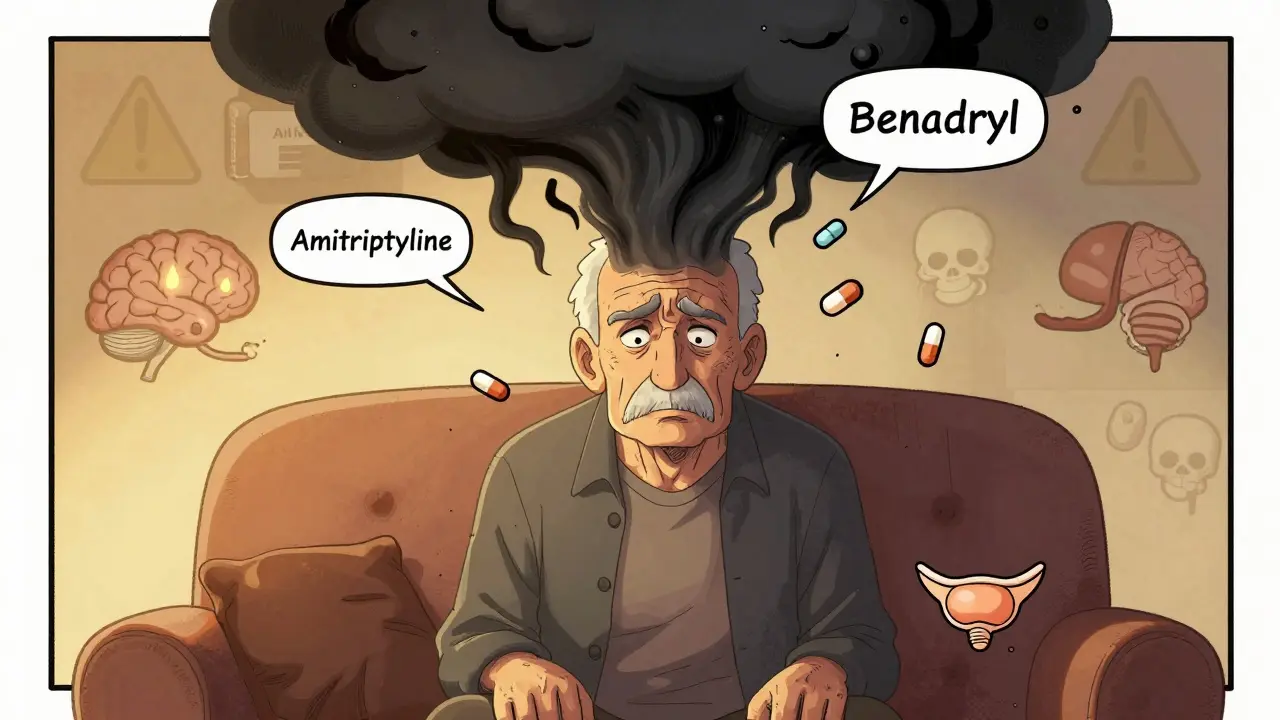
Combining tricyclic antidepressants (TCAs) with first-generation antihistamines isn’t just a routine prescription-it’s a ticking time bomb for many older adults. While doctors may prescribe amitriptyline for chronic pain and diphenhydramine for allergies or sleep, few realize how dangerously these drugs stack up in the body. Together, they trigger anticholinergic overload, a condition that quietly shuts down vital brain functions, often leading to confusion, memory loss, urinary retention, and even hospitalization.
What Exactly Is Anticholinergic Overload?
Anticholinergic overload happens when too many drugs block acetylcholine, a key chemical messenger in your nervous system. Acetylcholine helps with memory, muscle control, digestion, and alertness. When it’s blocked, your brain and body start to slow down. TCAs like amitriptyline, clomipramine, and imipramine were designed to affect serotonin and norepinephrine-but they also strongly block muscarinic receptors. First-generation antihistamines like diphenhydramine (Benadryl), hydroxyzine, and promethazine do the same thing. When taken together, their effects multiply, not add up.Think of it like turning off multiple lights in a room. One light off? You can still see. But turn off ten? You’re in the dark. That’s what happens in the brain. A 2022 study in Pharmacoepidemiology and Drug Safety found that patients taking both a TCA and diphenhydramine had a 54% higher risk of developing dementia over time. Even short-term use can cause acute delirium-especially in people over 65.
Why This Combination Is So Dangerous
The problem isn’t just that both drugs are anticholinergic. It’s that they hit the same receptors, at the same time, in the same vulnerable people. Older adults naturally produce less acetylcholine and metabolize drugs slower. Their kidneys and liver can’t clear these medications as quickly, so levels build up. A typical dose of amitriptyline (25-100 mg) and diphenhydramine (25-50 mg) can push total anticholinergic burden into the danger zone.Here’s how bad it gets:
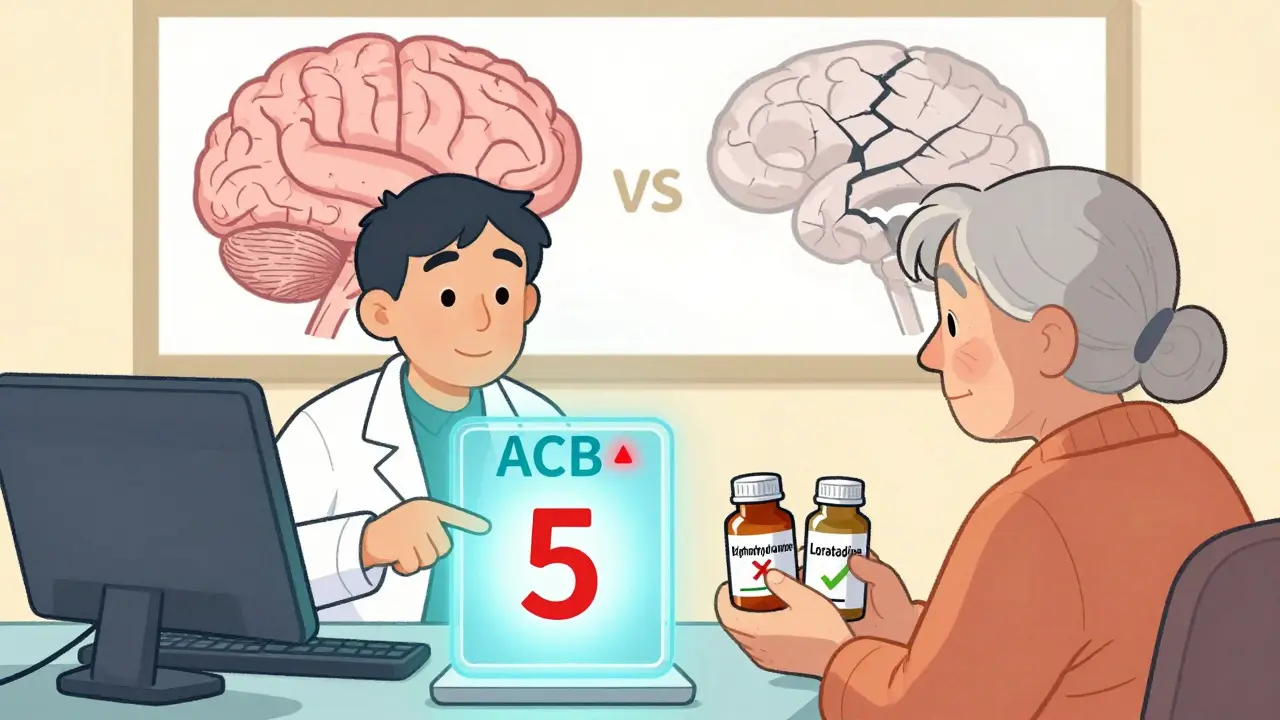
- Amitriptyline scores a 3 on the Anticholinergic Cognitive Burden (ACB) scale-the highest possible.
- Diphenhydramine scores a 2.
- Together? That’s a score of 5. Research shows that a score of 4 or higher doubles the risk of dementia.
And it’s not just memory. Patients report dry mouth, constipation, blurred vision, fast heartbeat, trouble urinating, and sudden confusion. One Reddit user, a medical resident, shared: “I’ve seen three elderly patients admitted with delirium-all because their primary care doctor added Benadryl to their amitriptyline for sleep.”
Who’s Most at Risk?
It’s not just the elderly. Anyone with kidney or liver disease, Parkinson’s, glaucoma, or an enlarged prostate is at higher risk. But older adults are the most vulnerable. According to the American Geriatrics Society’s 2023 Beers Criteria, combining first-generation antihistamines with TCAs is a “potentially inappropriate medication” for anyone over 65.Here’s a real case from a 2020 Elsevier study: A 72-year-old woman with chronic back pain was on 50 mg of amitriptyline. Her doctor added 25 mg of diphenhydramine at night for insomnia. Within two weeks, she stopped recognizing her grandchildren, couldn’t find the bathroom, and couldn’t urinate. She ended up in the ER with acute urinary retention and anticholinergic delirium. Her ACB score was 5. She was discharged after five days-but her cognitive decline never fully reversed.
What About Newer Antidepressants?
You might think switching to an SSRI like sertraline or fluoxetine solves the problem. But here’s the twist: even some SSRIs can interact with TCAs or antihistamines in dangerous ways. Fluoxetine, for example, slows down the liver enzyme CYP2D6, which is needed to break down amitriptyline. That means amitriptyline levels can spike-increasing toxicity risk even without antihistamines.And not all TCAs are equal. Nortriptyline and desipramine have lower anticholinergic effects than amitriptyline or clomipramine. But even then, adding diphenhydramine still pushes the risk up. The bottom line: if you’re on a TCA, avoid first-gen antihistamines entirely.
What Are the Safer Alternatives?
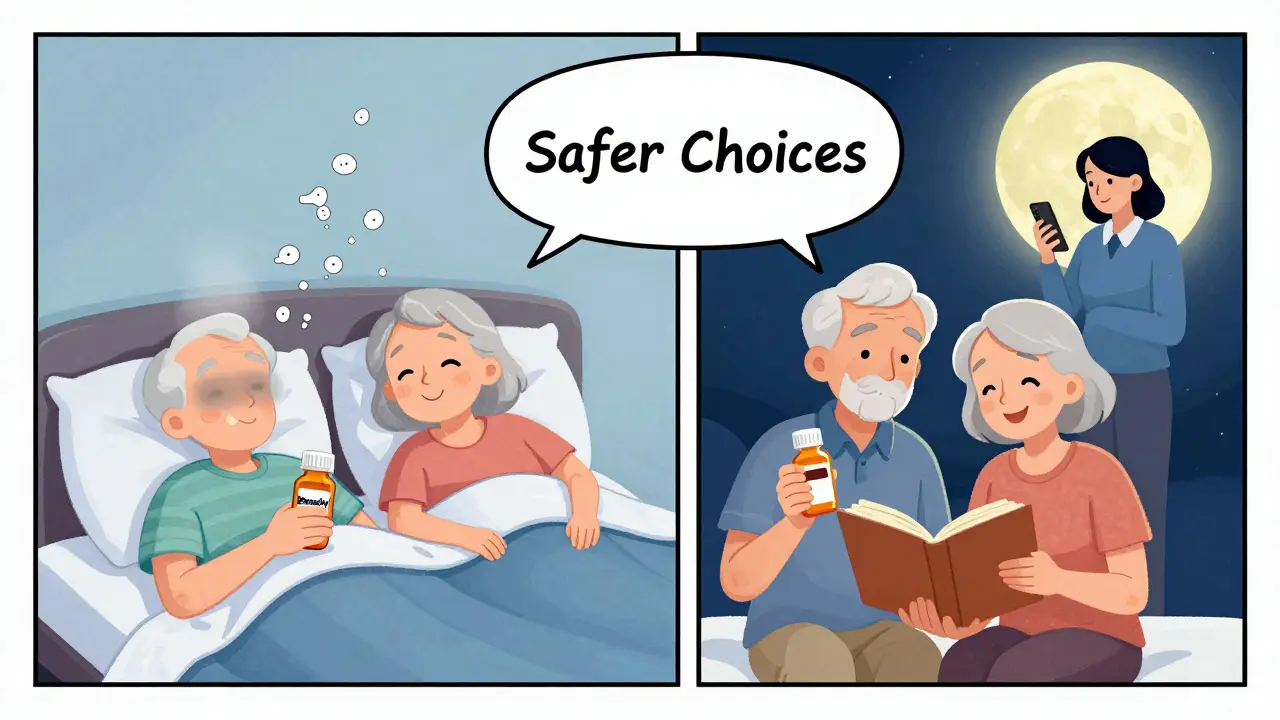
You don’t have to suffer through allergies or insomnia just because you’re on a TCA. There are better options:- Second-generation antihistamines: Loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) have almost zero anticholinergic activity. Their ACB score is 0. They work just as well for allergies without the brain fog.
- For sleep: Skip diphenhydramine. Try melatonin (0.5-5 mg), magnesium glycinate, or cognitive behavioral therapy for insomnia (CBT-I). CBT-I is proven to work better than sleep meds long-term.
- For chronic pain: If you’re on amitriptyline for nerve pain, ask your doctor about gabapentin, pregabalin, or even low-dose nortriptyline instead.
One 2023 study in the Journal of the American Geriatrics Society followed 217 older adults who stopped all anticholinergic meds. After 18 months, their cognitive scores improved by 34%. That’s not a small gain-it’s life-changing.
How to Spot Anticholinergic Overload
If you or a loved one is on a TCA and an antihistamine, watch for these signs:- Sudden confusion or disorientation
- Memory lapses that aren’t normal for age
- Difficulty urinating or complete inability to void
- Very dry mouth, constipation, or blurred vision
- Unexplained drowsiness or slurred speech
- Fast heartbeat or dizziness when standing up
If you see even one of these, stop the antihistamine immediately and call your doctor. Don’t wait. Anticholinergic delirium can escalate fast.
What Your Doctor Should Be Doing
Most doctors don’t check anticholinergic burden. But they should. Tools like the ACB scale are free, simple, and built into many electronic health records now. Epic, Cerner, and other major systems flag TCA-antihistamine combinations with hard stops-92% of attempts to prescribe them together trigger an alert, according to a 2022 JAMIA study.Ask your doctor:
- “What’s the anticholinergic burden of my medications?”
- “Is there a non-anticholinergic alternative for my allergies or sleep?”
- “Could my confusion or memory issues be from my meds?”
According to a 2023 survey in the Journal of Clinical Psychiatry, 78% of psychiatrists now routinely screen for anticholinergic load-up from just 32% in 2018. That’s progress. But primary care doctors still lag behind.
What You Can Do Today
You don’t need to wait for your next appointment. Here’s what to do now:- Check every medication you take-prescription and over-the-counter. Look for diphenhydramine, hydroxyzine, chlorpheniramine, or promethazine.
- If you’re on amitriptyline, clomipramine, or imipramine, avoid any antihistamine labeled “for sleep” or “for allergies.”
- Switch to loratadine, cetirizine, or fexofenadine for allergies.
- For sleep, try melatonin or talk to your doctor about CBT-I.
- Bring your full med list to your next appointment and ask for an ACB score calculation.
There’s no reason to accept brain fog, memory loss, or urinary problems as “just part of aging.” These are red flags from your body saying: your meds are too much.
Final Thought: It’s Not About Stopping Treatment-It’s About Smarter Treatment
TCAs still have a place in treating chronic pain, depression, and some anxiety disorders. But they’re not the only option-and antihistamines are not harmless sleep aids. The goal isn’t to eliminate treatment. It’s to eliminate unnecessary risk.Medication safety isn’t about fear. It’s about awareness. And awareness saves lives.
Can I take Benadryl with amitriptyline?
No. Taking diphenhydramine (Benadryl) with amitriptyline significantly increases your risk of anticholinergic overload. This combination can cause confusion, memory loss, urinary retention, fast heartbeat, and even delirium-especially in people over 65. Even short-term use can be dangerous. Switch to a non-sedating antihistamine like loratadine (Claritin) or cetirizine (Zyrtec) instead.
What are the signs of anticholinergic toxicity?
Signs include sudden confusion or disorientation, memory problems, dry mouth, blurred vision, constipation, trouble urinating, fast heartbeat, dizziness when standing, and extreme drowsiness. If you notice any of these while taking a TCA and an antihistamine, stop the antihistamine and contact your doctor immediately. These symptoms can escalate quickly and may require emergency care.
Are all antihistamines dangerous with TCAs?
No. Only first-generation antihistamines like diphenhydramine, hydroxyzine, and chlorpheniramine have strong anticholinergic effects. Second-generation antihistamines-loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra)-have minimal to no anticholinergic activity. They’re safe alternatives for allergies and won’t interfere with your TCA.
Can anticholinergic overload cause dementia?
Yes. Multiple studies, including a 2015 JAMA Internal Medicine study, show that long-term use of medications with high anticholinergic burden-including TCAs and first-gen antihistamines-is linked to a 54% increased risk of dementia. The more drugs you take that block acetylcholine, and the longer you take them, the higher the risk. Stopping these meds can improve cognitive function over time.
What should I do if I’m on both a TCA and an antihistamine?
Don’t stop your TCA without talking to your doctor. But do stop the antihistamine immediately and replace it with a safer alternative like loratadine or cetirizine. Schedule a medication review with your doctor or pharmacist. Ask them to calculate your total anticholinergic burden using the ACB scale. Many hospitals now flag these combinations automatically-your doctor should know this risk.


Lawrence Jung
People keep treating meds like candy like if you take one little pill it won't matter
Then you wake up confused not remembering your grandkids name and wonder why
Its not magic its chemistry and your brain is drowning in blocked signals
Stop blaming doctors when you dont ask the right questions
Prachi Chauhan
in india we use diphenhydramine for everything cold sleep anxiety even headaches
no one checks acb score because no one even knows what it means
grandma takes it with her pain pills and says her mind feels clearer
but she forgets where she put the tea kettle every 10 minutes
we dont have the luxury of asking for alternatives
its either this or nothing
Katherine Carlock
I just had my dad’s med review last week and we found he was on amitriptyline + Benadryl for sleep
He’d been having memory lapses and we thought it was aging
Turns out his ACB score was 5
Switched him to melatonin and loratadine
Two weeks later he remembered my mom’s birthday for the first time in a year
Its scary how simple the fix was
Why isn’t this standard practice everywhere
Lelia Battle
The scientific evidence is clear and well-documented.
Yet the cultural normalization of over-the-counter anticholinergics persists without critical evaluation.
Many patients assume that because a drug is available without a prescription, it is inherently safe.
This misconception is reinforced by marketing, convenience, and a lack of patient education.
Healthcare systems must prioritize cognitive burden screening as part of routine geriatric assessments.
It is not merely a pharmacological issue-it is an ethical one.
Patients deserve to be informed, not just prescribed.
Compliance is not the problem-awareness is.
Rinky Tandon
you people are freaking out over a little drowsiness
my aunt took benadryl with amitriptyline for 12 years and she’s still alive
you think your brain is special
maybe you just need to stop being so sensitive
and stop blaming doctors for your own laziness
if you dont want to be sleepy then dont take the meds
but dont make a whole post about it like its a conspiracy
youre all overreacting
and yes i know what acb means i studied it in med school
but not everyone has your privilege to have 3 specialists
Ben Kono
my grandma took benadryl with her pain meds and she stopped forgetting her name
so maybe its not so bad
and why do you always blame doctors
theyre just trying to help
you want a perfect solution but life isnt perfect
if you dont like it dont take it
but dont make everyone feel guilty for trying to sleep
Cecelia Alta
Okay so let me get this straight
You're telling me that every single grandma who takes Benadryl for sleep and amitriptyline for pain is just one step away from dementia
And that the entire medical establishment is just sitting on their hands while old people turn into zombies
But somehow the solution is just to swap one pill for another and everything magically fixes itself
And no one ever asks why the hell we're prescribing two anticholinergics in the first place
Oh wait we do know why
Because sleep is hard
And pain is real
And insurance won't pay for CBT-I
And no one has time to teach patients how to use melatonin properly
So yeah sure let's all panic about the ACB score
But while we're at it let's also fix the broken healthcare system that made this a problem in the first place
Otherwise you're just doing performative medicine while real people suffer in silence
And yes I know the studies
But you don't get to reduce human suffering to a risk percentage and call it a day
It's not just about pharmacology
It's about access
It's about time
It's about dignity
And until we fix those things
People will keep taking Benadryl
Because they have no other choice
Audu ikhlas
you americans think you own medicine
in nigeria we dont even have amitriptyline in half the clinics
so you worry about anticholinergic overload
we worry about if the pills are real
or if the pharmacy has any left
you have acb scales and electronic alerts
we have a nurse who says take the white one and pray
stop lecturing us about your perfect meds
you dont know what real healthcare looks like
and your privilege is showing
and btw benadryl is cheap and works
your brain fog is your problem not ours
Sonal Guha
Stop the antihistamine immediately
Replace with loratadine
Call your doctor
ACB score
Done