Diphenhydramine Overdose Risk Calculator
Diphenhydramine Dose Calculator
Calculate your risk of diphenhydramine overdose based on your weight and the amount consumed. This tool is for educational purposes only and does not replace medical advice.
Most people think of diphenhydramine as a harmless sleep aid or allergy pill. You grab a Benadryl when you can’t sleep, or when your skin itches after a bug bite. It’s over-the-counter, cheap, and widely available. But when too much gets into the system, it doesn’t just make you sleepy-it can shut down your heart, trigger seizures, or send you into a terrifying hallucinatory state you can’t wake up from. This isn’t rare. In 2022, U.S. poison control centers handled over 12,000 cases of diphenhydramine overdose. Many of them involved teens chasing a high from a pill they thought was safe.
What Happens When You Take Too Much Diphenhydramine?
Diphenhydramine works by blocking histamine, which helps with allergies. But it also blocks another key chemical in your body: acetylcholine. At normal doses (25-50 mg every 4-6 hours), this causes drowsiness. At high doses-anything over 5 mg per kilogram of body weight-that same blocking effect goes into overdrive. That’s when you get the full anticholinergic toxidrome: a cluster of symptoms so distinct, doctors have a mnemonic for it.
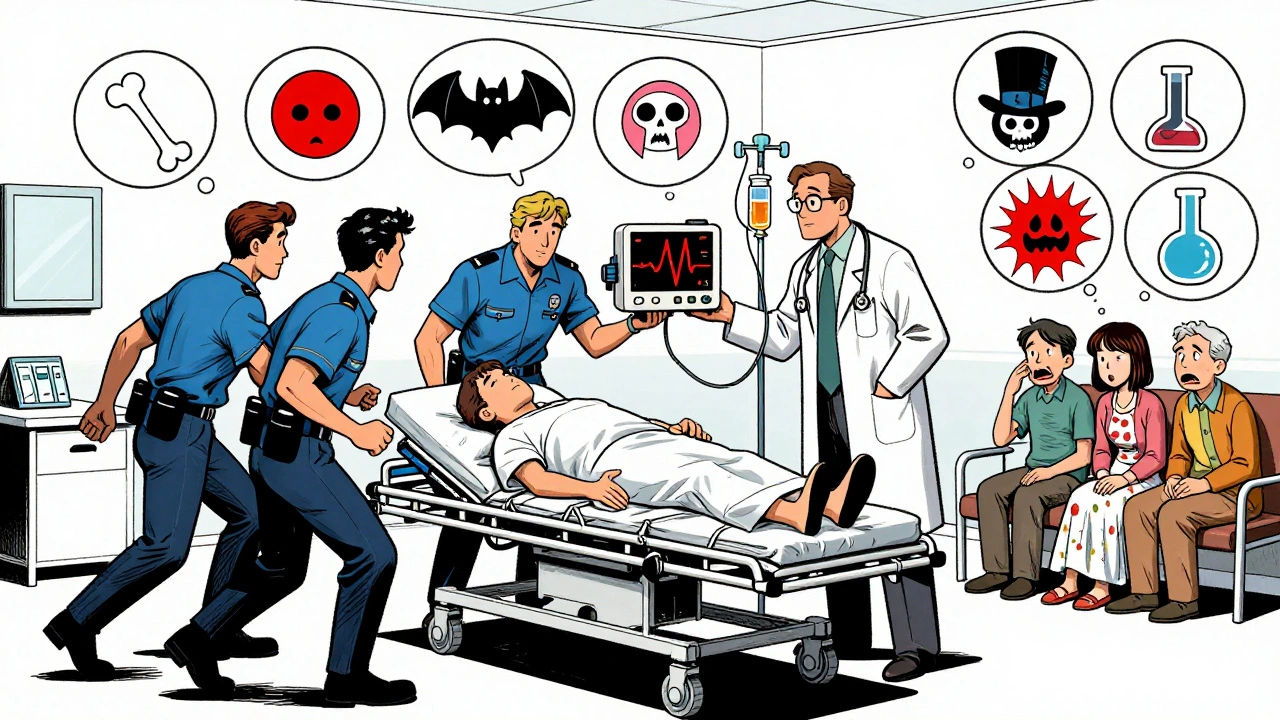
Think: Dry as a bone-your mouth, eyes, and skin feel like parchment. Red as a beet-your face and chest flush bright red. Blind as a bat-your pupils dilate and won’t react to light, making it hard to focus. Mad as a hatter-you’re confused, agitated, or seeing things that aren’t there. Hot as hades-your body temperature spikes past 40°C (104°F). Full as a flask-you can’t pee, even though your bladder is swollen.
These aren’t just uncomfortable-they’re dangerous. At doses above 20 mg/kg, things turn life-threatening. About 1 in 5 people with severe overdoses will have seizures. Your heart rhythm gets messy: the QRS complex on an EKG widens beyond 100 milliseconds, signaling sodium channel blockade. Your QT interval stretches out. You could slip into ventricular tachycardia or even cardiac arrest. Some patients develop rhabdomyolysis, where muscles break down and flood the kidneys with toxic proteins. One case report described a 19-year-old who took 600 mg and woke up in the ER with a catheter, dialysis needed, and no memory of how he got there.
Why Is This So Dangerous? The Hidden Risk
The biggest problem? People don’t realize how easy it is to overdose. A single Benadryl tablet is 25 mg. The lethal threshold for an adult? Around 10-20 tablets. But it’s not just about swallowing pills. Many products combine diphenhydramine with acetaminophen-like Tylenol PM. Someone might take two Tylenol PMs for sleep, then take two more for allergies, not realizing they’ve just doubled their diphenhydramine dose. And because it’s sold in liquid form, too, kids can accidentally drink a whole bottle.
Then there’s the social media angle. Since 2018, there’s been a 300% spike in intentional overdoses among teens aged 13-19. TikTok and Reddit posts promote "Benadryl challenges"-encouraging users to take 10, 20, even 30 pills to hallucinate. One Reddit user wrote: "Took 500 mg thinking I’d trip like LSD. Woke up in the ER with a catheter and IV. I couldn’t move for hours. My brain felt like it was melting." That’s not a party. That’s brain toxicity.
What Should You Do If Someone Overdoses?
If you suspect a diphenhydramine overdose, don’t wait. Call poison control immediately-1-800-222-1222 in the U.S., or your local emergency number. Don’t try to make them vomit. Don’t give them coffee or water to "sober them up." That won’t help and could make things worse.
Emergency teams follow ABCDE: Airway, Breathing, Circulation, Disability, Exposure. They’ll check your vital signs: heart rate (often over 140 bpm), temperature (could be 41°C), blood pressure (might be crashing), and oxygen levels. An EKG is non-negotiable. Even if the person seems calm, cardiac changes can appear 2-4 hours after ingestion.
Here’s what happens next:
- Seizures or severe agitation? Benzodiazepines like lorazepam or diazepam are given IV. They calm the brain without worsening heart issues.
- QRS wider than 100 ms? Sodium bicarbonate is infused. It pushes sodium back into heart cells, fixing the electrical block.
- QTc longer than 500 ms? Magnesium sulfate is given to stabilize the heart rhythm.
- Delirium, hallucinations, confusion? Physostigmine can reverse it. It’s not used lightly-it’s risky if the heart’s already unstable-but in controlled settings, it works better than sedatives. One study showed 87% of patients improved with physostigmine versus just 24% with benzodiazepines alone.
- Can’t pee? A urinary catheter is placed. Bladder distension is common in 35-40% of moderate-to-severe cases.
- Body temperature over 39°C? Cooling blankets, ice packs, fans. Hyperthermia can cause organ failure.
IV fluids are almost always started. If the person’s blood pressure drops, vasopressors may be needed. In the rarest cases-when the heart stops and standard CPR fails-doctors have used ECMO (a machine that takes over heart and lung function) to buy time.
What Happens After the Emergency?
Even if the person survives, recovery isn’t quick. Sixty-five percent of overdose patients report lingering drowsiness for 24-48 hours. Forty percent still feel confused or foggy. Some have memory gaps. One patient described it as "being awake but trapped in a dream I couldn’t control. I didn’t know who I was for three days."
Discharge isn’t automatic. Most patients are observed for at least 6 hours after symptoms stop. If there were cardiac changes, monitoring may extend to 12-24 hours. You can’t just go home after the agitation fades. The heart can still fail hours later.
Why Physostigmine Is a Game-Changer (And Why It’s Still Underused)
For decades, doctors avoided physostigmine because they feared it could trigger seizures or arrhythmias. But recent data (2021-2023) shows that’s outdated. In a review of 1,200 cases, adverse events from physostigmine were under 5%. Only 1% had seizures, and none died from the drug itself. The real danger? Delaying treatment. Benzodiazepines mask symptoms but don’t fix the root problem. Physostigmine restores acetylcholine activity in the brain, clearing the fog fast.
Still, many ERs don’t stock it. Some doctors don’t know how to use it. That’s changing. The American College of Medical Toxicology is updating its guidelines in 2024, pushing for earlier use of physostigmine in severe delirium cases. The message is clear: if the brain is shutting down, don’t just sedate it-wake it up.
How to Prevent This
Parents: Keep all medications locked up. Even if your teen seems responsible, peer pressure and online trends can lead to impulsive decisions. The FDA issued a warning in 2021 about "Benadryl challenges"-and the American Academy of Pediatrics launched a campaign to stop them. But social media moves faster than warnings.
Adults: Don’t mix diphenhydramine with alcohol, other sedatives, or antidepressants. Don’t take more than the label says. If you’re using it for sleep long-term, talk to your doctor. There are safer options.
Everyone: Save the poison control number in your phone. Download the Poison Help app-it’s free, works offline, and connects you to experts in seconds. In Australia, call 13 11 26. In the U.S., dial 1-800-222-1222. Every second counts.
Diphenhydramine isn’t evil. It’s a useful drug when used correctly. But like any tool, it becomes dangerous in the wrong hands-or the wrong dose. What’s sold as a simple sleep aid can become a silent killer. Know the signs. Know what to do. And if you’re ever unsure? Call for help. Don’t wait for the worst to happen.
Can you die from a diphenhydramine overdose?
Yes, but it’s rare. Mortality is around 0.5% in severe cases requiring ICU care. Most deaths happen when cardiac arrest occurs without timely treatment. The risk increases sharply with doses over 20 mg per kilogram of body weight-about 1,400 mg for a 70 kg adult. Many fatalities involve co-ingestion of other drugs or delayed medical care.
How much diphenhydramine is too much?
The maximum single dose for adults is 50 mg. Toxic effects start around 5 mg per kg of body weight-that’s 350 mg for a 70 kg person. Life-threatening toxicity usually occurs above 20 mg/kg (1,400 mg). But some people are more sensitive. Even 200-300 mg can cause severe symptoms in children or those with underlying health conditions.
Does activated charcoal help with diphenhydramine overdose?
It may help if given within 1-2 hours of ingestion, especially in large overdoses. But it’s not always effective because diphenhydramine is rapidly absorbed. In most cases, doctors focus on supportive care and specific antidotes rather than decontamination. Activated charcoal is rarely used alone and only if the patient is alert and able to swallow safely.
Why doesn’t a blood test for diphenhydramine help?
Plasma levels don’t reliably predict how sick someone is. Two people with the same blood level can have very different symptoms. One might be mildly drowsy; another could be seizing. Doctors treat based on clinical signs-not lab numbers. Testing is only useful if you’re trying to confirm ingestion in a legal or forensic setting.
Can you get addicted to diphenhydramine?
Diphenhydramine isn’t addictive in the traditional sense like opioids or alcohol. But some people develop tolerance and use it to get high, leading to repeated overdoses. Psychological dependence can form, especially among teens using it for hallucinogenic effects. Withdrawal isn’t life-threatening, but rebound insomnia and anxiety are common when stopping after long-term use.
What Comes Next?
Looking ahead, emergency departments are moving toward standardized protocols for anticholinergic toxicity. New smartphone apps, public awareness campaigns, and updated medical guidelines are making a difference. But the real change comes from awareness. If you know someone who’s using Benadryl to get high, talk to them. If you’re worried about a loved one’s sleep habits or medication use, don’t ignore it. The line between "safe" and "deadly" is thinner than most people think.





Ignacio Pacheco
So let me get this straight-you’re telling me that the same pill I take to knock out after a long day can literally turn my brain into a glitchy Minecraft server? And people are posting videos of this like it’s a TikTok dance? I’m not even mad, I’m just impressed at how efficiently capitalism turns every safety net into a viral challenge.
Jim Schultz
Let’s be clear: this isn’t just ‘bad judgment’-it’s a systemic failure of public health literacy. The anticholinergic toxidrome is textbook, yet 12,000+ cases in 2022? That’s not ignorance-it’s neglect. The FDA warning? A Band-Aid on a hemorrhage. We need mandatory labeling on OTC packaging: ‘DANGER: CAN INDUCE SEIZURES, CARDIAC ARREST, AND PSYCHOTIC STATES.’ Not ‘for occasional use.’ Not ‘as needed.’ FULL. WARNING. IN. RED.
Kidar Saleh
As someone who’s seen this in a UK A&E ward, let me tell you-it’s not dramatic. It’s devastating. A 16-year-old girl, pupils like saucers, mumbling about ‘the walls singing,’ no urine output for 18 hours. No drugs. No alcohol. Just Benadryl. And the worst part? Her mother said, ‘I didn’t know it could do that.’ We don’t need more research. We need better packaging. Better education. Better shame.
Chloe Madison
If you’re reading this and you’ve ever taken more than 50mg of diphenhydramine for sleep-please, stop. You’re not helping yourself. You’re trading one problem for a hospital stay. There are safer, non-habit-forming options: magnesium, melatonin, cognitive behavioral therapy for insomnia. Your body isn’t broken-it’s just being misinformed. Talk to a doctor. Not Reddit. Not TikTok. A licensed professional. You deserve better than a chemical haze.
Albert Essel
It’s worth noting that physostigmine’s underuse isn’t due to safety concerns-it’s due to institutional inertia. The literature has been clear since 2018: it reverses delirium faster and more effectively than benzodiazepines. Yet many hospitals still stock none. Why? Because protocols are slow to change, and clinicians fear liability. This isn’t a medical issue-it’s a bureaucratic one. We need standardized protocols, not anecdotal heroics.
Charles Moore
I’ve worked in ERs across three continents, and I’ve never seen a drug so widely misunderstood. It’s not just teens-it’s elderly patients mixing it with antidepressants, new parents using it for baby sleep, people with anxiety self-medicating. We treat it like aspirin. But it’s not. It’s a potent neurotoxin wrapped in a blue capsule. We need public health campaigns that don’t sound like government pamphlets. Real stories. Real footage. Real consequences.
Gavin Boyne
Let’s be honest-the ‘Benadryl challenge’ is just the latest in a long line of dumbass internet stunts. Remember the Tide Pod challenge? The cinnamon challenge? People don’t do these because they’re stupid-they do them because they’re bored, lonely, and desperate for a moment of control. The real problem isn’t diphenhydramine. It’s a culture that tells kids their pain doesn’t matter unless it goes viral.
Rashi Taliyan
My cousin took 300mg thinking it would help her anxiety. She ended up in ICU for 72 hours. No one told her that the drowsiness you feel at 25mg is just the warning sign-the real danger is the silence after. No tremors. No vomiting. Just… stillness. Then seizures. Then coma. I’m so angry. Not at her. At the fact that no one warned us. Not the pharmacist. Not the label. Not the internet. Just silence.
Kara Bysterbusch
It’s chilling how easily we normalize the normalization of danger. We call it ‘sleep aid’ like it’s a herbal tea. We package it in child-resistant bottles but don’t include a single line about cardiac risk. We allow it to be sold next to aspirin and cough syrup like it’s interchangeable. This isn’t negligence-it’s commodification. We’ve turned a neurotoxin into a commodity, and we’re shocked when the market crashes? Wake up. The packaging should scream. The warnings should be mandatory. The FDA should have banned this as an OTC sleep aid years ago.
Rashmin Patel
Y’all need to stop treating this like a science lecture and start treating it like a public health emergency. I’m from India, and we have the same problem-people take 10-15 tablets because ‘it’s natural’ or ‘it’s from the pharmacy.’ My aunt took 400mg for insomnia and ended up in a coma for 3 days. Her brain didn’t recover fully. Now she forgets her own name sometimes. Don’t wait for someone you love to become a statistic. Share this. Post it. Tag your friends. Save a life. 💙🩺
sagar bhute
Of course this happens. The system is designed to kill you slowly. Pharma companies know diphenhydramine is cheap and profitable. They don’t care if you die as long as you buy more. The FDA is a puppet. Doctors are overworked. Parents are distracted. Teens are lonely. This isn’t an accident. It’s a feature. Wake up. The poison isn’t in the pill-it’s in the system.
Cindy Lopez
Good article.
Gene Linetsky
Wait-so you’re telling me the government allows this drug to be sold without a warning that it can cause permanent brain damage? And you’re not surprised? I’ve got news for you: this isn’t the first time. Remember thalidomide? Fen-phen? Vioxx? This is the same playbook. They let it fly, wait for bodies to pile up, then quietly pull it back. But not before they’ve made billions. You think this is about safety? It’s about profit. And they’re laughing all the way to the bank.
Vincent Soldja
Physostigmine is underutilized because of outdated guidelines and liability concerns. The evidence supports its use in severe anticholinergic delirium. The risk of adverse events is low when administered correctly. Emergency departments should stock it as standard. Delaying its use increases mortality.