Getting the meds you need shouldn’t mean choosing between rent and refills. Millions of Americans - even those with jobs - struggle to afford prescriptions. But there’s a network of community clinics across the country that offer free or low-cost medications to people who can’t pay full price. You don’t need insurance. You don’t need to be homeless. You just need to be struggling to pay.
What Kind of Clinics Give Out Free Medications?
There are two main types of clinics that help people get medications without breaking the bank: Federally Qualified Health Centers (FQHCs) and free or charitable clinics. Both serve low-income patients, but they work differently.FQHCs are government-funded clinics that charge based on your income. If you make less than $29,160 a year as a single person (200% of the federal poverty level in 2023), your visit and medications could cost as little as $10-$20. You pay what you can. These clinics often have pharmacies on-site or partnerships with local pharmacies to fill prescriptions at reduced prices. They’re open regular business hours, have more staff, and offer more services - including mental health care and chronic disease management.
Free clinics are usually nonprofit, volunteer-run, and don’t charge anything at all - if you qualify. Most require proof that you have no insurance and earn under 200% of the federal poverty level. They don’t have the same hours or staffing as FQHCs, but they’re often the only option for people who make too much to qualify for Medicaid but too little to afford prescriptions.
Many free clinics focus on chronic conditions like diabetes, high blood pressure, asthma, and depression - the kind of illnesses that need daily meds. The Free Clinic of Powhatan in Virginia, for example, runs an in-house pharmacy that dispenses medications for these exact conditions. Patients don’t get every drug on the market, but they get the ones that keep them alive.
How Do Clinics Get These Medications?
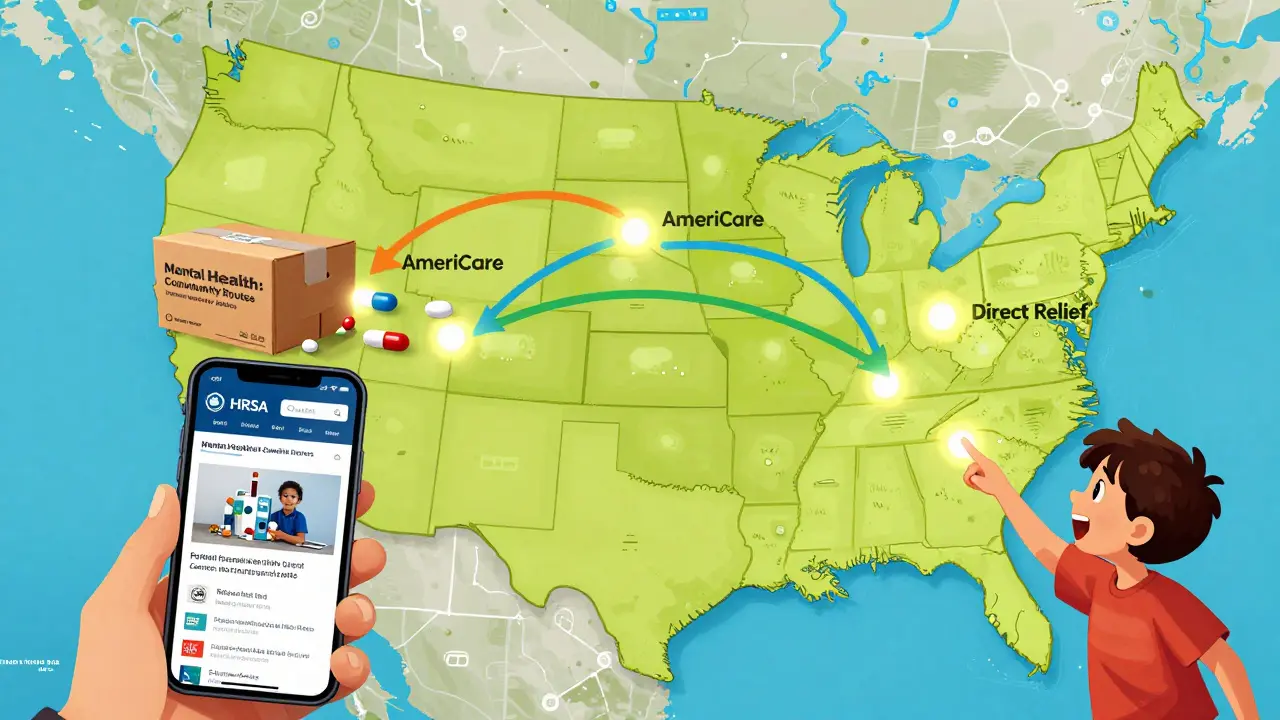
You might wonder: where do all these free drugs come from? The answer is mostly donations.Pharmaceutical companies donate millions of dollars’ worth of unused or excess medications each year. Organizations like Americares and Direct Relief collect these donations, sort them by type and expiration date, and ship them to clinics. Americares alone distributed $190 million in medicines and supplies to nearly 1,000 clinics in 2023, helping over 7 million people.
Some clinics get direct support from drugmakers through Patient Assistance Programs (PAPs). These are programs run by companies like Pfizer, Merck, and Teva that give free or deeply discounted drugs to people who meet income requirements. Clinics help patients apply for these programs - sometimes filling out paperwork, sometimes just giving out the forms.
In 2023, a big push happened in mental health. Teva Pharmaceuticals teamed up with Direct Relief and the National Association of Free & Charitable Clinics to launch Community Routes: Access to Mental Health Care. They gave $75,000 grants to clinics in California, Florida, and New Jersey to expand access to anxiety and depression meds. That program has since expanded to seven more states.
How to Find a Clinic Near You
You can’t just walk into any clinic and get free meds. You need to find one that serves your area and accepts your income level. Here’s how to start:- Go to HRSA’s Find a Health Center tool (findahealthcenter.hrsa.gov). This maps all FQHCs in the U.S. Click on one near you, then call and ask: “Do you offer sliding scale medication costs?”
- Visit the National Association of Free & Charitable Clinics website (nafcclinics.org). They have a searchable directory of free clinics by state. Each listing tells you what services they offer - including whether they have an on-site pharmacy.
- Check your state’s free clinic association. For example, if you’re in Virginia, go to vafreeclinics.org. These state sites often list clinics that don’t appear on the national directory.
- If you’re looking for mental health meds, search for clinics participating in the Community Routes program. Contact NAFC directly to ask which clinics in your state are part of it.
Don’t assume a clinic is too far. Many serve entire counties. If you live in a rural area, your best bet is often the nearest FQHC - they’re more likely to have transportation help or telehealth options.
What You Need to Bring
When you show up, you won’t get meds on the spot. First, you’ll need to prove you qualify. Most clinics ask for:- Proof of income: last 3 pay stubs, tax return, or a letter from your employer
- Proof of residency: utility bill, lease agreement, or state ID
- Proof of no insurance: a written statement that you don’t have coverage, or a denial letter from Medicaid
- Current medication list: bottles or a written list of what you’re taking
- Photo ID
Some clinics require you to fill out a full application form. Others do a quick interview. Either way, they’ll ask about your medical history - especially if you have diabetes, heart disease, or a mental health condition. That’s because they prioritize chronic illness meds.
Be honest. If you’re working two jobs and still can’t afford your insulin, they’ll help. If you’re skipping doses because of cost, they’ve heard it before - and they want to fix it.
What Medications Are Available?
Not every drug is free. Clinics don’t stock brand-new, expensive specialty drugs. But they do carry the essentials:- Metformin for diabetes
- Metoprolol, Lisinopril, Amlodipine for high blood pressure
- Albuterol inhalers for asthma
- Fluoxetine, Sertraline, and other common antidepressants
- Levothyroxine for thyroid issues
- Aspirin and statins for heart health
Many clinics have a formulary - a list of approved meds. If you need something not on the list, they may help you apply for a Patient Assistance Program through the drugmaker. That can take 2-6 weeks, but it’s often successful.
One big limitation: antibiotics and short-term meds (like for infections) are rarely available for free. Clinics focus on long-term, life-sustaining drugs. If you need a quick fix, they’ll refer you to a low-cost urgent care or pharmacy discount program.

What If You’re Turned Away?
Sometimes clinics are full. Waitlists are common. Some free clinics only hold clinics two nights a week. FQHCs may have 4-6 week wait times for new patients.If you’re denied:
- Ask if they can connect you to a pharmacy discount card. Programs like GoodRx, NeedyMeds, or RxAssist can cut your cash price by 80% - even if you have insurance.
- Call 211 - the national helpline. They’ll connect you to local resources, including food banks that sometimes partner with clinics to distribute meds.
- Check if your state has a prescription drug assistance program. Some states, like California and New York, offer state-funded help for low-income residents.
- Visit a pharmacy like Walmart or Kroger. Many sell generic versions of common meds for $4-$10 a month.
And if you’re still stuck? Keep calling. Clinic staff change. New grants come in. A clinic that said “no” last month might have extra insulin next week.
Why This System Exists - And Why It’s Not Enough
This network of clinics exists because the U.S. healthcare system leaves millions behind. Over 30 million Americans are uninsured. Even more are underinsured - meaning they have insurance but can’t afford copays or deductibles.Most patients using these clinics are working. They’re cashiers, warehouse workers, home health aides. They make too much for Medicaid but not enough to afford insulin that costs $300 a vial.
But the system is fragile. Forty-two percent of free clinics reported medication shortages in 2022. Volunteers quit. Donations drop after holidays. Clinics in rural areas close faster than those in cities.
Still, they’re saving lives. A patient in Ohio told a clinic worker: “I haven’t missed a dose of my blood pressure pill in 18 months because of you.” That’s not a statistic. That’s what this is for.
You don’t have to be desperate to ask for help. You just have to need it. And if you do, there’s someone out there who can help - if you know where to look.
Can I get free medications if I have a job?
Yes. Most free clinics serve people who earn under 200% of the federal poverty level - about $29,160 a year for one person. Many working adults fall into this range, especially if they’re hourly workers, part-time employees, or have dependents. You don’t have to be unemployed to qualify.
Do I need to be a U.S. citizen to get free meds?
No. Most clinics serve anyone living in their service area, regardless of immigration status. Proof of residency - like a utility bill or lease - is usually enough. Some clinics may ask for an ID, but they won’t report you to immigration.
Can I get brand-name drugs for free?
Rarely. Clinics mostly stock generic versions, which are just as effective and far cheaper. But if you need a brand-name drug and can’t afford it, the clinic may help you apply for the manufacturer’s Patient Assistance Program. These programs sometimes provide brand-name meds for free to qualifying patients.
How long does it take to get medications after applying?
If the clinic has the medication on-site, you might get it the same day. If they need to order it or apply for a Patient Assistance Program, it can take 2 to 6 weeks. Mental health meds through the Community Routes program often take 3-4 weeks. Ask the clinic for a temporary supply while you wait.
Are there clinics that help with insulin specifically?
Yes. Many clinics prioritize insulin because it’s life-saving. Americares and other donors supply insulin in bulk. Some clinics also partner with insulin manufacturers like Eli Lilly and Novo Nordisk, which offer free insulin programs for uninsured patients. Ask specifically about insulin when you call.
What if I need a medication that’s not on the clinic’s list?
Tell them anyway. Clinics often have connections to pharmaceutical companies or nonprofit programs that can help. They might not have the drug, but they may know how to get it for you through a Patient Assistance Program. Don’t assume it’s impossible - many people get access to rare or expensive meds this way.





anggit marga
This whole system is just a bandaid on a gunshot wound
Why are we celebrating free insulin when the drug companies are still raking in billions
Someone needs to burn down the pharmaceutical boardroom and start over
These clinics are a joke
We need universal healthcare or nothing
Joy Nickles
OMG I JUST FOUND OUT ABOUT THIS!!
I’ve been skipping my blood pressure meds for 3 years because I thought I had no options!!
Just called my local FQHC and they said I qualify!!
They have lisinopril!!
Like… literally right now??
My heart is crying!!
Thank you thank you thank you!!
PS: Do they take debit cards??
PPS: Is the pharmacy open on Sundays??
PPPS: Can I get a sample of the metformin before I commit??
Emma Hooper
Let me tell you about my cousin Brenda-she’s a single mom working two shifts at Target, makes $28k a year, and her insulin used to cost $400 a vial
She found a free clinic in Toledo that gives her metformin, sertraline, and even a free inhaler for her asthma
They don’t ask for a social security number
They don’t care if you’re ‘legal’
They just hand you the pills like you’re family
Brenda’s been stable for 14 months now
She started painting again
She says the sertraline didn’t just fix her mood-it gave her back her soul
And you know what? She volunteers there now
She’s the one who fills out the forms for new patients
She says the hardest part isn’t the paperwork
It’s watching people cry when they realize they don’t have to choose between rent and refills anymore
So yeah
These clinics? They’re not charity
They’re miracles in scrubs
Sara Stinnett
It's fascinating how society has normalized the existence of pharmaceutical apartheid
Where access to life-saving medication is contingent upon income, geography, and bureaucratic whim
The fact that we’ve created a parallel system of charitable medicine to compensate for systemic failure is not a triumph
It is a moral indictment
These clinics are not solutions
They are symptoms
Of a healthcare model that commodifies survival
And yet
We praise the volunteers
We thank the donors
We applaud the nonprofit directors
When we should be marching on Congress
And demanding that insulin be priced at cost
Not at profit
Not at convenience
But at the value of a human life
linda permata sari
I came from Indonesia and I never thought I’d see anything like this in America
In Jakarta, if you can’t pay for meds, you just… don’t get them
People die quietly
Here? People get metformin
Here? People get sertraline
Here? People get to live
I cried when I read this
Not because I needed help
But because I realized-this is what compassion looks like
Not in a temple
Not in a church
But in a tiny clinic with a volunteer pharmacist who remembers your name
Brandon Boyd
THIS IS THE KIND OF STUFF THAT MAKES ME BELIEVE IN PEOPLE AGAIN
Stop scrolling
Stop complaining
Go find a clinic near you
Volunteer
Donate
Or just shut up and be grateful someone’s doing the work
You think your 9-to-5 is hard?
Try being the person who shows up every Tuesday to hand out pills to 80 people who might not see another doctor this year
That’s real work
That’s real courage
That’s real love
Branden Temew
If you think this is a story about healthcare
You’re missing the point
This is a story about the quiet rebellion of kindness
When the system says ‘no’
People say ‘here’
When the government looks away
Volunteers show up with boxes of pills
And you know what?
It’s not enough
But it’s everything
And maybe that’s how revolutions start
Not with marches
But with a pharmacist handing you your insulin and saying ‘Take care of yourself’
Frank SSS
Yeah sure
Free meds
But have you seen the waitlist at the free clinic in my town?
They only open twice a month
And the guy who runs it retired last year
Now it’s run by a 72-year-old nurse who drives 40 miles each way
And the insulin they have? Expired last June
But hey
At least they’re trying
Right?
Paul Huppert
Just called the FQHC in my county
They have metoprolol and fluoxetine
And they’ll help me apply for PAP if I need something else
They don’t ask for ID if I don’t have it
Just need proof I’m making under $30k
It’s not perfect
But it’s real
Thank you for sharing this
Hanna Spittel
THEY’RE LYING ABOUT THE INSULIN!!!
It’s all a government mind-control scheme to make you dependent on clinics so they can track your biometrics!!!
Also I saw a video where someone got a free inhaler and then their phone started glitching
Check the comments on the FDA site
They’re deleting posts about this!!!
🚨
Urvi Patel
How quaint
That in America you need charity to survive
While in Delhi we just pay
Or die
At least there’s clarity
Here you pretend compassion is a solution
When it’s just a distraction
From the real disease
The system
Marilyn Ferrera
Important note: Many free clinics now offer telehealth for med refills
If you’re rural or disabled, call first
Some have mail-order options for chronic meds
Also: Always ask about their formulary before you go
Some have 200+ drugs; others only 30
Don’t waste your trip
Robb Rice
Thank you for this comprehensive and well-researched guide
It’s rare to see such thoughtful documentation of community-based care
I’ve shared it with my local health department
And encouraged them to partner with Americares
Let’s hope this becomes policy, not just prayer
Harriet Hollingsworth
So now we’re rewarding people who can’t afford meds by giving them free ones?
What about personal responsibility?
Why not just get a better job?
My cousin works two jobs and still pays for her meds
She didn’t get handouts
She just worked
Maybe if people stopped expecting free stuff they’d stop being poor