Every year, thousands of people with G6PD deficiency have life-threatening reactions to common medications - not because they’re careless, but because many doctors don’t test for it. If you or someone you know has this condition, knowing which drugs to avoid isn’t just helpful - it’s a matter of survival.
What Is G6PD Deficiency?
G6PD deficiency is a genetic condition that affects how your red blood cells handle stress. Your body uses an enzyme called glucose-6-phosphate dehydrogenase to protect those cells from damage caused by oxidation. When this enzyme is missing or weak, even small amounts of certain drugs, foods, or infections can cause your red blood cells to burst - a process called hemolysis.
This isn’t rare. Around 400 million people worldwide have it. It’s most common in people with ancestry from Africa, the Mediterranean, Southeast Asia, and the Middle East. In some regions, up to 20% of the population carries the gene. And while it’s often called a "male disease," women can be affected too - about 15% of female carriers experience hemolysis due to how X-chromosomes work.
There are over 200 known variants of G6PD deficiency. The most common ones are:
- G6PD A- - found in 90% of African descent cases
- G6PD Mediterranean - common in Southern Europe and the Middle East
- G6PD Canton - dominant in China and Southeast Asia
Class III deficiency (moderate enzyme activity) is the most common globally. People with this type can live normally - unless they take the wrong meds.
Why Do Certain Drugs Cause Hemolysis?
Red blood cells don’t have the ability to repair themselves like other cells. They rely entirely on G6PD to keep their internal environment stable. When you take a drug that causes oxidative stress, your body produces free radicals. Normally, glutathione - a natural antioxidant - neutralizes them. But without enough G6PD, glutathione can’t be replenished fast enough.
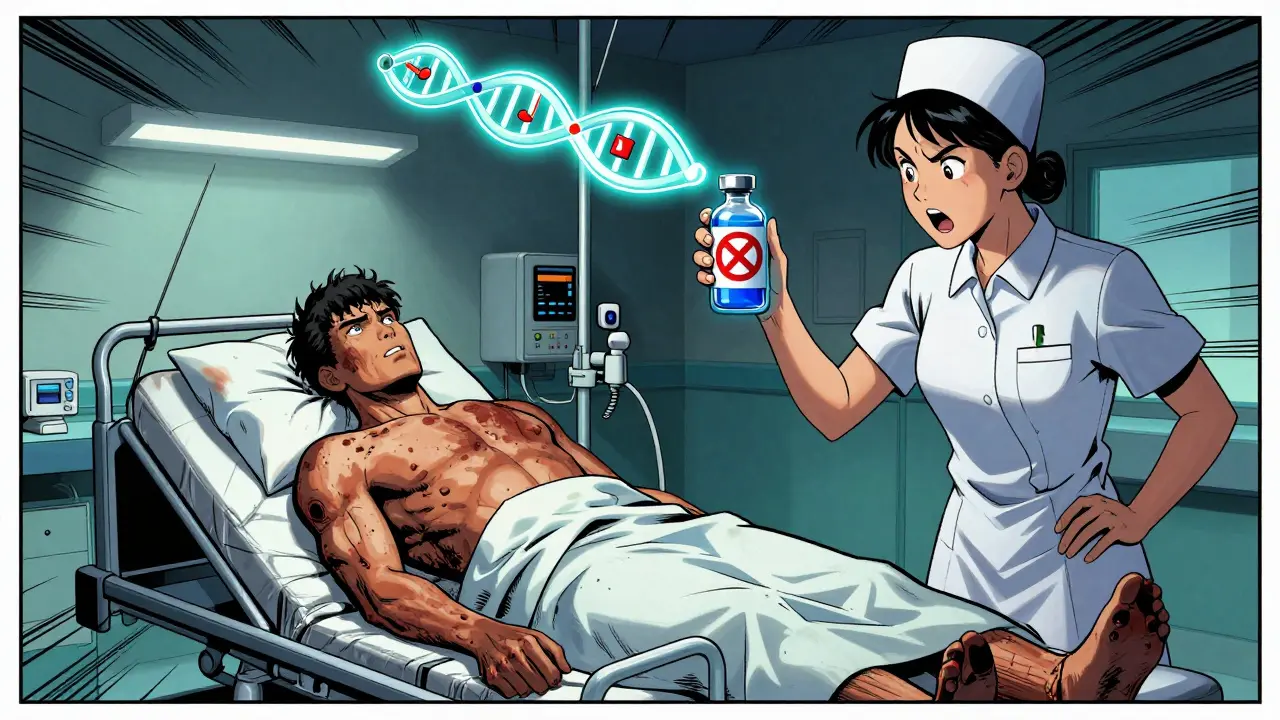
The result? Red blood cells get damaged, break apart, and flood your bloodstream with hemoglobin. That’s when you start seeing symptoms: dark urine (like cola), jaundice (yellow skin), extreme fatigue, shortness of breath, and rapid heartbeat. In severe cases, hemoglobin can drop from 14 g/dL to under 6 g/dL in less than a week - enough to require a blood transfusion.
It’s not just about the drug itself. The risk depends on your specific G6PD variant. Someone with Mediterranean G6PD might have a severe reaction to a single dose of primaquine. Someone with African G6PD might tolerate the same dose without issue. That’s why blanket warnings aren’t enough - you need to know your type.
Medications That Can Trigger Hemolysis
There are 87 medications currently flagged by the WHO as high-risk for G6PD-deficient patients. Here are the most dangerous ones you need to know:
- Rasburicase - used to treat tumor lysis syndrome. This drug directly produces hydrogen peroxide. In G6PD-deficient patients, it causes rapid, massive hemolysis. The FDA has a black box warning: never give it without testing first.
- Methylene blue - used for methemoglobinemia. It’s a strong oxidizing agent. In one 2021 case, a patient’s hemoglobin dropped from 14.2 to 5.8 g/dL in 48 hours after receiving it. He needed three units of blood.
- Primaquine - used to treat malaria, especially Plasmodium vivax. Until recently, it was given without testing. Now, WHO requires G6PD testing before use. Without it, Class I and II patients face near-certain hemolysis.
- Dapsone - used for leprosy and some skin conditions. Doses over 50mg/day are dangerous. Even lower doses can cause problems in sensitive individuals.
- Sulfonamides - antibiotics like sulfamethoxazole (Bactrim). While not all are equally risky, many are avoided out of caution.
Some drugs are less clear-cut. Sulfonylureas like glyburide (used for diabetes) carry warnings on 92% of labels - but only 17 confirmed cases of hemolysis exist since 1965. Experts say these warnings are outdated and scare patients unnecessarily.
Safe Alternatives
You don’t have to avoid all treatment. Many safe options exist:
- Chloroquine - safe for malaria prevention in all G6PD variants
- Tafenoquine - a newer alternative to primaquine, but only if G6PD testing confirms you’re not deficient
- Artemisinin-based combination therapies - first-line for malaria, safe across all classes
- Atovaquone-proguanil (Malarone) - recommended for travelers with G6PD deficiency going to malaria zones
- Penicillins and cephalosporins - generally safe antibiotics
For pain relief, acetaminophen (Tylenol) is safe. Avoid aspirin and other NSAIDs unless approved by a doctor familiar with your G6PD status.
Testing Is the Key to Prevention
There’s no cure for G6PD deficiency. Prevention is everything. And the best prevention? Testing.
Standard blood tests can’t detect it. You need a specific test:
- Fluorescent spot test - fast, cheap, and 98.7% accurate. Results in 15 minutes. Used in newborn screening programs.
- Quantitative spectrophotometric assay - measures exact enzyme activity. Used to classify severity (Class I-V).
- Genetic testing - identifies the specific mutation. Useful for family planning or complex cases.
Important: Don’t test right after a hemolytic episode. Your body produces new red blood cells that have normal enzyme levels. This can give a false negative. Wait at least three months after a crisis to get accurate results.
In countries like Saudi Arabia, universal newborn screening reduced hospital admissions for hemolysis by 78% between 2010 and 2020. In Thailand, mandatory testing before primaquine use dropped hemolytic episodes from 15% to 0.3%.
What to Do If You’ve Already Been Exposed
If you took a risky drug and now feel dizzy, have dark urine, or your skin looks yellow:
- Stop the medication immediately.
- Drink plenty of water to flush your kidneys.
- Seek emergency care. You may need blood tests (hemoglobin, reticulocyte count, bilirubin), IV fluids, or even a transfusion.
- Inform your doctor about your G6PD status - even if you weren’t diagnosed before.
Early intervention can prevent kidney failure and other complications. Don’t wait.
Living With G6PD Deficiency
Most people with G6PD deficiency live normal lives - if they know their limits.
Here’s what works:
- Carry a medical alert card - list your condition and the top 5 dangerous drugs.
- Keep a list of safe alternatives - share it with every doctor you see.
- Ask before taking any new medication - even over-the-counter ones. Herbal supplements like fava beans, menthol, and naphthalene (mothballs) can also trigger hemolysis.
- Get tested if you’re from a high-risk region - even if you’ve never had symptoms.
- Teach your family - if you have children, they may inherit it.
Patients who received detailed education on triggers had a 92% no-episode rate over five years. Those who didn’t? Only 38% avoided another crisis.
The Bigger Picture
Despite knowing this for over 70 years, G6PD deficiency is still under-tested and under-treated. In the U.S., only 12 states require newborn screening. In Africa, only 18 of 47 countries have national programs. Meanwhile, the global market for G6PD testing is growing fast - $187 million in 2023, projected to hit $313 million by 2028.
Why? Because the tools are finally here. In January 2024, the FDA approved the first point-of-care G6PD test that gives results in 8 minutes. It’s accurate to 99.1%. That means in emergency rooms, before giving rasburicase or methylene blue, you can test - and save a life - in under 10 minutes.
Research is also moving forward. Early trials are testing N-acetylcysteine (NAC) to protect red blood cells during exposure to risky drugs. In the lab, NAC reduced hemolysis by 75% when given with primaquine. And by late 2024, the first enzyme replacement therapy trials will begin.
By 2035, preventable deaths from G6PD deficiency could be nearly eliminated - but only if testing becomes standard.
Frequently Asked Questions
Can G6PD deficiency be cured?
No, G6PD deficiency is a genetic condition and cannot be cured. But it can be managed effectively by avoiding oxidative triggers like certain medications, foods, and infections. Most people live normal, healthy lives with proper awareness and precautions.
Is G6PD deficiency only a problem for men?
No. While it’s X-linked and more common in men, women can also be affected. Due to X-chromosome inactivation, about 15% of female carriers have low enough enzyme levels to experience hemolysis. Many women are misdiagnosed because doctors assume only males are at risk.
Can I take ibuprofen or Tylenol if I have G6PD deficiency?
Acetaminophen (Tylenol) is generally safe. Ibuprofen and other NSAIDs are usually okay in standard doses, but some doctors recommend caution. Always check with your provider - especially if you’ve had a previous reaction. When in doubt, choose acetaminophen.
What should I do if I’m traveling to a malaria area?
Avoid primaquine and chloroquine unless you’ve been tested. Use atovaquone-proguanil (Malarone) instead - it’s safe for G6PD-deficient travelers. If you must use tafenoquine, you need a confirmed normal G6PD test result. Always carry proof of your status and a list of safe alternatives.
How do I know if I have G6PD deficiency?
If you’re from a region with high prevalence (Africa, Mediterranean, Southeast Asia) or have had unexplained jaundice, dark urine, or anemia after taking certain drugs, get tested. The fluorescent spot test is quick, affordable, and widely available. Don’t wait for symptoms - prevention is the only reliable strategy.
Can I donate blood if I have G6PD deficiency?
Yes. Your blood is safe to donate. However, if you’re donating for someone with G6PD deficiency, inform the blood bank - they may avoid using your red blood cells in transfusions for G6PD-deficient recipients due to potential oxidative stress from storage.
Next Steps
If you’ve never been tested and you’re from a high-risk background, get a fluorescent spot test now. It takes 15 minutes and costs less than $20 in many clinics.
If you’ve had a hemolytic episode, keep a written list of all drugs you can’t take. Bring it to every doctor’s appointment. Ask for a copy of your G6PD test results - don’t assume they’re in your chart.
If you’re a parent, ask your pediatrician if your newborn was screened. If not, request it. In the U.S., screening is not mandatory in most states - but it should be.
Knowledge saves lives. G6PD deficiency doesn’t have to be a hidden danger. With the right information and testing, it’s a condition you can live with - safely - for your whole life.


Brendan F. Cochran
So let me get this straight-we’re spending millions on tests while people die from drugs that’ve been around since the 70s? And the FDA only just approved a point-of-care test in 2024? This isn’t medicine, it’s corporate negligence with a side of bureaucratic laziness. We test for everything except what actually kills people. Wake up, America.
jigisha Patel
While the article presents a comprehensive overview of G6PD deficiency and its pharmacological implications, it fails to adequately address the heterogeneity of enzyme kinetics across variants. The conflation of Class III with global prevalence statistics is statistically misleading-G6PD A- exhibits markedly different oxidative thresholds than Mediterranean variants, and clinical guidelines must reflect this. Furthermore, the assertion that sulfonylureas are ‘outdated’ in warnings is unsupported by longitudinal cohort data from South Asian populations, where hemolytic events remain documented despite low incidence.
Jason Stafford
They don’t want you to know this-but the real reason G6PD testing isn’t mandatory is because Big Pharma doesn’t profit from it. Think about it: if everyone got tested before taking primaquine or methylene blue, those drugs would be used way less. And who controls the labs? Who owns the patents on those tests? It’s the same people who profit from transfusions, ICU stays, and kidney dialysis after hemolysis. This isn’t about health-it’s about control. They’d rather keep you blind than lose billions.
Justin Lowans
This is one of the most important public health pieces I’ve read in years. The clarity around safe alternatives-especially Malarone and artemisinin-based therapies-is a game-changer for travelers and clinicians alike. The data on newborn screening reducing admissions by 78% in Saudi Arabia should be a wake-up call for every state legislature. We have the tools. We just need the will. Let’s push for mandatory screening in every state. Lives depend on it.
Stephen Craig
Knowledge is prevention. Prevention is peace.
Connor Hale
I’ve had G6PD deficiency my whole life and never knew it until I got jaundice after a flu shot. Turns out, the flu shot was fine-but the OTC cold medicine I took with it wasn’t. I wish someone had told me sooner. Now I carry a card in my wallet. Simple. Cheap. Life-saving. Why isn’t this taught in high school biology?
Abhishek Mondal
While the article is commendably thorough, it exhibits a troubling Anglo-centric bias: it references U.S. and Saudi data as benchmarks, yet ignores the vast, under-documented G6PD variants in the Indian subcontinent-particularly the G6PD Delhi and G6PD Mahidol variants, which exhibit unique pharmacokinetic sensitivities not captured by Western classifications. Furthermore, the dismissal of sulfonylurea risks as 'outdated' is not only premature but dangerously reductive; Indian clinical registries report 47 confirmed cases since 2015, predominantly in diabetic patients with coexisting renal impairment. The author’s reliance on WHO guidelines without contextualizing regional metabolic differences is a critical oversight.
Joseph Snow
Let’s be real-this whole G6PD testing push is just another way for hospitals and labs to bill more. The ‘black box warning’ on rasburicase? That’s not safety-it’s liability insurance. And don’t get me started on the ‘point-of-care test’-it’s barely 99.1% accurate. That’s still one in a hundred false negatives. Meanwhile, the FDA approved it because the manufacturer donated to their advisory board. This isn’t medicine. It’s a money machine disguised as science.