Older Adults and Medication Safety: What You Need to Know
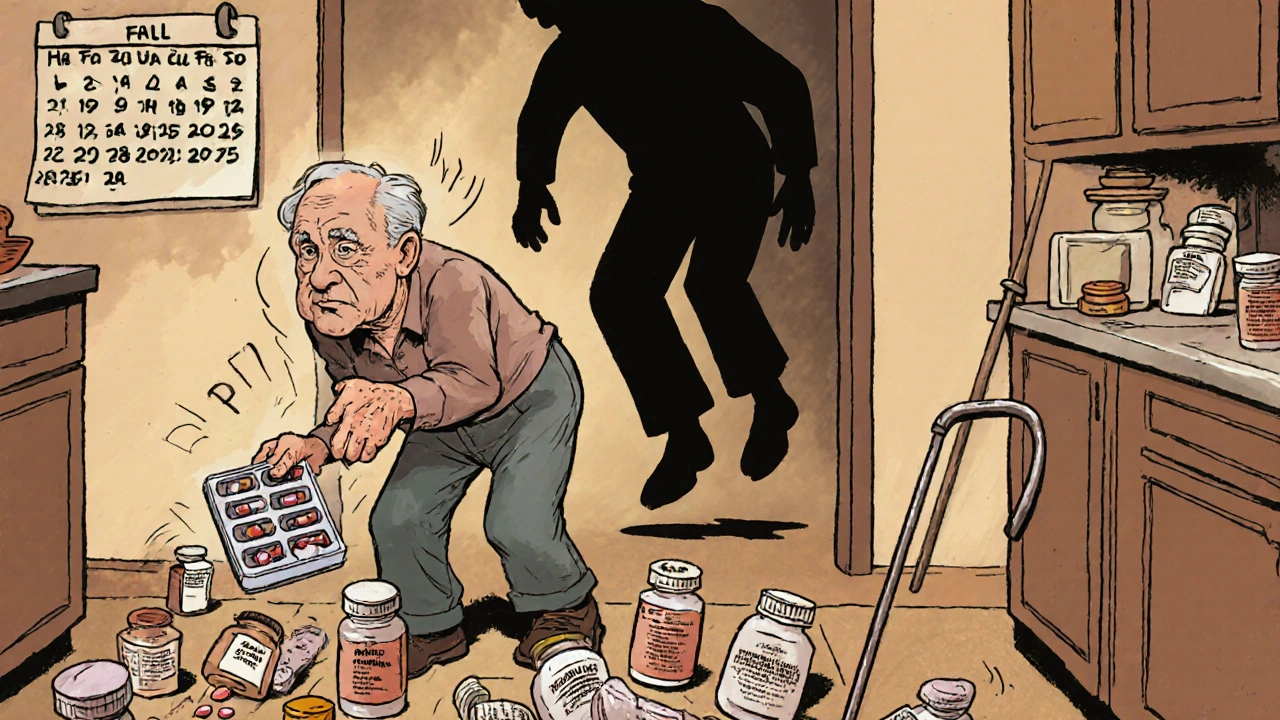
When it comes to older adults, people aged 65 and older who often manage multiple chronic conditions and medications. Also known as seniors, they make up the largest group of prescription drug users in the U.S. Nearly 80% of older adults take at least one prescription drug daily, and over 40% take five or more. That’s not just common—it’s a ticking time bomb for side effects, mix-ups, and dangerous interactions.
Why does this happen? As people age, their bodies change. Liver and kidney function slow down, meaning drugs stick around longer. Muscle mass drops, fat increases, and stomach acid levels shift—all of which change how medications are absorbed and broken down. Add to that the fact that many older adults see multiple doctors, fill prescriptions at different pharmacies, and forget what they’re taking, and you’ve got a recipe for trouble. A simple mix of a blood thinner and an anti-inflammatory can lead to internal bleeding. A common decongestant like pseudoephedrine can spike blood pressure in someone already on heart meds. These aren’t rare mistakes—they’re everyday risks.
It’s not just about the drugs themselves—it’s about how they interact with your body and other pills. pharmacogenomics, the study of how your genes affect your response to medications. Also known as personalized medicine, it’s already helping doctors pick the right antidepressant or cholesterol drug based on your DNA. But most seniors haven’t been tested. That means they’re guessing what works, and what doesn’t. Meanwhile, drug interactions, when two or more medications change each other’s effects. Also known as medication conflicts, they’re the leading cause of hospital visits for older adults. And senior prescriptions, the collection of medications regularly taken by older adults, often including blood pressure pills, pain relievers, and mental health drugs. Also known as polypharmacy, this isn’t always necessary—it’s often just the result of routine refills without review.
You don’t need to stop taking your meds. But you do need to ask the right questions. What’s this pill really for? Could it be making my dizziness worse? Is there a cheaper, safer version? Are any of these drugs canceling each other out? The Medicare Annual Medication Review isn’t just a formality—it’s your best chance to catch problems before they become emergencies. And if you’re on statins, anticoagulants, or antidepressants, you’re especially at risk for side effects that get mistaken for aging—like muscle pain, confusion, or fatigue.
What follows is a collection of real, practical guides written for people who manage medications every day. You’ll find clear breakdowns of how common drugs like statins, antihistamines, and antidepressants behave in older bodies. You’ll learn how to spot dangerous interactions before they happen. And you’ll see how newer tools—like genetic testing and medication reviews—are making it safer to take what you need without taking unnecessary risks. This isn’t theory. These are the stories, data, and steps real seniors and their caregivers use to stay healthy, alert, and in control.