Every year, thousands of children end up in emergency rooms because of a simple mistake: the wrong dose of medicine. Not because parents are careless, but because the system is stacked against them. In pediatric emergencies, medication errors happen more than twice as often as in adults. One in three kids gets hit with a dosing error. And half of those errors could have been stopped before they hurt the child.
Why Pediatric Medication Errors Are So Common
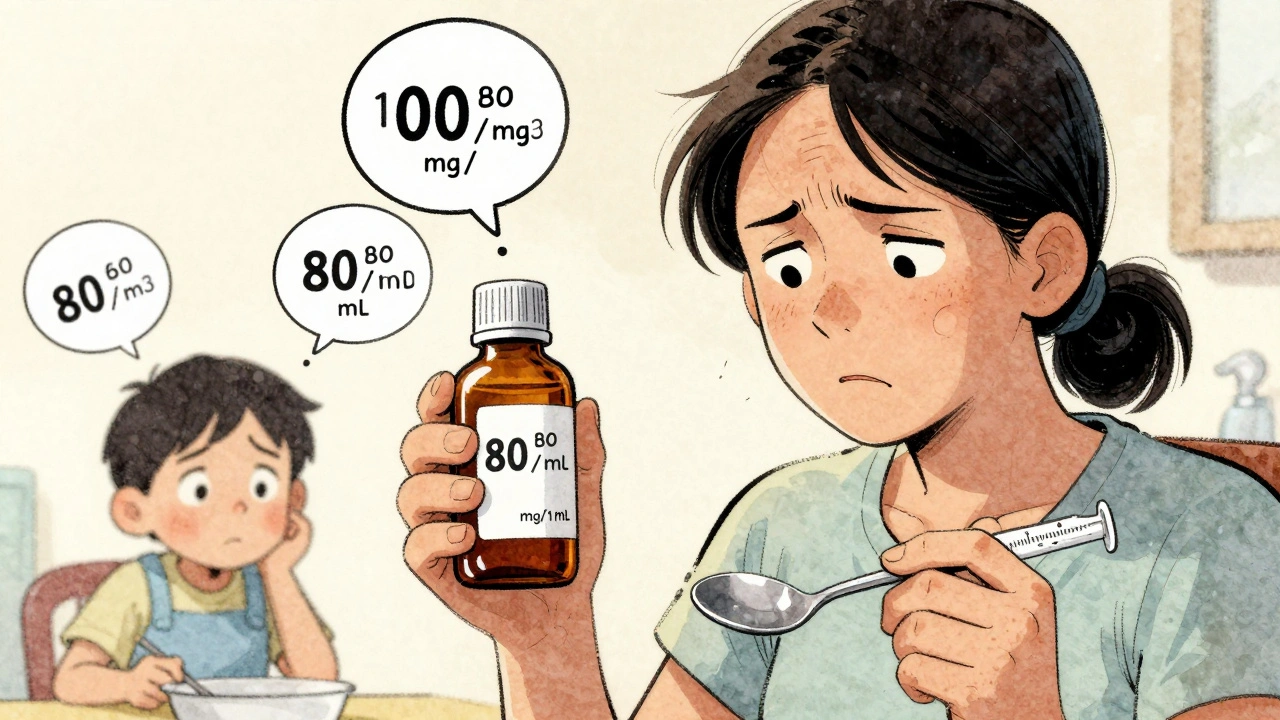
Pediatric dosing isn’t like adult dosing. Adults often get a fixed pill - 500 mg of acetaminophen, 10 mg of ibuprofen. Kids? Their dose depends on weight. Every single time. A 5-kilogram infant needs a completely different amount than a 25-kilogram toddler. That means calculations. And calculations under pressure? That’s where things go wrong. In the chaos of an emergency room, a nurse might grab the wrong syringe. A doctor might misread a weight entered in pounds instead of kilograms. A parent, stressed and exhausted, might mix up milligrams (mg) with milliliters (mL). And it’s not just hospitals. At home, 60 to 80% of dosing errors happen with liquid medicines. Why? Because parents use kitchen spoons, eyeball the dose, or don’t realize that children’s Tylenol and infant Tylenol have different concentrations. One real case: a mother gave her 10-kilogram child 5 mL of liquid acetaminophen, thinking it was the right dose. But the label said 5 mg/kg. That’s 50 mg total. She gave 250 mg - five times too much. The child ended up in the ER with liver damage. This isn’t rare. It’s routine.The Most Dangerous Mistakes
Not all errors are the same. Some are minor. Others are life-threatening. According to safety data from children’s hospitals, the top errors are:- Wrong dose - 13% of all pediatric medication errors
- Wrong medication - 4%
- Wrong rate or time - 3%
- Wrong route - 1%
Who’s at Highest Risk?
It’s not just about the hospital. The biggest risk factor? The family. Parents with low health literacy are 2.3 times more likely to make a dosing mistake. Non-English speakers? Their error rate jumps to 45%, compared to 28% for English-speaking families. Medicaid-enrolled children have 27% more errors than kids with private insurance. Why? Language barriers. Confusing labels. Lack of follow-up. No one sat down with them after discharge to make sure they understood. One parent on Reddit shared: “I gave my 2-year-old 5 mL of children’s Tylenol instead of infant concentrate. I didn’t know they were different. My pediatrician called me back three hours later. I nearly killed my kid.” And it’s not just parents. Nurses in busy ERs juggle 10 kids at once. Doctors rely on verbal orders. Pharmacists are stretched thin. Everyone’s rushing. And in that rush, the simplest things get missed - like checking the concentration on a liquid medicine bottle.
What’s Being Done to Fix It
Some hospitals are turning things around. Nationwide Children’s Hospital in Ohio slashed harmful medication errors by 85% in five years. How? They didn’t just train staff. They changed the system.- Every pediatric dose is now double-checked by two staff members before it’s given.
- EMRs now have built-in pediatric calculators that auto-calculate doses based on weight.
- High-alert medications like epinephrine come pre-mixed in pediatric-specific concentrations - no more manual dilution.
- Pharmacists review every single order in real time.
What Parents Can Do Right Now
You don’t need a PhD to keep your child safe. But you do need to ask questions.- Always ask for the dose in mg/kg. If the nurse says “5 mL,” ask, “How much is that in milligrams per kilogram?”
- Use the tool that came with the medicine. Never use a kitchen spoon. Use the syringe, dropper, or cup that came with the bottle. Those are measured correctly.
- Check the concentration. Infant Tylenol is 160 mg/5 mL. Children’s Tylenol is 160 mg/5 mL too - wait, no. Some brands changed it. Always read the label. If it says “80 mg/1 mL,” that’s a different bottle. Don’t assume.
- Ask for a teach-back. Say: “Can you show me how you want me to give this?” Then do it back to them. If they nod and say yes, you got it right.
- Keep a list. Write down every medication your child takes - name, dose, time, reason. Bring it to every ER visit. Even if you think it’s not important.

The Bigger Picture
This isn’t just about one kid getting too much Tylenol. It’s about a system that assumes parents are experts. But most aren’t. Most are tired, scared, and overwhelmed. And the system doesn’t meet them where they are. The real fix? Standardization. Clear labels. Better training. Technology that doesn’t rely on human memory. And above all - time. Time for nurses to sit down. Time for doctors to explain. Time for pharmacists to double-check. Time for parents to ask questions without feeling stupid. Right now, 63,000 children in the U.S. alone end up in ERs each year because of home medication errors. That costs $28 million. But the real cost? The fear. The guilt. The trauma. The child who almost died because no one made sure the dose was right. We can fix this. But it won’t happen by blaming parents. It’ll happen when hospitals stop treating pediatric dosing like a math test and start treating it like a safety system.What’s the most common pediatric medication error in emergency rooms?
The most common error is giving the wrong dose - often because of miscalculating weight-based amounts. For example, a child weighing 10 kg needs 10 mg/kg of a drug, so 100 mg total. If the dose is written as 10 mL and the concentration is 10 mg/mL, that’s correct. But if the parent thinks it’s 10 mg total and gives 10 mL of a 100 mg/mL solution, that’s a 10-fold overdose. Liquid medications account for 60-80% of these errors.
Why are liquid medications so risky for kids?
Liquid medicines come in different concentrations - like 160 mg/5 mL or 80 mg/1 mL - and many parents don’t realize the difference. Using a kitchen spoon instead of the calibrated syringe that comes with the bottle adds another layer of risk. Studies show 60-80% of home dosing errors involve liquid meds. Even small measurement mistakes can lead to dangerous overdoses in small children.
Can electronic medical records help prevent these errors?
Yes - but only if they’re built for kids. Hospitals with pediatric-specific EMRs now auto-calculate doses based on weight, flag dangerous ranges, and prevent incompatible drug combinations. By 2023, 68% of children’s hospitals had these systems. But most general ERs still use adult-focused software, which doesn’t flag pediatric risks. That creates a safety gap for kids treated outside specialized centers.
How can parents reduce the chance of a dosing mistake at home?
Use only the measuring tool that comes with the medicine. Never use spoons. Write down every medication, dose, and time. Ask the provider to show you how to give it - then do it back to them. Check the concentration on the bottle every time. If it says “80 mg/1 mL” and you’re used to “160 mg/5 mL,” don’t assume they’re the same. Ask. And if you’re unsure, call the pharmacy or your pediatrician before giving it.
Are medication errors more common in certain families?
Yes. Families with limited English proficiency have 45% dosing error rates, compared to 28% for English speakers. Parents with low health literacy are 2.3 times more likely to make mistakes. Children on Medicaid have 27% higher error rates than those with private insurance. These aren’t about negligence - they’re about access, communication, and support. The system needs to adapt to them, not the other way around.
What should I do if I think I gave my child the wrong dose?
Don’t wait. Call your pediatrician or poison control immediately. In Australia, call 13 11 26. In the U.S., call 1-800-222-1222. Have the medicine bottle with you. Tell them the child’s weight, the medicine name, the dose you gave, and the time. Even if your child seems fine, some overdoses take hours to show symptoms. Better safe than sorry.



Anna Roh
Why do hospitals still use paper charts in 2024? I get it, budgets, but kids are dying because someone can’t read handwriting. Fix the system, not the parents.
Katherine Chan
This is so real I cried reading it. My niece got the wrong dose last year because the label was blurry and the nurse was rushing. We got lucky. But so many don’t. Please push for standardized labels everywhere. Not just fancy hospitals. Every ER. Every pharmacy. Every corner store that sells kids’ Tylenol. We can do better.
Simran Chettiar
It is not merely a matter of dosage calculation it is a profound epistemological failure of modern medicine to outsource critical cognitive labor to the exhausted and the linguistically marginalized. The very architecture of care assumes a level of medical literacy that is, statistically, nonexistent among the majority of caregivers. We are not dealing with negligence but with systemic alienation. The parent who uses a kitchen spoon is not stupid - they are abandoned by a system that refuses to meet them in their reality. The real tragedy is not the error - it is the silence that follows it.
Olivia Portier
My cousin is a nurse in a rural ER and she told me they still use handwritten orders and no one double checks meds because they’re understaffed. It’s not that they don’t care - they’re drowning. We need to fund hospitals like we fund military bases. Kids’ lives aren’t a budget line item. Also - use the syringe. I used a teaspoon once. I felt like a monster for weeks. Don’t be like me.
Lauren Dare
Oh wow. So now it’s the hospital’s fault parents don’t know how to read a label? Let me guess - next we’ll be blaming the opioid crisis on people who didn’t read the pamphlet. I mean, I get it. But if you can’t follow basic instructions, maybe don’t be the one administering medicine to a child. Or maybe, just maybe, we need to stop pretending every parent is a nurse.
Taya Rtichsheva
so i gave my kid 10ml of infant tylenol instead of 5ml once bc i was tired and the bottle looked like it had a cap on it but it was just the dropper thing and then i panicked and called poison control and they were chill and said we’re good but still. why is this so hard. why does everything have to be a puzzle.
Darcie Streeter-Oxland
It is incontrovertible that the prevalence of medication error in pediatric emergency settings is directly correlated with the absence of standardized, mandatory, and universally enforced protocols across all healthcare institutions. The notion that parental education alone can mitigate systemic failure is not merely optimistic - it is statistically indefensible. The data is unequivocal: institutional reform, not individual vigilance, is the only empirically validated solution. One must question the moral authority of a system that places the burden of its own incompetence upon the vulnerable.
Tiffany Sowby
It’s not my fault my kid got sick. I didn’t even know there were two kinds of Tylenol. Everyone else in America seems to know this. Why am I the only one who didn’t? Maybe I should’ve Googled it. But I didn’t have time. I was working two jobs. And now I’m the bad parent? No. The system failed me. And you know what? I’m not sorry.