Fall Prevention: How to Stay Steady and Avoid Injury as You Age
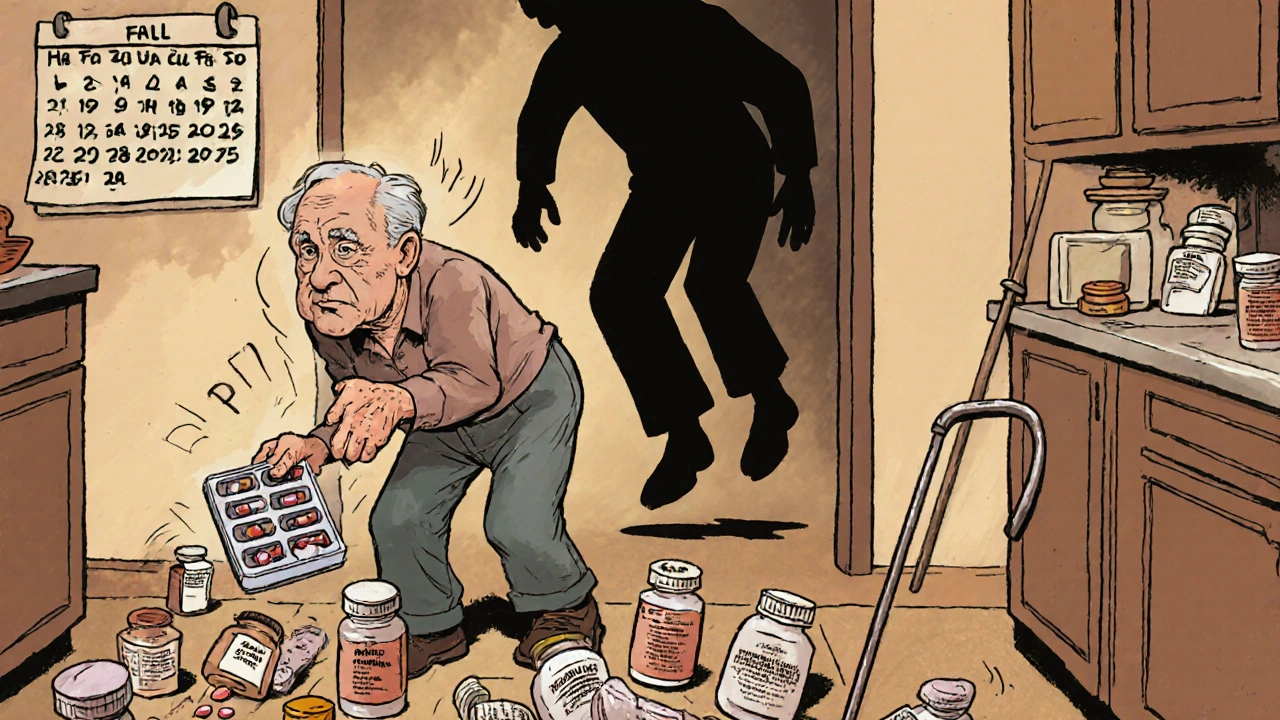
When we talk about fall prevention, the practice of reducing the risk of accidental falls, especially in older adults. Also known as fall risk reduction, it’s not just about installing grab bars—it’s about spotting hidden dangers in your body, your meds, and your home. One in four adults over 65 falls each year, and many of those falls aren’t accidents—they’re side effects of something they’re taking.
Medications like antidepressants, drugs used to treat depression that can cause dizziness and balance issues, sedatives, medications that calm the nervous system and slow reaction time, and even blood pressure pills, drugs that lower hypertension but may cause sudden drops in pressure when standing can make you wobbly. You might not feel dizzy until you stand up—and by then, it’s too late. That’s why a Medicare Annual Medication Review, a yearly check-in with your doctor to review all your prescriptions isn’t just paperwork—it could be the difference between staying on your feet and ending up in the ER.
Your home matters too. Loose rugs, poor lighting, cluttered hallways—these aren’t just annoyances, they’re trip wires. But fixing them isn’t just about buying a non-slip mat. It’s about understanding how your vision, nerve health, and muscle strength are changing. Simple balance exercises, like standing on one foot while brushing your teeth, can rebuild stability over time. And if you’re taking something like statins, which can cause muscle aches, that weakness might be making you more likely to stumble. It’s not just age—it’s the combo of meds, movement, and environment.
What you’ll find below are real stories and science-backed tips from people who’ve been there: how a change in antidepressants stopped daily dizziness, why a simple home audit cut falls in half for one senior, and how a single medication review uncovered three drugs that were working against each other. No fluff. Just what works.