Meningitis isn’t just a headache with a fever. It’s an inflammation of the membranes around your brain and spinal cord-and it can turn deadly in hours. Many people mistake it for the flu, but the difference isn’t just severity-it’s speed. While viral meningitis often clears on its own, bacterial meningitis can kill within 24 hours if untreated. The good news? Most cases are preventable. Vaccines have cut bacterial meningitis rates by up to 99% in countries with strong immunization programs. Understanding the types, recognizing early signs, and knowing when to act can save lives.
What Are the Different Types of Meningitis?
There are five main types of meningitis, each with different causes, risks, and treatments. The most common and least dangerous is viral meningitis, which makes up about 85% of all cases. It’s usually caused by enteroviruses-the same viruses that give you stomach bugs. Most people recover fully in 7 to 10 days without special treatment. Bacterial meningitis is the most dangerous. It’s caused by a few key bacteria: Neisseria meningitidis (meningococcus), Streptococcus pneumoniae (pneumococcus), and Haemophilus influenzae type b (Hib). These bacteria spread through close contact-coughing, kissing, sharing drinks or toothbrushes. Without antibiotics, bacterial meningitis kills 5 to 30% of those infected. Even with treatment, 10 to 20% of survivors face long-term problems like hearing loss, seizures, or brain damage. Fungal meningitis is rare and mostly affects people with weakened immune systems, like those with HIV or on chemotherapy. It’s often caused by Cryptococcus neoformans, a fungus found in soil and bird droppings. It grows slowly but is deadly if not treated with antifungal drugs. Parasitic meningitis is even rarer. It’s most often linked to Angiostrongylus cantonensis, a parasite carried by snails and slugs. People get it from eating raw or undercooked produce in Southeast Asia or the Pacific Islands. It’s not contagious between people. Non-infectious meningitis isn’t caused by germs at all. It can be triggered by autoimmune diseases, certain cancer treatments, or reactions to medications like ibuprofen or antibiotics. It’s harder to diagnose because it doesn’t respond to antibiotics or antivirals.What Are the Real Symptoms of Meningitis?
The classic trio-fever, stiff neck, and confusion-is often shown in movies. But in real life, only about 41% of people with bacterial meningitis have all three. That’s why so many cases are missed at first. More common signs include:- High fever (over 101.3°F or 38.5°C)
- Severe headache that doesn’t go away with painkillers
- Stiff neck-you can’t touch your chin to your chest
- Sensitivity to light (photophobia)
- Nausea or vomiting
- Confusion, trouble concentrating, or drowsiness
How Is Meningitis Diagnosed?
You can’t diagnose meningitis just by symptoms. A spinal tap (lumbar puncture) is the gold standard. A needle is inserted into the lower back to collect cerebrospinal fluid (CSF). In bacterial meningitis, the CSF shows:- White blood cell count over 1,000 per microliter
- Low glucose (under 45 mg/dL)
- High protein (over 100 mg/dL)

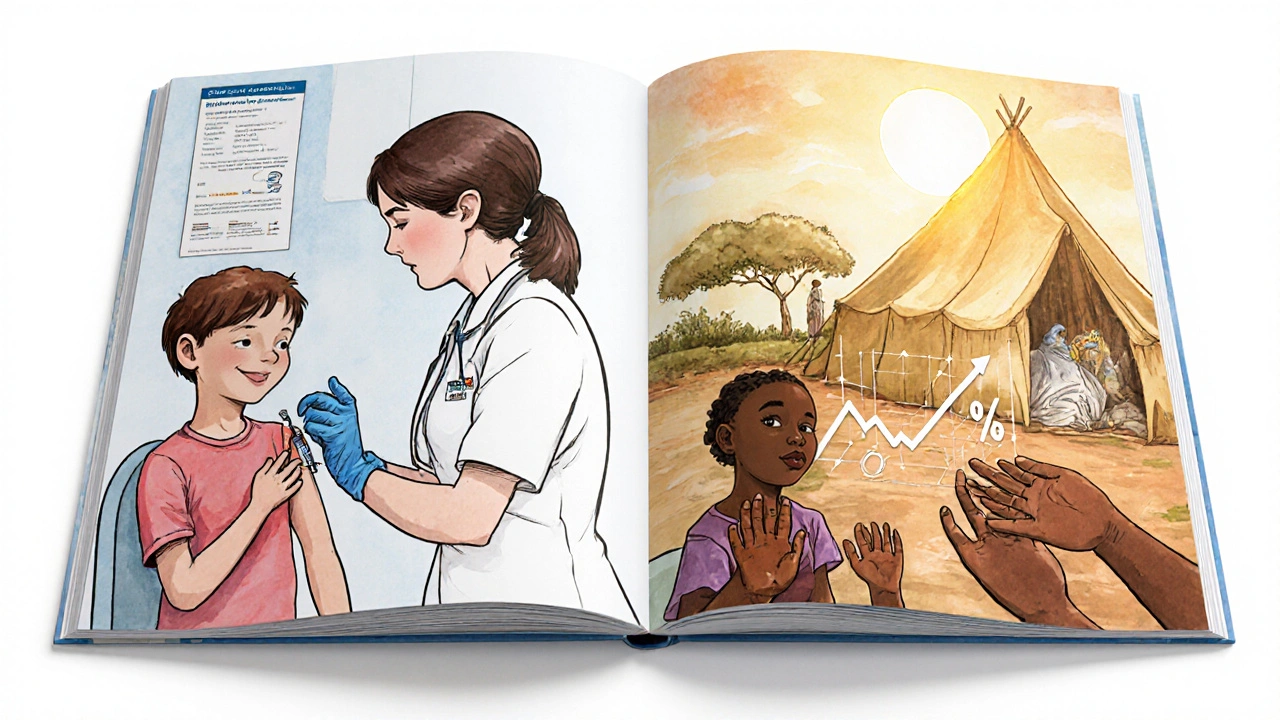
Vaccines: The Most Effective Way to Prevent Meningitis
Vaccines are the single biggest reason meningitis deaths have dropped so sharply. Here’s what’s available and who needs it:- MenACWY (Menveo, MenQuadfi): Protects against four deadly strains (A, C, W, Y). Recommended for all kids at age 11-12, with a booster at 16. It’s 80-85% effective.
- MenB (Bexsero, Trumenba): Targets serogroup B, which causes about 30% of cases in teens and young adults. The CDC now recommends it for all adolescents, not just high-risk groups. It’s 60-70% effective.
- PCV13 (Prevnar 13): Protects against pneumococcal meningitis. Given to babies at 2, 4, 6, and 12-15 months. It cuts disease in young children by 80%.
- Hib: Almost eliminated Hib meningitis in countries with routine shots. Before the vaccine, it was the leading cause of bacterial meningitis in kids under 5.
What Else Can You Do to Prevent Meningitis?
Vaccines are the best tool, but hygiene helps too:- Wash your hands often-especially before eating and after coughing or sneezing. Handwashing cuts transmission risk by 30-50%.
- Don’t share drinks, utensils, toothbrushes, or lip balm. These are common ways bacteria spread.
- If you’re pregnant, avoid unpasteurized dairy and undercooked meats. Listeria can cause meningitis in newborns.
- If someone close to you gets bacterial meningitis, you may need antibiotics to prevent infection. Ciprofloxacin or rifampin can reduce the chance of you getting it from less than 5% to under 0.1%.
Why Do So Many People Miss the Signs?
A 2023 survey of 1,200 meningitis survivors found that 68% waited over 38 hours before seeking help. Many thought it was just the flu. Nearly half were initially told they had migraines or a viral infection. On online forums, a common mistake is waiting for the rash. But as we’ve seen, it doesn’t always appear. One Reddit thread with 287 healthcare workers showed that 73% had treated patients who delayed care because they didn’t have a rash. Parents often feel dismissed by doctors. The Meningitis Research Foundation found that 63% of caregivers said medical staff initially ignored their concerns. That’s why it’s critical to trust your gut. If your child or loved one has a fever, headache, and seems unusually sleepy or confused-get them to a hospital. Don’t wait for the rash. Don’t wait for the stiff neck. Time is everything.What’s Next in Meningitis Prevention?
The future looks promising. In 2024, the FDA approved Trumenba for use in kids as young as 10. The WHO prequalified a new low-cost MenACWY vaccine for African use. And researchers are testing a universal meningococcal vaccine that targets proteins common to all strains. Early trials showed 92% effectiveness. But challenges remain. Antibiotic resistance in pneumococcus is rising-now over 30% of strains in the U.S. don’t respond to penicillin. That means doctors must use stronger drugs right away, even before test results come back. The WHO’s goal is to cut meningitis cases by 50% and deaths by 70% by 2030. That’s possible-but only if vaccines reach everyone, not just the wealthy. Global access, better surveillance, and public awareness are the next frontiers.What Should You Do Now?
If you’re a parent: Make sure your child has had all their meningitis shots. Check their immunization record. If they’re 16 and never got the MenB shot, talk to your doctor. If you’re a college student: Many schools require MenACWY. Ask if MenB is recommended or required. If you live in a dorm, you’re at higher risk. If you’re traveling: Check if meningitis vaccines are recommended for your destination. Some countries, like Saudi Arabia, require proof of vaccination for pilgrims. If you’re unsure: Call your doctor. Don’t wait for symptoms. Prevention is simple. Treatment is not.Every year, thousands of people survive meningitis with permanent damage. But almost all of those cases could have been prevented. Vaccines work. Early action saves lives. Know the signs. Get protected.



Victoria Short
My kid got the MenB shot last year and I still don’t know why it cost $150. Like, why does this vaccine feel like a luxury item? We’re not even rich and it felt like we were buying a new phone.
But yeah, at least she’s not getting sick. Just wish it was easier to get.
Eric Gregorich
Let’s be real-this whole meningitis thing is just nature’s way of reminding us how fragile we are. We live in this hyper-connected world where we share drinks, hugs, and Wi-Fi passwords like they’re nothing, and then boom-one sneeze and you’re staring down a bacterial storm that could end your life before you finish your coffee.
And yet we’re still out here debating whether vaccines are ‘natural’ or ‘too corporate.’ Like, the same people who’ll cry about ‘freedom’ will also ignore the fact that their kid’s immune system is basically a solo player in a global game of tag where one wrong move means a lifetime of hearing loss.
It’s not about fear. It’s about humility. We used to bury children for this. Now we have a shot that costs less than a Netflix subscription. The real tragedy isn’t the disease-it’s the arrogance that lets us think we’re somehow above it all. We’re not. We’re just lucky we’ve got science on our side… for now.
Koltin Hammer
Man, I remember when my cousin got meningitis in college back in 2012. She was fine one night, woke up with a headache, and by noon she was in the ICU. No rash. No stiff neck. Just… really weird behavior. Like she couldn’t remember her own name for a minute.
Turns out it was MenB. She survived, but her hearing’s never been the same. And honestly? I didn’t even know MenB was a thing until then.
Now I make sure my nieces and nephews are all up to date. Not because I’m scared-I’m just tired of seeing people get blindsided by something that’s literally preventable. And yeah, the cost sucks, but compared to a lifetime of rehab? That’s not even a calculation.
Also, props to the WHO for pushing those 50-cent vaccines in Africa. That’s the kind of global solidarity we need more of. Not just lip service.
And if you’re reading this and you’re 18 and living in a dorm? Go get the shot. Don’t wait for a meme to tell you it’s important. Your future self will thank you.
Phil Best
Ohhh so now we’re supposed to trust doctors who told my sister it was ‘just a migraine’ for three days before she collapsed? Thanks, but I’ll take my gut over a textbook any day.
And let’s not pretend vaccines are some magical unicorn. They’re not perfect. But neither is waiting for a rash that might never come.
Also, why do we act like meningitis is some rare horror movie? It’s not. It’s a slow-motion car crash that happens every single day-and we’re all just scrolling past it because ‘it won’t happen to me.’
Newsflash: it already did. To someone you know. Maybe even you.
Get the shot. Stop the drama. The world doesn’t need more ‘I told you so’ obituaries.
Parv Trivedi
Thank you for sharing this important information. In my country, many people still believe vaccines cause more harm than good. But after reading this, I understand how much protection they provide. I will share this with my family and friends. Prevention is better than cure, and vaccines are one of the greatest gifts of modern medicine.
Let us all be responsible and protect each other.