When you pick up a generic pill, you assume it’s the same as the brand-name version. Same active ingredient. Same effect. Same safety. But what if the problem isn’t the drug itself - but what’s around it?
The hidden ingredients in your pills
Every pill you swallow contains more than just the medicine your doctor prescribed. It’s packed with chemicals that don’t treat your condition - but still affect your body. These are called excipients. They’re the fillers, binders, dyes, and preservatives that make the drug stable, easy to swallow, or shelf-ready. The FDA defines them as ingredients that have no therapeutic effect. But calling them ‘inactive’ is misleading. In 2019, a major study of over 42,000 oral medications found that 90.2% of them contained at least one excipient linked to allergic reactions or intolerances. That’s not a rare edge case. That’s the norm.On average, a single oral medication contains 8.8 excipients. The most commonly prescribed pills - like those for high blood pressure or thyroid conditions - can have over 80 different formulations just for the same active ingredient. That means two generic versions of the same drug, made by different companies, might have completely different ingredients inside. And if you’re sensitive to one of them, switching generics could make you sick.
Why generics aren’t always interchangeable
The FDA requires generic drugs to be bioequivalent to the brand version. That means the active ingredient must be absorbed into your bloodstream at the same rate and amount - within 80-125% of the original. But that rule says nothing about the other 95% of the pill. The excipients? They can change completely.Take Synthroid, the brand-name thyroid medication. Many patients report feeling worse after switching to a generic version. Why? One common culprit: FD&C Blue #2, a food dye used in some generic formulations. Patients with dye sensitivities report bloating, headaches, rashes, or nausea after the switch. On Reddit, one user wrote: “Switched to generic Synthroid - three days later, I couldn’t stop vomiting. Turned out the generic had Blue #2. I’ve never had a reaction to any other pill.”
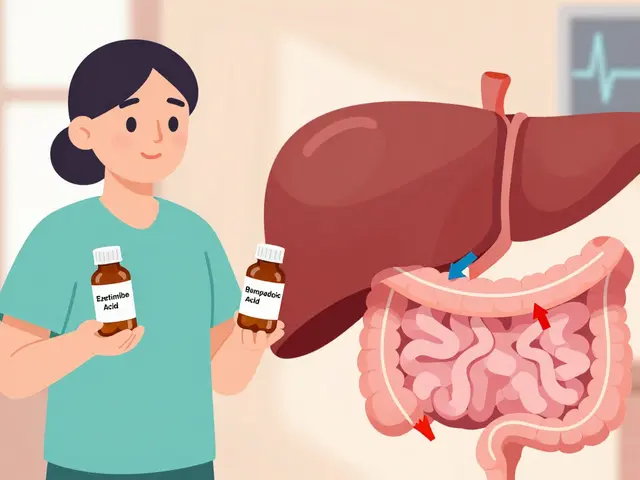
Lactose is another major issue. About 40-60% of oral tablets contain lactose as a filler. For people with lactose intolerance, even small amounts - as little as 1-2 grams - can trigger symptoms like bloating, cramps, and diarrhea. A typical tablet might contain 100-200 mg of lactose. Sounds tiny? Multiply that by three pills a day, and you’re hitting 600 mg. For someone severely sensitive, that’s enough to cause real discomfort. The FDA says lactose intolerance thresholds vary from person to person, but studies show up to 70% of lactose-intolerant patients react when daily intake exceeds 12 grams. And many don’t even realize their stomach issues are drug-related.
Other hidden triggers
Beyond lactose and dyes, other excipients cause real problems:- Parabens - used as preservatives - linked to skin rashes and allergic reactions in sensitive individuals.
- Polysorbate 80 - a solubilizer - associated with anaphylaxis in rare cases.
- FD&C Yellow #5 (Tartrazine) - known to trigger asthma and hives in susceptible people.
- Gluten - not always labeled - can be present as a binder in some generics, posing risks for celiac patients.
- Magnesium stearate - a lubricant - rarely causes issues, but some patients report bloating or gas.
These aren’t theoretical risks. A 2021 study in the Journal of Generic Medicines found that 73.5% of pharmacists had patients report side effects they believed were caused by excipient differences between brand and generic drugs. Independent pharmacists surveyed by the National Community Pharmacists Association found that nearly 7 out of 10 patients had experienced adverse reactions after switching generics.

What the FDA does - and doesn’t - require
The FDA’s rules are clear: for injectables, eye drops, and ear drops, generics must match the brand’s excipients exactly. But for oral tablets and capsules? No such rule. That’s why a generic version of a blood pressure pill might use croscarmellose sodium as a disintegrant, while another uses starch. One might use titanium dioxide for color; another might skip it entirely. Neither is “wrong.” But if you’re sensitive to one, you’ll feel the difference.The FDA maintains the Inactive Ingredient Database (IID), which lists approved excipients and their maximum safe amounts for each route of administration. But this database isn’t easy for patients or even many doctors to use. And manufacturers aren’t required to list all excipients on the label - only the active ingredient and a few major ones. To find the full list, you often need to contact the manufacturer directly or search online databases like Pillbox, run by the National Library of Medicine.
Real-world consequences
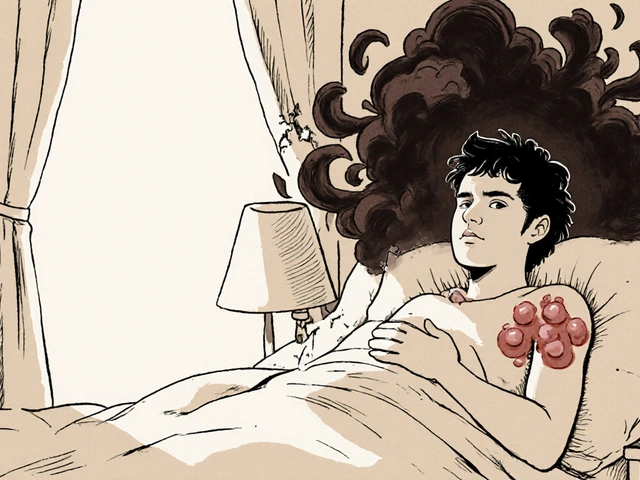
Imagine you’re on a daily medication for depression. You’ve been stable for months. Then your insurance switches you to a cheaper generic. Within days, you’re having panic attacks, insomnia, and nausea. You assume the drug isn’t working. But it’s not the antidepressant - it’s the new capsule’s coating, which contains a dye you’re sensitive to. You stop taking it, thinking the medication failed. You go back to the brand version - and feel fine again. But now your doctor thinks you’re non-compliant or that the drug doesn’t work for you.This happens more than you think. A 2021 survey of 88 healthcare providers showed that only 22.7% documented excipient intolerance in patient records. Most just assumed the patient wasn’t responding to treatment. That’s dangerous. It leads to unnecessary drug switches, misdiagnoses, and worsening symptoms.

What you can do
If you’ve noticed new symptoms after switching to a generic - or after changing manufacturers - don’t ignore it. Here’s what to do:- Track your symptoms. Write down when they started. Did they begin right after a new prescription? Did they go away when you switched back?
- Check the ingredients. Use the FDA’s Inactive Ingredient Database or the Pillbox tool to look up the exact formulation. You’ll need the drug name, strength, and manufacturer.
- Ask your pharmacist. Pharmacists have access to manufacturer data. Ask: “What excipients are in this version?”
- Request a specific brand or manufacturer. If you’re sensitive to lactose, ask for a lactose-free version. Some generics are made without dyes or gluten. They’re not always the cheapest - but they might be the only one you can tolerate.
- Document it. Tell your doctor exactly what you suspect. Write down the excipient name. If you’ve had a reaction, make sure it’s in your medical record.
Pharmacists spend an average of 7.2 minutes per patient investigating these issues. That’s time they’re not spending on other things - because the system doesn’t make it easy. But your health is worth the effort.
The future of excipient safety
The pharmaceutical industry is starting to wake up. In 2023, the FDA launched the Excipient Safety Modernization Initiative to include patient-reported data in their safety database. MIT researchers have already developed an AI tool that predicts individual excipient tolerance based on genetic markers. By 2025, the FDA plans to require full excipient disclosure in electronic prescriptions - meaning your doctor will see the full ingredient list before writing your script.Companies are already responding. The market for specialty excipients - gluten-free, dye-free, lactose-free - hit $18.7 billion in 2022 and is growing fast. Sixty-three percent of pharmaceutical executives believe personalized excipient profiles will be a major differentiator by 2030. That means the future may hold generics tailored to your sensitivities - not just your diagnosis.
For now, the system still treats all patients the same. But your body doesn’t. If you’ve ever felt off after switching pills - even if your doctor says it’s “the same drug” - you’re not imagining it. The excipients matter. And you have the right to know what’s in them.
Are generic drugs always safe if they have the same active ingredient?
No. While the active ingredient must be identical, the excipients - the inactive ingredients - can differ between brand and generic versions or between different generic manufacturers. These differences can cause allergic reactions, intolerances, or absorption issues in sensitive individuals, even if the drug itself works the same way.
Can excipients in generics cause real side effects?
Yes. Common excipients like lactose, FD&C dyes, parabens, and polysorbate 80 have been linked to symptoms such as bloating, nausea, rashes, headaches, and even asthma attacks in sensitive patients. A 2019 study found that over 90% of oral medications contain at least one excipient associated with adverse reactions.
How do I find out what excipients are in my generic medication?
Check the FDA’s Inactive Ingredient Database or use the Pillbox tool from the National Library of Medicine. You’ll need the drug name, strength, and manufacturer. You can also ask your pharmacist to look up the full ingredient list from the manufacturer - they have access to this information.
Is lactose in pills a problem for people with lactose intolerance?
Yes. While most people can tolerate small amounts, sensitive individuals can react to as little as 1-2 grams of lactose per day. Many pills contain 100-200 mg each - so taking three pills a day could exceed your tolerance. Symptoms include bloating, gas, cramps, and diarrhea. Lactose-free versions exist - ask your pharmacist for them.
Should I avoid generics because of excipients?
No - but be informed. Generics are safe and effective for most people. If you’ve never had a reaction, there’s no need to switch. But if you’ve noticed new symptoms after switching formulations, investigate the excipients. You may just need to stick with one manufacturer or request a version without certain additives.
Can my doctor prescribe a specific generic manufacturer?
Yes. If your doctor knows you’re sensitive to certain excipients, they can write “Dispense as Written” or “Do Not Substitute” on your prescription. This prevents the pharmacy from switching to a different generic version without your consent.

Juan Reibelo
Wow. I switched generics last month for my BP med-started getting migraines and thought it was stress. Turns out the new version had FD&C Yellow #5. I didn’t even know dyes were in pills. This is wild. I’m checking every med now.
lorraine england
People act like this is news? I’ve been telling my doctors for years that generics make me feel like garbage. They just shrug and say ‘it’s the same chemical.’ Well, no-it’s the same chemical *in a different candy coating*. And no, I don’t care if it’s cheaper. I’m not a lab rat.
Elizabeth Cannon
ok so i had no idea lactose was in pills?? like… i’m lactose intolerant and i’ve been taking 3 pills a day of my thyroid med for 5 years and i thought my bloating was just ‘me being a weirdo’. turns out it was the filler. i switched to a lactose-free generic and my stomach is finally chill. why isn’t this on the label??
Phil Maxwell
I’ve been on the same generic for years. Never had an issue. But I know people who swear by sticking to one brand. Maybe it’s not about generics vs brand-it’s about consistency. If it works, don’t switch. If it doesn’t, dig into the ingredients. Simple.
Shelby Marcel
wait so if i switch from one generic to another generic… it could be totally different stuff inside?? like… how do i even know what i’m getting? is there a way to just get the same one every time??
Josh McEvoy
MY LIFE IS A LIE. 🤯 I thought I was just ‘sensitive’… turns out I’ve been reacting to BLUE DYE IN PILLS. I’ve cried over this. I’ve been misdiagnosed. I’ve been told I’m ‘anxious’ when I was just vomiting from a capsule. I’m never switching again. I’m paying out of pocket. This is criminal.
Heather McCubbin
Big Pharma doesn’t want you to know this. They profit off your confusion. Why? Because if you knew your meds were full of toxic fillers, you’d demand transparency. But instead, you’re told to ‘just take it’ and shut up. This is control. This is corporate manipulation. Wake up.
venkatesh karumanchi
This is so important. In India, we get generics everywhere-and no one talks about this. I had a friend who got rashes after switching. We found out it was parabens. Now we always check the manufacturer. Small thing, big difference. Thank you for sharing.
Jenna Allison
As a pharmacist, I see this daily. Patients come in saying ‘I feel weird’ after a switch. We pull up the IID, compare excipients, and 80% of the time, it’s a match. Lactose, dyes, gluten-yes. But most docs don’t ask. We’re the ones digging through manufacturer sheets at 11pm. This needs to be easier.
Sharon Biggins
you’re not alone. i used to think i was just ‘bad at taking meds’ until i found out my antidepressant had gluten. now i only take the ones labeled ‘gluten-free’-and my anxiety dropped 70%. don’t blame yourself. blame the system. you’re doing great just by asking questions.
John McGuirk
They’re putting glyphosate in pills. I’ve seen the patents. The FDA is in bed with Big Pharma. You think this is about safety? No. It’s about profit. They don’t care if you get sick. As long as you keep buying pills. They’ll keep adding chemicals. You’re being poisoned. Wake up.
Michael Camilleri
It’s not about the drug-it’s about control. The system wants you dependent. If you knew how many of these pills are filled with synthetic junk, you’d refuse them. But you’ve been trained to trust the white coat. That’s the real illness.
Kevin Waters
My mom has Crohn’s and switched generics for her RA med-got a flare-up. We called the manufacturer, found out it had corn starch (her allergen). Switched back to the original generic. Done. Took 10 minutes. No drama. Just ask your pharmacist. Seriously.
Dolores Rider
EVERY TIME I SWITCH I GET A HEADACHE. I thought it was my brain. Turns out it’s the dye. I’m done. I’m paying $15 more for the same pill. I’d rather be broke than sick. And no, I don’t care what you say. This is my body. 🤬
Darren Links
Why are we letting Big Pharma control our health? In America, we pay more for drugs than anywhere else. And now we’re being poisoned by fillers? This is why we need single-payer. So they can’t hide behind ‘market competition.’ This is a national disgrace.