Hypercalcemia Risk Calculator
Calculate Your Risk
This tool helps determine your risk of hypercalcemia when taking vitamin D supplements with thiazide diuretics. Based on your inputs, it will show whether your current dosage is safe or if you should adjust your vitamin D intake.
Many people take vitamin D supplements to support bone health, immune function, or just because they’ve heard it’s good for them. At the same time, millions are prescribed thiazide diuretics to manage high blood pressure. What happens when these two overlap? The answer isn’t obvious - but the risk is real. When vitamin D and thiazide diuretics are taken together, they can push calcium levels in your blood too high, leading to hypercalcemia. This isn’t a rare side effect. It’s a well-documented, preventable problem that’s quietly affecting older adults, especially those on long-term therapy.
How Vitamin D and Thiazides Work Together - and Why That’s Dangerous
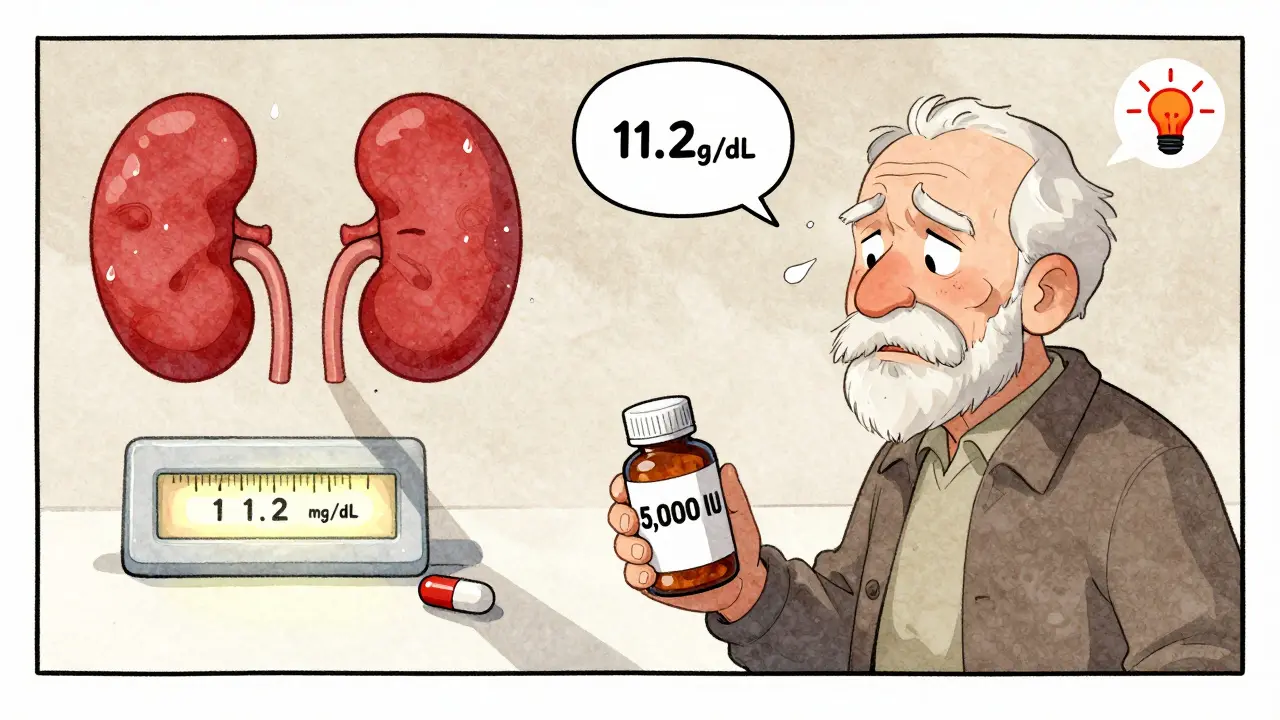
Vitamin D doesn’t just help your body absorb calcium from food. Its active form, calcitriol, turns on genes that make your intestines pull in more calcium - sometimes by 30% to 80%, depending on the dose. If you’re taking 5,000 IU or more daily, that’s a big boost. Meanwhile, thiazide diuretics like hydrochlorothiazide (Microzide) or chlorthalidone don’t just make you pee more. They actually cause your kidneys to hold onto calcium instead of flushing it out. Studies show they reduce urinary calcium loss by 30-40%. That’s why they’re sometimes used to treat kidney stones - less calcium in urine means fewer stones. Put them together, and you’ve got a double hit: your gut is soaking up more calcium, and your kidneys are saving every bit of it. The result? Calcium builds up in your blood. Normal levels are 8.5 to 10.2 mg/dL. Hypercalcemia kicks in above 10.5 mg/dL. At 11 mg/dL or higher, symptoms become noticeable - fatigue, nausea, confusion, constipation, frequent urination, even kidney damage.Who’s at Highest Risk?
This isn’t a problem for everyone. But certain groups are much more vulnerable:- People over 65 - older kidneys don’t handle calcium as well, and many take both vitamin D and thiazides.
- Those taking high-dose vitamin D (4,000 IU or more daily) - especially without medical supervision.
- Patients already with borderline high calcium (10.2-10.5 mg/dL) - even a small push can tip them over.
- People on higher doses of thiazides (25 mg hydrochlorothiazide or more).
What’s the Real-World Impact?
This isn’t just a lab number issue. Real people end up in the ER. A 2022 national survey found that 15% of all emergency visits for drug-induced hypercalcemia involved thiazide and vitamin D together. One nurse practitioner on Reddit shared that in six months, she had three patients with calcium levels above 11 mg/dL - all on 5,000 IU of vitamin D3 and hydrochlorothiazide. All three needed hospitalization. On Drugs.com, 32% of negative reviews for hydrochlorothiazide mention calcium-related problems. And a 2022 survey by the National Council on Aging found that 61% of seniors taking thiazides didn’t even know they should be checking their calcium levels when on vitamin D. That’s a gap in care - and it’s dangerous.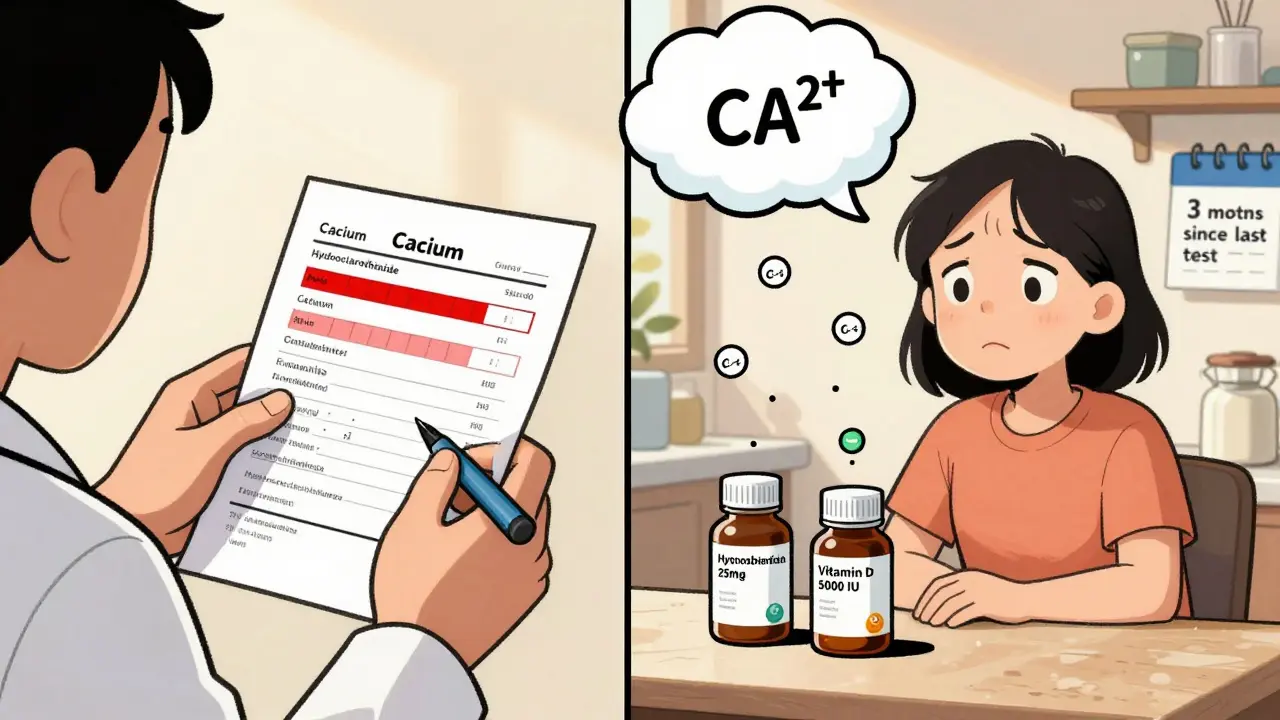
Not All Diuretics Are the Same
If you’re on a diuretic and need vitamin D, the type matters. Loop diuretics like furosemide (Lasix) do the opposite - they make you lose calcium. So if you’re at risk, switching from a thiazide to a loop diuretic might be safer. Potassium-sparing diuretics like spironolactone don’t affect calcium much either. But here’s the catch: thiazides are still the go-to for most doctors. Why? They control blood pressure better over 24 hours than other diuretics. The SPRINT trial showed they’re more effective at lowering long-term cardiovascular risk. So many doctors stick with them - even knowing the risk.How to Stay Safe
The good news? This risk is manageable. You don’t have to stop either medication. You just need to be smart about it.- Test your calcium levels before starting vitamin D if you’re on a thiazide. Then again at 3 months, and every 6-12 months after that.
- Keep vitamin D at 800-1,000 IU daily - that’s enough for most people to maintain healthy levels without pushing calcium too high. The Endocrine Society recommends this range for patients on thiazides.
- Avoid high-dose supplements unless prescribed. 5,000 IU, 10,000 IU, or 50,000 IU capsules are not necessary for most people and significantly raise risk.
- Ask about lower-dose thiazides. Switching from 25 mg to 12.5 mg hydrochlorothiazide cuts calcium retention in half, according to clinical studies.
- Watch for symptoms: unusual tiredness, dry mouth, constipation, frequent urination, or confusion. Don’t brush them off as "just getting older."
What Experts Are Saying
There’s disagreement among doctors - but the trend is clear. Dr. Murray Epstein argues the risk is overstated, citing low incidence in monitored patients. But Dr. John Burnett from Mayo Clinic calls this one of the most underrecognized causes of iatrogenic hypercalcemia in the elderly. The European Society of Cardiology says: don’t exceed 2,000 IU/day of vitamin D if you’re on a thiazide. The American Geriatrics Society Beers Criteria outright lists this combo as potentially inappropriate for older adults with calcium already above 10.2 mg/dL. The bottom line? The science isn’t split. The data shows a clear, measurable risk. The question is whether doctors and patients are paying attention.What’s Changing Now?
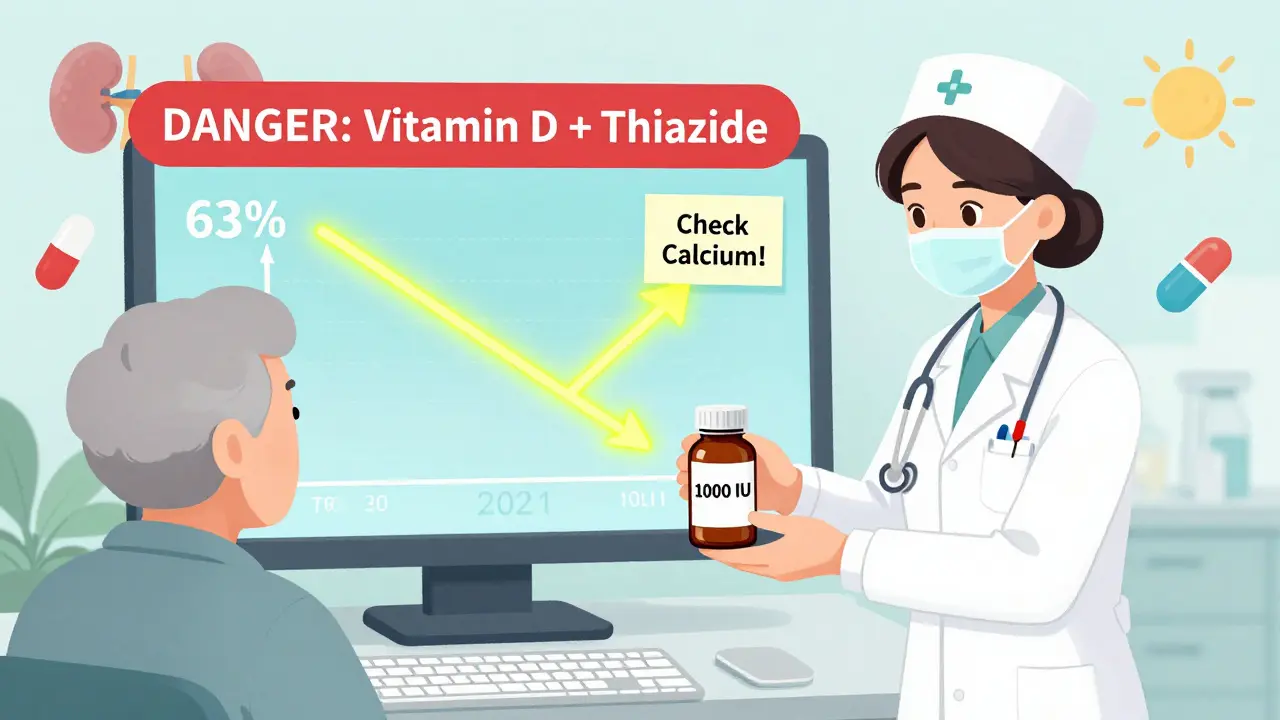
Health systems are catching on. Kaiser Permanente now has electronic alerts that pop up in doctors’ systems when someone on a thiazide tries to order vitamin D over 2,000 IU. Since implementing this in 2021, they cut inappropriate combinations by 63%. A new FDA-approved test called CalcCheck, launched in 2023, can predict individual risk based on genetic variants in the calcium-sensing receptor gene. It’s not routine yet - but it’s coming. The 2024 American Heart Association guidelines, expected this month, are likely to tighten recommendations around monitoring. And new diuretics like metolazone may offer a safer alternative - they reduce calcium reabsorption less than traditional thiazides.What You Can Do Today
If you’re taking a thiazide diuretic and a vitamin D supplement:- Check your supplement bottle. Is it more than 1,000 IU per day? Consider cutting back.
- Call your doctor. Ask if your calcium level has been checked in the last year. If not, request a basic metabolic panel.
- If you’re over 65, ask if a lower-dose thiazide (12.5 mg) could work for you.
- Don’t stop your medication. But do get the facts.
Can I still take vitamin D if I’m on a thiazide diuretic?
Yes - but only at low doses. For most people on thiazide diuretics, 800-1,000 IU of vitamin D per day is safe and sufficient. Higher doses (4,000 IU or more) significantly increase the risk of hypercalcemia. Always check your calcium levels before and during supplementation.
What are the signs of hypercalcemia from this interaction?
Symptoms include extreme fatigue, nausea, vomiting, constipation, increased thirst and urination, confusion, and muscle weakness. In severe cases, it can lead to kidney stones or heart rhythm problems. Many people mistake these for normal aging - but they’re warning signs.
How often should calcium levels be checked?
Baseline testing should happen before starting vitamin D. Then repeat at 3 months, and every 6-12 months after that if you’re on both medications. More frequent checks are needed if you have kidney disease, are over 70, or take high-dose vitamin D.
Are there safer alternatives to thiazide diuretics?
Yes. Loop diuretics like furosemide and potassium-sparing diuretics like spironolactone don’t reduce calcium excretion like thiazides do. If you’re at risk for hypercalcemia, your doctor may consider switching - especially if your blood pressure is well-controlled on a lower dose. Chlorthalidone has a stronger calcium-sparing effect than hydrochlorothiazide, so it’s not always a safer choice.
Is this interaction only a problem for older adults?
No - but it’s most common and dangerous in older adults. People over 65 are more likely to take both medications, have reduced kidney function, and absorb more calcium from supplements. However, younger patients on high-dose vitamin D and thiazides can also develop hypercalcemia - it’s just less frequent.
Can I get enough vitamin D from sunlight instead of supplements?
Yes - for many people, 10-20 minutes of midday sun exposure on arms and legs 2-3 times a week is enough to maintain healthy vitamin D levels without supplements. In places like Perth, Australia, with strong sunlight, supplementation is often unnecessary unless you have a diagnosed deficiency or limited sun exposure.
Should I stop taking vitamin D if I’m on a thiazide?
No - unless your calcium levels are already high. Stopping vitamin D can lead to bone loss and increased fracture risk. Instead, reduce the dose to 800-1,000 IU daily and get your calcium checked regularly. The goal is balance, not avoidance.



Angel Tiestos lopez
bro i took 5k IU of D3 with my hctz for 6 months and felt like a zombie 😴... thought i was just aging, but my doc finally checked my calcium and it was 11.8... now i’m at 1000 IU and life’s back to normal. thanks for this post, i thought i was the only one 😅
Pankaj Singh
This is why most Americans are dumb. You take random supplements like candy and wonder why you’re sick. Thiazides + high-dose D3? That’s not a side effect, that’s stupidity. Get your lab work done or stop being a walking pharmacology experiment.
Scottie Baker
I had a patient last week with calcium at 12.1. 5000 IU D3 + 25mg HCTZ. She thought she was ‘boosting immunity’. Her family said she’d been ‘off’ for months. ER visit, IV fluids, hospital stay. This isn’t theoretical. It’s happening every damn day. Stop the hype. Your ‘wellness routine’ is killing you.
Angel Molano
Stop taking vitamin D unless prescribed. Period. You don’t need it. Sunlight exists. Stop being lazy and stop poisoning yourself.
John Tran
I mean… think about it on a metaphysical level, right? Vitamin D is the sunshine hormone, the soul’s vitamin… and thiazides? They’re the system’s silent enforcers, pulling water out like a bureaucratic drain on the body’s divine equilibrium. So when you stack ‘em? You’re not just altering calcium levels-you’re disrupting the cosmic balance between absorption and release. The body’s not dumb. It’s screaming. But we’ve normalized silence. We’ve normalized ‘just getting older’. But what if ‘older’ is just what happens when we ignore the whispers before they become screams? 🤔💧
Milla Masliy
This is such an important post. I’m a nurse and I’ve seen this exact scenario play out too many times. Patients are told to ‘take a vitamin’ and never told to get labs. We need better education-not just for patients, but for primary care docs too. I’ve started printing out a simple one-pager for anyone on thiazides who asks about D. Small change, big impact.
Avneet Singh
The pharmacokinetic interplay between CYP2R1-mediated hydroxylation and TRPV6-mediated intestinal calcium transport under thiazide-induced renal calcium conservation presents a clinically significant iatrogenic cascade. Most clinicians lack the nuance to contextualize this within geriatric polypharmacy paradigms. The data is robust, yet implementation remains fragmented due to systemic under-resourcing.
Nelly Oruko
I appreciate this. I'm 68, on 12.5mg HCTZ, and took 2000 IU D3 for years. My calcium was 10.4. Doctor said 'it's fine.' I got a second opinion. They lowered my dose to 800 IU. Calcium is now 9.8. Never assume 'normal' is safe. Always ask for the numbers.
vishnu priyanka
in india, everyone’s on some kind of vitamin D pill like it’s chai. and doctors just prescribe HCTZ like candy. no one checks calcium. my uncle ended up in ICU last year with this exact combo. he thought he was ‘healthy’. reality check: your grandma’s supplement shelf is a silent killer.
Anny Kaettano
To anyone reading this: you are not alone. I was terrified when my calcium spiked, but my doctor helped me adjust. You don’t have to quit D3 or your blood pressure med-you just need to be informed. Let’s normalize asking questions. Let’s normalize checking labs. You deserve to feel your best, not just ‘not dead’.
Trevor Davis
I’ve been on HCTZ for 15 years and took 5000 IU D3 for 3 years. I never felt anything. My calcium was normal. So maybe this isn’t a universal problem? Just saying. Not everyone gets hit by this. Maybe it’s genetic? Or maybe the fear is being blown out of proportion?
Lance Nickie
LOL so now vitamin D is evil? Next they’ll say sunlight causes cancer. I take 10k IU and feel amazing. Your doc is scared of lawsuits, not science. This is fearmongering disguised as medicine.
sam abas
You guys are missing the real issue. The real problem is that the FDA doesn’t regulate supplement dosing. If you can buy 50,000 IU capsules over the counter like candy, that’s a regulatory failure. Not the patients. Not the doctors. The system. And until they force label limits and require calcium monitoring for high-dose D3 sales, this will keep happening. Also, typo: it’s ‘hydrochlorothiazide’ not ‘hctz’ in formal context. Just saying.
Clay .Haeber
Oh wow, another ‘concerned citizen’ who thinks their 5000 IU supplement is ‘natural’ and therefore harmless. Newsflash: ‘natural’ doesn’t mean ‘safe’. Vitamin D is a hormone, not a vitamin. You’re not ‘boosting immunity’-you’re playing Russian roulette with your kidneys. Congrats, you’re a walking biohazard.
Priyanka Kumari
This is exactly why we need community health workers to educate seniors. In my village, 8 out of 10 elderly patients on blood pressure pills take D3 without knowing why. I made a simple poster with icons: sun + pill = check calcium. Posted it at the pharmacy. 3 people came in for labs last week. Small steps, big change.