It’s not uncommon to feel a little off after taking a new medication. Maybe your stomach feels queasy, or you get a mild headache. But if you break out in hives, your lips swell up, or you can’t breathe, that’s not just a side effect - it could be a drug allergy. And unlike regular side effects, drug allergies involve your immune system reacting as if the medicine is a threat. This isn’t something you can just tough out. Knowing the difference between a nuisance and a danger can save your life.
What Exactly Is a Drug Allergy?
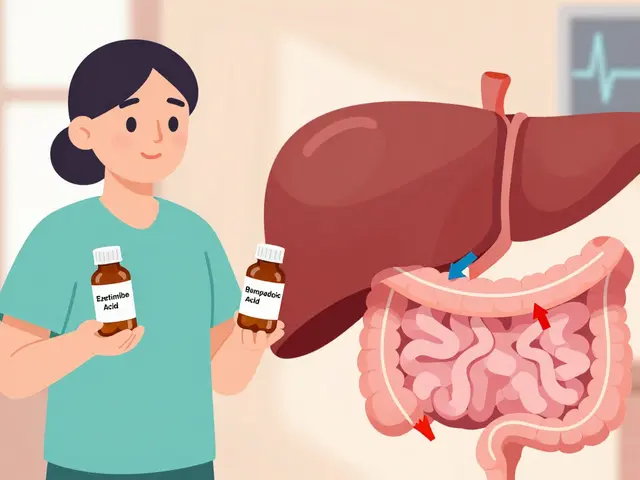
A drug allergy happens when your immune system mistakenly identifies a medication as harmful. It’s not the same as nausea from antibiotics or dizziness from blood pressure pills - those are side effects, not allergies. Allergies trigger your body to release chemicals like histamine, which cause symptoms ranging from itchy skin to full-blown shock. The key? It’s unpredictable. One person might take penicillin with no issues, while another breaks out in hives after one pill. That’s why you can’t assume you’re safe just because someone else handled the drug fine.
According to the National Institutes of Health, about 10% of people in the U.S. are incorrectly labeled as allergic to drugs. Many of them aren’t allergic at all - they just had a side effect or a virus that looked like a reaction. But mislabeling has real consequences. Doctors avoid the drug, even if it’s the best treatment. That means you might get a stronger, more expensive, or riskier antibiotic instead. In some cases, it leads to longer hospital stays or worse infections like C. diff.
Common Signs of a Drug Allergy
Drug allergies show up in different ways, and timing matters. Some reactions hit fast. Others creep in over days or weeks.
- Hives - Raised, red, itchy welts that can appear anywhere on your body. They often come and go, shifting locations.
- Itching - Not just skin-deep. You might feel it in your eyes, throat, or even deep inside your mouth.
- Swelling - Lips, tongue, eyelids, or throat. Swelling in the throat is dangerous. It can block your airway.
- Rash - Flat red patches or small bumps. These can show up days after starting the drug, even if you’ve taken it before without issue.
- Difficulty breathing - Wheezing, tightness in your chest, or feeling like you can’t get enough air. This is a red flag.
- GI symptoms - Nausea, vomiting, diarrhea, or cramping. When paired with skin or breathing issues, it’s more likely an allergy.
Some reactions are delayed. A rash might not show up until 5 to 10 days after starting the drug. That’s often a sign of a type called drug exanthem. It’s usually not life-threatening, but it still needs medical attention.
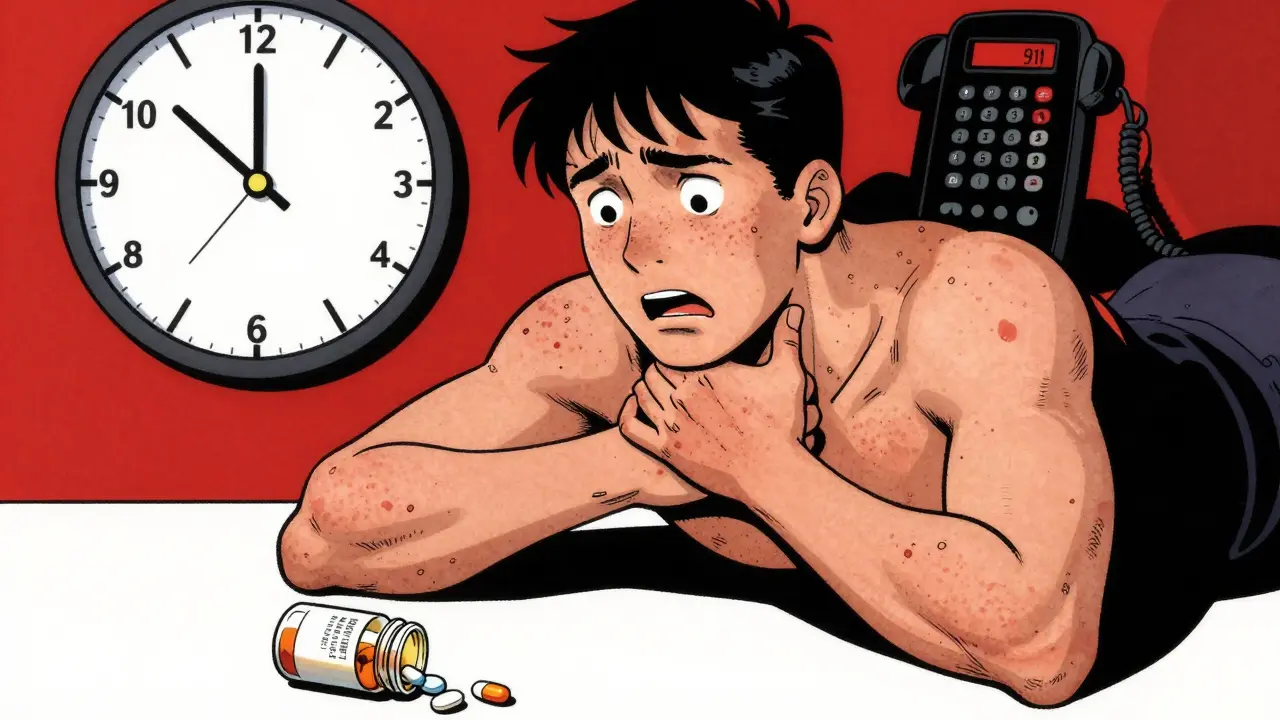
When It’s an Emergency: Anaphylaxis
Anaphylaxis is the most dangerous drug allergy reaction. It hits fast - often within minutes to an hour after taking the drug. It affects two or more body systems at once. For example:
- Skin rash + trouble breathing
- Swelling + vomiting + dizziness
- Hives + low blood pressure + loss of consciousness
If you or someone else has these signs, call 911 immediately. Don’t wait. Don’t try to drive yourself. Anaphylaxis can kill in under an hour if untreated. Epinephrine is the only treatment that stops it. If you’ve had a serious reaction before, your doctor should have given you an epinephrine auto-injector (like an EpiPen). Carry it everywhere. Know how to use it. Teach someone close to you how to use it too.

Delayed Reactions You Can’t Ignore
Not all dangerous reactions happen right away. Some show up weeks later. Two serious ones to watch for:
- Serum sickness-like reaction - Fever, joint pain, swollen lymph nodes, and a rash that looks like hives. This usually starts 1 to 3 weeks after taking the drug. Common culprits include antibiotics like penicillin or anti-seizure meds.
- DRESS syndrome - Drug Reaction with Eosinophilia and Systemic Symptoms. This is rare but deadly. Signs include a widespread rash, high fever, swollen glands, liver inflammation, and abnormal blood counts. It can come back even after stopping the drug. If you suspect DRESS, get to a hospital right away.
Another life-threatening reaction is Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN). It starts like the flu - fever, sore throat, burning eyes - then the skin begins to blister and peel. Mucous membranes in your mouth, eyes, and genitals are often affected. If more than 10% of your skin detaches, it’s classified as TEN. These are medical emergencies. Survival depends on rapid hospital care.
What to Do If You Suspect a Drug Allergy
If you think you’re having a reaction, stop taking the drug - but don’t just quit cold turkey. Some meds need to be tapered. Call your doctor. If it’s mild - just a rash or itching - schedule an appointment. Take photos of the rash. Write down when you started the drug, what symptoms you had, and when they started. This helps your doctor figure out what’s going on.
If symptoms are severe - swelling, trouble breathing, dizziness, or skin peeling - go to the ER. Don’t wait. Don’t text your doctor. Go. Emergency rooms are equipped to handle anaphylaxis and other life-threatening reactions. Afterward, ask for a referral to an allergist. They’re the only ones trained to properly test for drug allergies.
Testing and Diagnosis: It’s Not as Simple as You Think
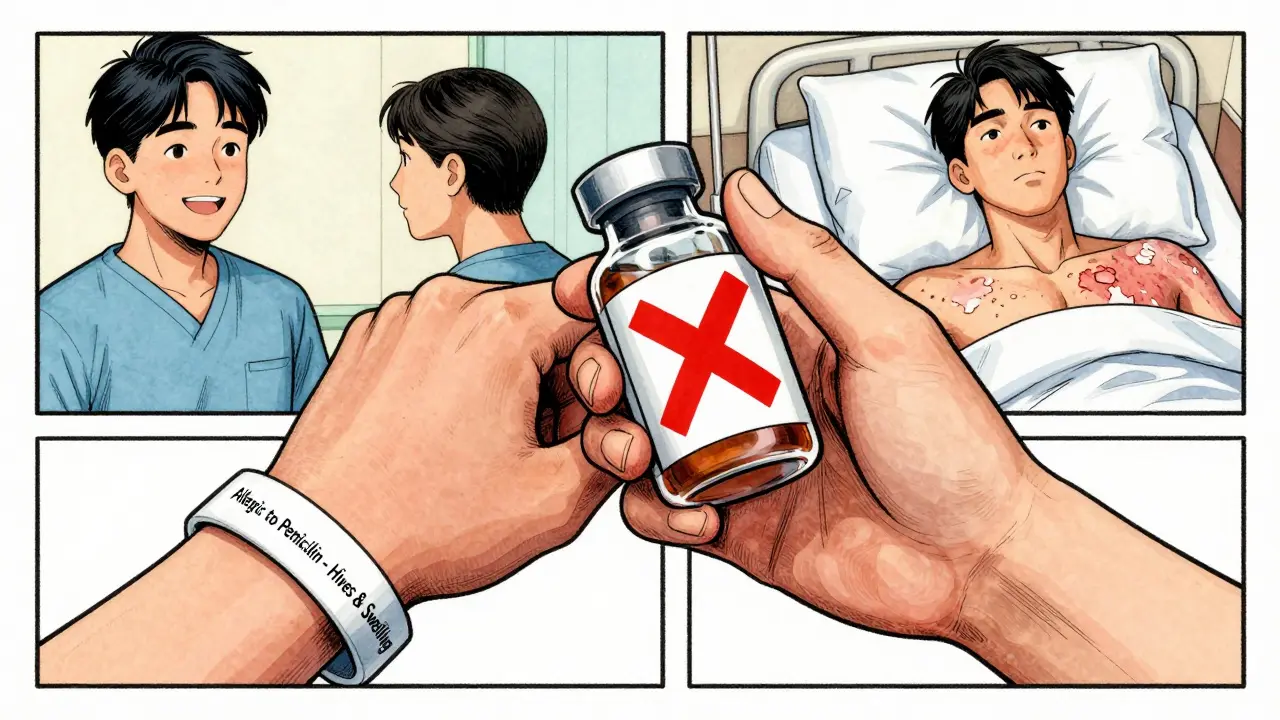
There’s no universal blood test for drug allergies. For most drugs, diagnosis relies on your history - what happened, when, and how bad it was. The exception? Penicillin. Skin testing for penicillin allergy is reliable. If you think you’re allergic, an allergist can test you. Studies show over 90% of people who say they’re allergic to penicillin aren’t - they just had a side effect years ago. Getting tested can open up better, safer treatment options.
For other drugs, if the reaction was serious, your doctor might recommend a controlled challenge - giving you a tiny, monitored dose of the drug to see if you react. This only happens in a clinic with emergency equipment on hand. Never try this at home.
For delayed reactions like DRESS, a blood test might help check for high white blood cells or liver damage. But even then, it’s not a direct allergy test. It just supports the diagnosis.
How to Protect Yourself Moving Forward
Once you know you have a drug allergy, you need to make sure every doctor, pharmacist, and hospital knows too. Keep a list of all drugs you’re allergic to - including the reaction you had. Don’t just write “penicillin allergy.” Write “hives and swelling after amoxicillin, 2023.” Specifics help.
Consider wearing a medical alert bracelet. It’s a small thing, but in an emergency, it can save your life. Tell family members what to do if you react. Make sure your pharmacy has your allergy list on file. When you get a new prescription, ask: “Is this safe for someone with a drug allergy to [name the drug]?”
Don’t assume you’ll outgrow it. Some allergies last a lifetime. Others fade. Only a specialist can tell you if you’re still allergic. Don’t guess. Get tested.
Why This Matters More Than You Realize
Every year in the U.S., over a million people end up in the emergency room because of drug reactions - not all allergic, but many are. Mislabeling adds to the problem. People avoid penicillin because they think they’re allergic, then get treated with stronger antibiotics that cost more and cause more side effects. That’s why accurate diagnosis isn’t just personal - it’s public health.
Knowing the signs, acting fast, and getting proper testing can prevent unnecessary risks. You don’t need to live in fear of medication. You just need to know what to watch for - and when to act.
Can you suddenly become allergic to a drug you’ve taken before?
Yes. Your immune system can change over time. You might take an antibiotic several times without issue, then suddenly develop hives or swelling on the next dose. This doesn’t mean you were allergic before - it means your body started reacting to it now. That’s why you should never assume a drug is safe just because you’ve used it in the past.
Is a rash always a sign of a drug allergy?
No. Many rashes from drugs are not allergic. They’re side effects - like a mild, non-itchy rash from amoxicillin in kids, which is common and harmless. Allergic rashes usually itch, spread quickly, and may come with other symptoms like swelling or breathing trouble. If you’re unsure, take a photo and show your doctor.
Can I take a different drug in the same class if I’m allergic to one?
Maybe - but don’t assume it’s safe. If you’re allergic to penicillin, you might still react to amoxicillin or other penicillin-type antibiotics. For other drug classes, like sulfa drugs or NSAIDs, cross-reactivity varies. Only an allergist can tell you if it’s safe based on your history and testing.
How long do drug allergy symptoms last?
It depends. Hives and itching often go away within hours or days after stopping the drug. Rashes from delayed reactions can last weeks. Serious reactions like SJS or DRESS can take months to heal and may need hospital care. Even after symptoms fade, your immune system may still remember the drug - so avoid it unless tested.
Should I carry an epinephrine pen for every drug allergy?
Only if you’ve had a life-threatening reaction like anaphylaxis. If your reaction was limited to a rash or mild swelling, you likely don’t need one. But if you’ve ever had trouble breathing, swelling in your throat, or low blood pressure after a drug, your doctor should prescribe an epinephrine auto-injector. Keep it with you, check the expiration date, and replace it on time.
Can drug allergies be cured?
Not exactly. Once your immune system reacts to a drug, it usually remembers it. But some people outgrow allergies over time - especially to penicillin. The only way to know for sure is through proper testing by an allergist. Never stop avoiding a drug just because you think you’re fine now. Get tested before trying it again.



Ambrose Curtis
i took amoxicillin once and broke out in hives like a damn tornado. thought it was just a rash till my lips swelled up and i nearly choked on my own spit. 911 called, epipen saved my life. now i wear a bracelet that says 'ALLERGIC TO PENICILLIN' and i don't care who thinks it's dramatic. better safe than dead.
Linda O'neil
THIS. So many people think 'side effect' and 'allergy' are the same. Big difference. My sister got mislabeled allergic to ibuprofen because she got a stomach ache once. She couldn't get pain relief for years. Got tested last year-turns out she's fine. Now she takes Advil like candy. Don't assume, get tested.
Chris Urdilas
oh cool so now i'm supposed to carry an epi-pen because i got a tiny itchy rash once? next you'll tell me to wear a helmet when i eat peanut butter. lol. also, 'DRESS syndrome'? sounds like a bad sci-fi movie. but yeah, if you're actually dying, go to the er. otherwise, stop scaring people with medical jargon.
Jeffrey Carroll
It is imperative that individuals recognize the distinction between adverse drug reactions and true immunologic hypersensitivity. Misclassification not only compromises therapeutic efficacy but also contributes to increased healthcare expenditures and antimicrobial resistance. I strongly encourage consultation with a board-certified allergist for accurate diagnostic evaluation.
Phil Davis
so you're telling me the same drug that gave my cousin a rash last year could kill me tomorrow? thanks for the reassurance. i'm just glad my doctor doesn't trust me enough to give me anything strong. guess i'll just suffer in silence with my migraines and my 'probably not allergic' label.
Irebami Soyinka
USA always overmedicalize everything 😂. In Nigeria, if you get rash from medicine, you drink bitter leaf water and pray. No epipen. No hospital. Just faith and patience. But hey, if you wanna pay $2000 for a test to find out if you're allergic to aspirin-go ahead, my brother. We still alive here without your fancy alarms. 🙏💊
doug b
you don't need to panic, but you DO need to pay attention. If you feel weird after a pill, stop it. Take a pic of the rash. Call your doc. Don't wait till you're gasping. I've seen too many people ignore early signs and end up in ICU. Be smart. Not scared. Smart.
SRI GUNTORO
People these days are too lazy to read the leaflet. If you take a drug without knowing the risks, you deserve what you get. I’ve never had an allergy because I read the warnings. You think your body is special? It’s not. Stop blaming the medicine and start taking responsibility.
Kevin Kennett
my aunt had SJS after a sulfa antibiotic. skin peeled off her arms like sunburn. spent 6 weeks in the burn unit. she’s alive now, but her eyes never healed right. i carry her story with me. if you think it's 'just a rash'-you haven't seen what happens when it goes wrong. don't gamble with your body.
Jess Bevis
Penicillin allergy? Get tested. 90% aren't really allergic. Save yourself the trouble.