DRESS Syndrome Diagnostic Checker
This tool helps assess the likelihood of DRESS syndrome using the RegiSCAR scoring system. Enter your symptoms and criteria below. A score of 3+ indicates probable DRESS, while 5+ is almost certain.
DRESS Criteria Assessment
Your DRESS Score
What Is DRESS Syndrome?
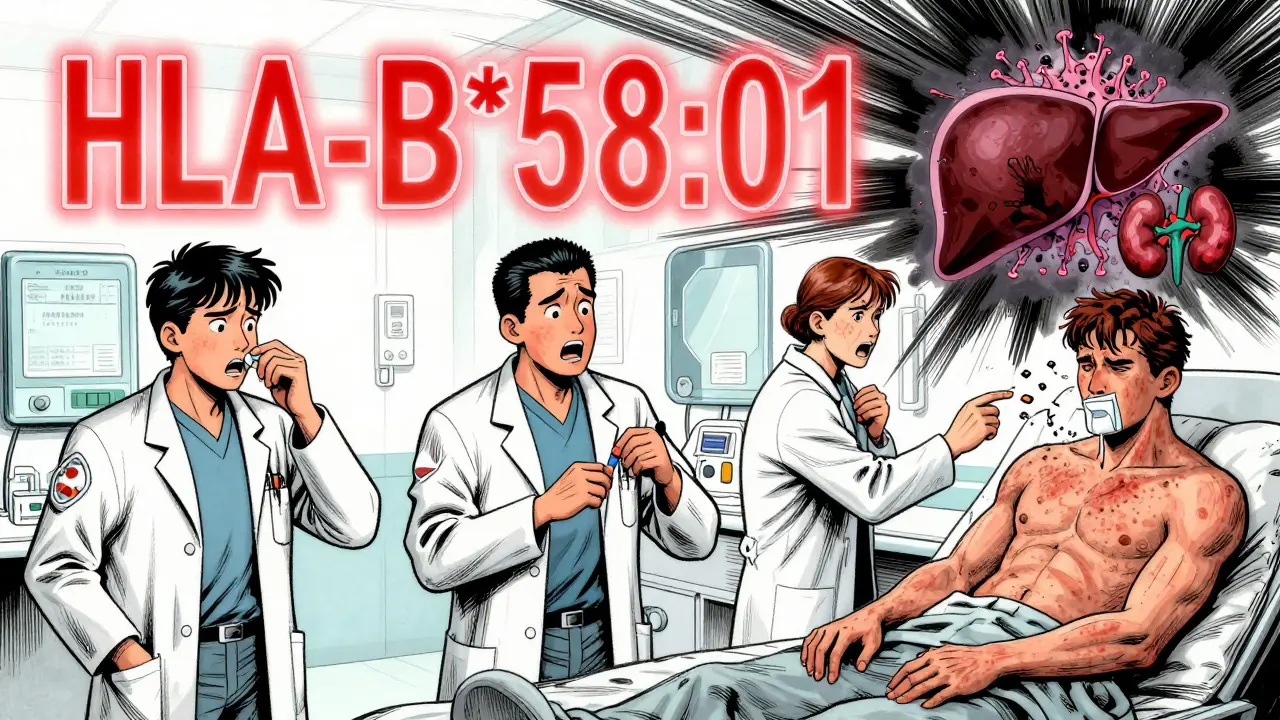
DRESS syndrome is a rare but life-threatening allergic reaction to certain medications that triggers a systemic inflammatory response involving the skin, internal organs, and immune system. It’s not just a rash - it’s a full-body crisis that can shut down your liver, kidneys, or heart if not caught early. First recognized in the 1950s as a reaction to phenytoin, it was formally named DRESS - Drug Reaction with Eosinophilia and Systemic Symptoms - in 1996. Since then, we’ve learned it’s far more dangerous than most doctors realize.
What makes DRESS so tricky is the timing. You don’t react the day after taking the pill. You might take a medication for 3, 4, even 6 weeks before your body flips out. That delay is why so many patients go to the ER three or four times before anyone says, “This isn’t a virus - it’s DRESS.”
How Do You Know It’s DRESS?
There are five key signs that scream DRESS. If you have at least three, you need to be evaluated immediately:
- A widespread, red, flat or slightly raised rash that starts on your face and chest and spreads to cover most of your body
- Fever over 38.5°C (101.3°F) that won’t break
- Swollen lymph nodes in your neck, armpits, or groin
- Eosinophils - a type of white blood cell - above 1,500 per microliter of blood
- One or more internal organs are damaged - most often the liver
More than 95% of patients get the rash. Nearly all have a fever. Liver enzymes like ALT often spike above 300 IU/L - sometimes over 1,000. That’s not just inflammation. That’s liver failure waiting to happen.
Facial swelling and cracked lips show up in over half the cases. But unlike Stevens-Johnson Syndrome, blisters and mouth ulcers are rare. That’s a big clue. If your skin is peeling off in sheets, it’s probably not DRESS. If your liver is failing and your eosinophils are through the roof, it very well could be.
What Medications Cause DRESS?
Not every drug causes DRESS. But some are notorious. The top three culprits:
- Allopurinol - used for gout. Accounts for nearly 3 out of every 10 DRESS cases.
- Anticonvulsants - carbamazepine, phenytoin, lamotrigine. These are the second biggest group.
- Antibiotics - especially sulfonamides and minocycline.
Here’s the scary part: Your risk isn’t random. If you carry the HLA-B*58:01 gene, taking allopurinol can trigger DRESS in up to 1 in 10 people. In Taiwan, they screen everyone before prescribing allopurinol. Since 2012, cases there have dropped by 80%. In the U.S.? No screening. Just guesswork.
Carbamazepine is worse for people with HLA-A*31:01. That’s why the FDA requires warnings on the label - but only for Asian populations. In Australia and Europe, doctors still prescribe it without checking.
Why Is DRESS So Deadly?
One in ten people with DRESS die. That’s a 10% mortality rate - higher than most cases of pneumonia or appendicitis. Why? Because it doesn’t just hurt. It multiplies.
It starts with the skin. Then the liver. Then the kidneys. Then the lungs or heart. And while your organs are failing, your immune system is attacking itself. That’s because of viral reactivation - particularly HHV-6, a herpes virus that lives quietly in your body until your immune system gets confused by the drug. Then it wakes up, and suddenly you’re fighting a virus you didn’t even know you had.
Delayed diagnosis is the biggest killer. The average patient visits the ER 3.5 times before getting the right diagnosis. One Reddit user described going to the ER three times with a rash and fever after taking lamotrigine. Each time, they were sent home with antihistamines. By week seven, their liver enzymes hit 1,200. That’s not a rash. That’s a ticking time bomb.
How Is It Diagnosed?
There’s no single blood test for DRESS. But there is a scoring system - RegiSCAR - that’s been used since 2007 and validated on over 200 patients. It gives you a score based on:
- Timing of reaction (2-8 weeks after starting drug)
- Presence of fever, rash, lymph nodes
- Eosinophil count
- Organ involvement
- Exclusion of other causes
A score of 3 or higher means probable DRESS. A score of 5 or higher? Almost certain. Most hospitals don’t use it. But they should. A 2021 study found only 38% of primary care doctors could correctly identify DRESS criteria. Academic dermatologists? 89% got it right.
Testing should include:
- Complete blood count with differential (to check eosinophils)
- Liver and kidney function tests
- HHV-6, EBV, CMV, and hepatitis viral panels
- HLA typing if high-risk drugs were used
The FDA approved a new point-of-care test for HLA-B*58:01 in March 2023. It gives results in under an hour. That’s a game-changer - if doctors use it.
How Is DRESS Treated?
Step one: Stop the drug. Immediately. No exceptions. If you suspect DRESS, the medication must be discontinued within 24 hours. Waiting even a day increases your risk of organ failure.
Step two: Hospitalize. Most experts agree - if DRESS is suspected, you need to be admitted. Not just any hospital. A place with specialists: dermatologists, infectious disease doctors, and critical care teams. The American Academy of Dermatology recommends ICU-level care if your ALT is over 1,000, your creatinine is above 2.0, or you’re having trouble breathing.
Step three: Steroids. There are no big randomized trials proving they work - but every observational study shows they do. If you start high-dose prednisone within 72 hours of diagnosis, your chance of survival jumps. Most patients need 3 to 6 months of tapering. Quit too fast? The reaction can come back. Too slow? You get diabetes, osteoporosis, or infections.
For the sickest patients, IVIG (intravenous immunoglobulin) or mycophenolate are being tested in clinical trials. Early results are promising. But steroids are still the standard. No one’s found a better option yet.
What Happens After Recovery?
Surviving DRESS doesn’t mean you’re done. About 1 in 3 people develop long-term problems:
- Chronic liver disease
- Autoimmune thyroiditis
- Chronic kidney damage
- Type 1 diabetes
One man in Australia developed permanent kidney failure after 22 days of undiagnosed carbamazepine-induced DRESS. He’s now on dialysis. Another woman recovered from vancomycin-induced DRESS but spent six months tapering off prednisone. She returned to work as a nurse - but she still gets monthly blood tests.
There’s a global registry now - launched in September 2023 - tracking long-term outcomes. Early data shows autoimmune diseases show up years later in people who thought they were “cured.”
Why Isn’t Everyone Getting Screened?
Taiwan screens everyone for HLA-B*58:01 before giving allopurinol. Cost? $15 per test. Savings? Thousands of lives and millions in hospital bills. The U.S. doesn’t do it. Australia doesn’t do it. Most of Europe doesn’t do it.
Why? Because guidelines lag behind science. Because doctors don’t know. Because the system doesn’t reward prevention.
But the numbers don’t lie. DRESS hospitalizations cost $28,500 per case on average in the U.S. in 2022. Screening costs $15. It’s not even a hard choice.
What Should You Do?
If you’re taking allopurinol, carbamazepine, lamotrigine, or sulfonamide antibiotics - and you develop a rash and fever after 2-6 weeks - don’t wait. Go to the ER. Ask: “Could this be DRESS?”
If you’ve had DRESS before - never take that drug again. Ever. And tell every doctor you see. It’s not just a reaction. It’s a life-altering event.
If you’re a clinician - learn the RegiSCAR criteria. Test for HLA-B*58:01 before prescribing allopurinol. Stop guessing. Start screening.
DRESS isn’t rare. It’s underdiagnosed. And every day we wait, someone else gets hurt.
Can DRESS happen with over-the-counter drugs?
Yes. While most cases are linked to prescription drugs like allopurinol or anticonvulsants, there are documented cases tied to NSAIDs like ibuprofen and even herbal supplements. Any medication that affects the immune system can potentially trigger DRESS. Don’t assume OTC means safe.
Is DRESS contagious?
No. DRESS is not contagious. You can’t catch it from someone else. But the viral reactivation involved - like HHV-6 - is common in the population. The problem isn’t the virus. It’s your immune system reacting to a drug and then misfiring against your own tissues.
Can you get DRESS more than once?
Yes. If you’ve had DRESS from one drug, you’re at higher risk of reacting to others - especially those in the same class. For example, if you had DRESS from carbamazepine, you’re likely to react to phenytoin or lamotrigine. Cross-reactivity is common. Always tell your doctor your history.
How long does it take to recover from DRESS?
Recovery takes months. The rash may fade in 2-4 weeks, but organ damage can linger. Liver enzymes often take 3-6 months to normalize. Steroid tapering usually lasts 3-6 months. Full recovery can take up to a year. Some people never fully recover - especially if diagnosis was delayed.
Are there any new treatments on the horizon?
Yes. Clinical trials are testing steroid-sparing drugs like IVIG and mycophenolate. A new NIH-funded project is searching for biomarkers that predict who will develop long-term autoimmune problems after DRESS. By 2027, we may have blood tests that tell you your risk before you even get sick.
Should I get tested for HLA genes if I’m on high-risk meds?
If you’re of Asian descent and prescribed carbamazepine - yes. If you’re prescribed allopurinol and have a family history of gout or kidney stones - absolutely. Even in Australia and the U.S., testing is available. Ask your doctor. It’s a simple blood test that could save your life.



Melissa Cogswell
I’ve seen this play out in the ER three times. One patient was on allopurinol for gout, developed a rash, got sent home with Benadryl twice. By the third visit, her ALT was 1,400. She spent 47 days in the hospital. We didn’t even think of DRESS until her eosinophils hit 2,800. It’s not rare - it’s just ignored. If you’re on any of those meds and get a fever + rash after 3 weeks? Don’t wait. Go now. I wish I’d known this 5 years ago.
Diana Dougan
Wow. Another ‘medical mystery’ that’s been known since the 90s and still no screening? 😂 So the US healthcare system is basically just guessing and hoping people don’t die? I mean, Taiwan screens everyone for $15 and we’re still playing Russian roulette with allopurinol? Someone get me a tissue - I’m crying from laughter.
Bobbi Van Riet
My cousin had DRESS from lamotrigine. She was a nurse, knew something was off, but the docs kept saying ‘allergic reaction’ and gave her steroids for eczema. By the time they admitted her, her kidneys were already failing. She’s fine now, but she has to get bloodwork every 3 months and takes thyroid meds because her immune system went rogue. I’ve told every family member who takes anticonvulsants to get the HLA test. It’s not expensive. It’s not complicated. It’s just common sense. Why are we still not doing this? I just don’t get it.
Holly Robin
THIS IS A BIG PHARMA COVERUP. They don’t want you to know about HLA screening because if you get tested before taking the drug, you won’t need the $28k hospital stay. That’s BILLIONS in lost profits. And don’t get me started on the FDA - they only require warnings for Asians? What is this, 1985? They’re letting white people die on purpose. I’ve seen the documents. The CDC knows. The WHO knows. They’re just waiting for enough people to die before they ‘act.’ I’m not paranoid - I’m informed. #DRESSisAMurder
Shubham Dixit
Why does America keep acting like it’s the only country that matters? India has been screening for HLA-B*58:01 since 2014 for high-risk patients. We have over 100 million people on allopurinol. We’ve cut DRESS cases by 70% in just 5 years. Meanwhile, the U.S. is still arguing about whether a $15 test is ‘cost-effective.’ What planet are you on? Your doctors are playing Russian roulette with people’s lives while you sit there complaining about healthcare costs. It’s not a system failure - it’s a moral failure.
KATHRYN JOHNSON
Stop. Just stop. This is not a debate. This is a preventable medical catastrophe. If you are prescribed allopurinol, carbamazepine, or lamotrigine, demand HLA testing before filling the prescription. If your doctor refuses, get a new doctor. Your life is not negotiable. This is not an opinion. It is a standard of care. And if you are reading this and have not been tested - you are at risk. Act now.
Sidhanth SY
I’m from India, took allopurinol last year for gout. Got the HLA test done before even starting - turned out I was positive. Switched to febuxostat. No issues. My dad had DRESS in 2010 - almost died. We don’t wait for tragedy here. We test. Simple. Why does the West make everything so complicated? It’s not about money. It’s about respect for life.
Yanaton Whittaker
Bro. This is why I don’t trust doctors anymore. 😭 I took minocycline for acne. Got a rash. Went to urgent care. They gave me hydrocortisone cream. 3 weeks later, I was in ICU. Liver failure. Now I’m on a 6-month steroid taper. I’m 24. I shouldn’t be this broken. Someone please tell me I’m not the only one who got screwed by this system.
Donna Fleetwood
Thank you for writing this. I’m a nurse who survived DRESS from sulfamethoxazole. Took me 11 months to feel like myself again. I now carry a medical alert card that says ‘DRESS - NO SULFONAMIDES.’ I tell every patient I meet who’s on a high-risk med: ‘Don’t wait. Ask for the test.’ You’re not being paranoid. You’re being smart. And if you’ve had it before - you’re not ‘allergic.’ You’re a walking warning sign. Don’t let anyone tell you otherwise. You’re not broken. You’re a survivor. 💪