handle the amount of a drug taken doesn’t always mean someone took pills on purpose. It can happen when someone doubles up because they forgot they already took one, or when a new prescription is added without checking what’s already in the system. Sedatives and sleep aids are especially risky—slow breathing, confusion, and unresponsiveness are signs you can’t ignore. And for older adults, even small doses of sedating drugs can lead to falls, fractures, and hospital stays. Aging changes how the body handles medicine, and what was safe at 50 might be dangerous at 70.
What you can do right now
Don’t wait for an emergency. Keep a written list of every pill, patch, cream, or supplement you take—including over-the-counter stuff and herbal remedies. Bring it to every doctor visit. Ask: "Could this interact with anything else I’m taking?" If you’re on lithium, blood thinners, or antidepressants, even a single dose of an NSAID like Advil can be risky. If you’re over 65, ask your doctor to review your meds for fall risks. And if you ever feel dizzy, confused, or your breathing feels slow after taking something new—go to the ER. It’s better to be safe than sorry.
What follows is a collection of real, practical stories and science-backed facts about how medications behave under pressure—how they cause nosebleeds, trigger anxiety, wreck kidneys, or hide in plain sight as "harmless" sleep aids. These aren’t theoretical warnings. These are the cases that end up in emergency rooms. And the good news? Most of them are preventable.