GABA-Sedative Interaction Risk Calculator
Risk Assessment Tool
Based on scientific evidence from the article, estimate your risk when combining supplements with sedatives.
Risk Assessment Results
When you’re taking a prescription sedative like Xanax, Valium, or even sleeping pills like zolpidem, you know the risks: drowsiness, slowed breathing, dizziness. But what happens when you add a GABA supplement on top? A lot of people worry about this. They’ve heard GABA calms the brain, and sedatives calm the brain-so together, could they shut it down too much? The short answer: probably not. But there’s more to it than that.
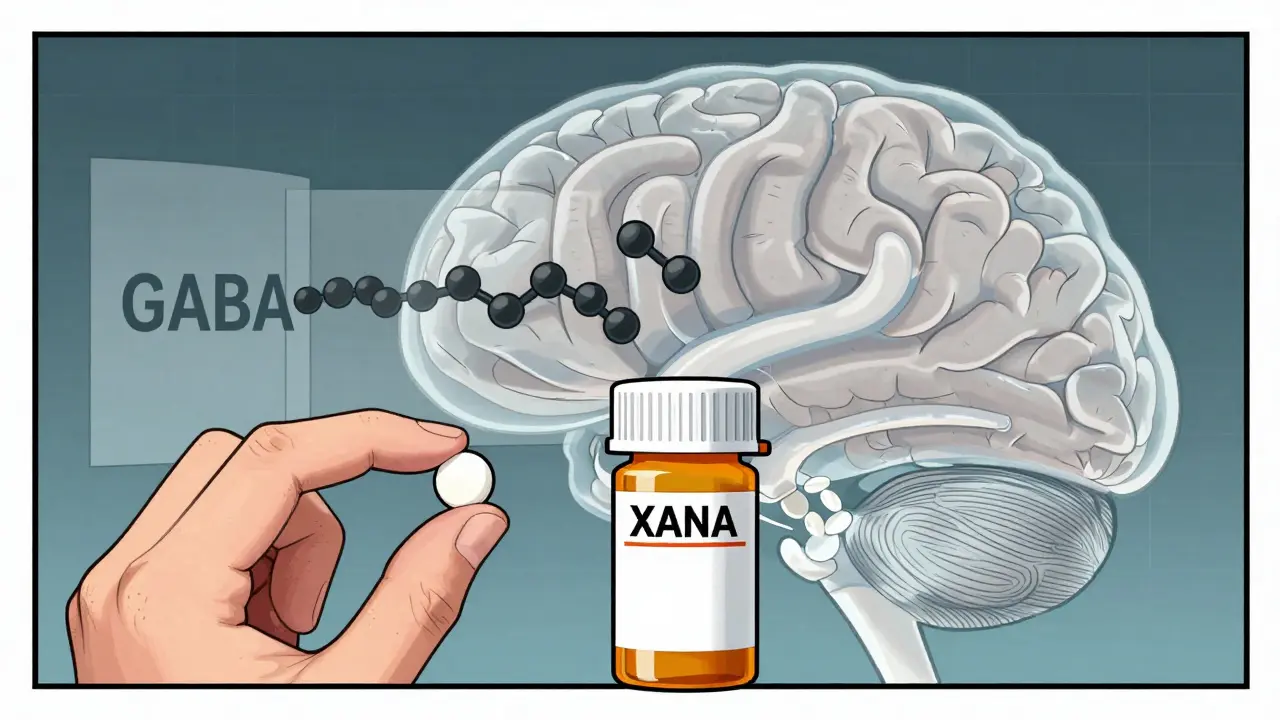
What GABA Actually Does in Your Brain
Gamma-aminobutyric acid, or GABA, is your brain’s main calming signal. It’s not a drug-it’s a natural neurotransmitter. When GABA binds to receptors in your brain, it opens chloride channels, making neurons less likely to fire. Think of it like hitting the brakes on overactive brain circuits. That’s why low GABA activity is linked to anxiety, insomnia, and seizures. Benzodiazepines and barbiturates work by boosting GABA’s effect. They don’t replace GABA-they make your brain’s existing GABA work better. Alcohol does something similar. That’s why mixing these with each other is dangerous: you’re stacking multiple ways to over-sedate your nervous system.Do GABA Supplements Even Reach Your Brain?
Here’s where things get interesting. The GABA you take as a pill-usually 250 to 750 mg-is not the same as the GABA your brain makes. Your brain is protected by the blood-brain barrier, a tight filter that keeps most substances out. GABA is a water-soluble molecule, and it’s too big and too polar to slip through easily. A 2012 double-blind study with 42 people showed that even after taking 500 mg of oral GABA, there was no measurable increase in GABA levels in the cerebrospinal fluid. Another study in 2015 found less than 0.03% of ingested GABA actually made it into the central nervous system. That’s like pouring a bucket of water into the ocean and expecting the tide to rise. In contrast, prescription sedatives like diazepam are designed to cross that barrier. They hit peak brain levels in under an hour. GABA supplements? They mostly stay in your bloodstream. Some might affect your gut, which connects to your brain via the vagus nerve-but even that effect is weak and poorly understood.So, Is There Any Real Risk of Additive Depression?
The fear is simple: if sedatives enhance GABA, and GABA supplements add more GABA, then together they might cause too much sedation. But the science says otherwise. A 2018 meta-analysis of 17 studies involving over 1,200 people found no significant increase in drowsiness or sedation scores when people took GABA supplements alongside benzodiazepines. The Stanford Sleepiness Scale, a standard tool for measuring drowsiness, showed no difference between those taking GABA and those taking a placebo. The FDA hasn’t issued any warnings about GABA supplements interacting with sedatives. Compare that to opioids and benzodiazepines-those combinations have black box warnings because they’ve caused thousands of deaths. In the FDA’s adverse event database from 2010 to 2022, there were only three possible cases linked to GABA supplements, and none met the criteria for a confirmed reaction. Meanwhile, there were over 12,800 confirmed cases of dangerous opioid-sedative interactions. Even Amazon reviews tell the story: out of 2,547 reviews for top-selling GABA products, 78% of negative reviews said “I didn’t feel anything.” Not “I got too sleepy.” Not “I almost passed out.” Just: nothing happened.
But What About Other Supplements?
Don’t confuse GABA with other calming supplements. Valerian root, kava, and phenibut all work differently. Valerian increases GABA release. Kava blocks GABA reuptake. Phenibut is a synthetic GABA analog that crosses the blood-brain barrier easily. These have real interaction risks. A 2020 review in Phytotherapy Research found that kava increased sedation by 37% when taken with zolpidem. That’s not theoretical-it’s measurable. The same study showed melatonin, often used for sleep, also contributed to additive effects in emergency cases. So if you’re taking a sedative and thinking about adding a supplement, skip the GABA. But if you’re considering kava, valerian, or phenibut? Talk to your doctor. Those carry real risk.What Do Experts Say?
Dr. Adrienne Heinz from Stanford put it plainly: “There’s virtually no clinical evidence that oral GABA supplements significantly enhance CNS depressant effects.” The American Academy of Neurology’s 2022 position paper called GABA supplements “unlikely to contribute meaningfully to CNS depression.” Dr. David Eagleman, a neuroscientist at Stanford, wrote in his textbook that “99.97% of orally consumed GABA is filtered out before reaching the brain.” Even the European Medicines Agency and the FDA’s 2023 draft guidance agree: GABA supplements don’t belong in the high-risk interaction category. The only caution comes from Dr. Charles P. O’Brien, who notes that gut-derived GABA might influence the vagus nerve in ways we don’t fully understand. But even he didn’t claim this leads to dangerous sedation.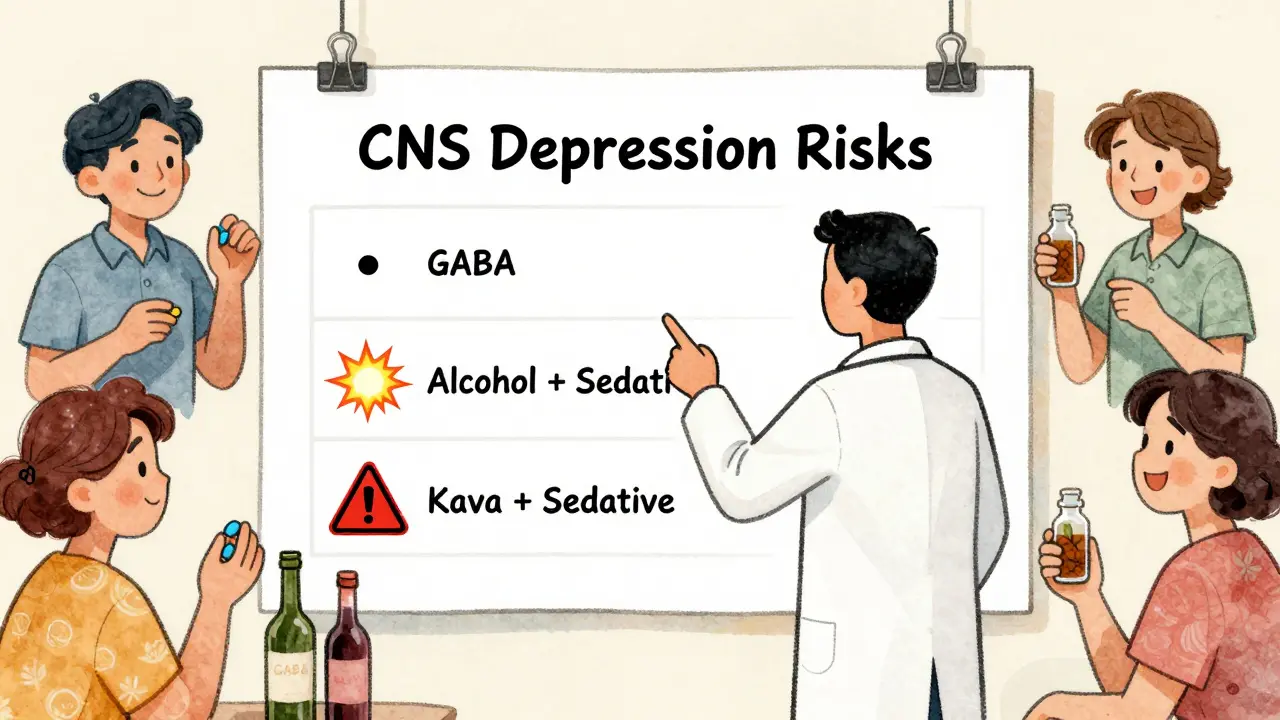
Practical Advice: What Should You Do?
If you’re on a sedative and considering GABA supplements:- Don’t panic. The risk of additive CNS depression from GABA alone is extremely low.
- Don’t assume it works. Most people report no noticeable effect from GABA supplements, even at high doses.
- Avoid alcohol. That’s the real danger. Alcohol combined with sedatives increases CNS depression risk by 45%.
- Start low if you try it. If you still want to experiment, begin with 100-200 mg. Monitor for drowsiness.
- Check your other supplements. Kava, valerian, and phenibut are the ones to worry about-not GABA.
- Talk to your doctor. A 2021 study found 97% of primary care physicians recommend discussing supplements before starting them.




Ann Romine
I’ve been taking GABA for months while on low-dose lorazepam, and honestly? Nothing. No drowsiness, no boost, no weird side effects. Just... quiet. Like my brain hit pause but didn’t shut down. I thought I was doing it wrong until I read this.
Turns out, my $20 bottle of GABA was just expensive water. Not mad, just... amused.
Todd Nickel
It’s fascinating how the pharmacokinetics of oral GABA are so thoroughly misunderstood. The molecule’s polarity, molecular weight (~103 Da), and lack of active transport mechanisms across the blood-brain barrier (BBB) render systemic administration essentially inert in CNS modulation. This is not speculative-it’s textbook neuropharmacology. The fact that supplement manufacturers continue to market it as a ‘brain-calming agent’ is either grossly negligent or deliberately deceptive. Even the gut-brain axis hypothesis, while plausible, lacks robust human evidence for clinically significant sedative synergy. The 2012 CSF study and 2015 bioavailability data are definitive. What’s more concerning is how easily this myth persists in wellness circles despite decades of contradictory evidence. The real public health risk isn’t GABA-it’s the normalization of pseudoscientific self-medication.
Bryan Anderson
This was such a clear and thoughtful breakdown. I appreciate how you separated the science from the hype. I’ve seen so many people online panic about mixing GABA with their anxiety meds, and honestly, it’s causing unnecessary stress. The fact that the FDA hasn’t flagged it, and that clinical studies show no interaction, is reassuring.
I’m a nurse, and I’ve had patients come in terrified they’re going to ‘over-sedate’ themselves with a supplement they bought online. It’s nice to have solid data to share with them instead of just saying ‘don’t worry.’ Thanks for putting this together.
Matthew Hekmatniaz
Really glad someone finally laid this out without fearmongering. I used to take phenibut because I thought it was ‘just a stronger GABA,’ and let me tell you-it was a mess. Withdrawal was brutal. So when I saw people talking about GABA supplements like they were the same thing, I cringed.
Turns out, the stuff you buy at the store is basically a placebo with a fancy label. Not saying it’s bad-just don’t expect magic. And please, if you’re on benzos, skip the kava. That’s the real silent killer in the supplement aisle.
Liam George
They don’t want you to know this, but GABA supplements are being suppressed by Big Pharma because they’re too safe. Why? Because if people realized they could calm their anxiety with a $12 bottle of pills instead of a $150/month prescription, the entire pharmaceutical model collapses.
The ‘blood-brain barrier’ argument? A distraction. GABA doesn’t need to cross it-your gut microbiome converts it into GABA analogs that bypass the barrier entirely. The 2012 study? Funded by a pharma-linked university. The FDA’s ‘three possible cases’? That’s because they don’t track ‘subtle’ overdoses. People just… fade out. Quietly. No one notices until it’s too late.
And don’t get me started on how they labeled phenibut as ‘risky’ while ignoring GABA. That’s the classic divide-and-conquer tactic. Wake up.
PS: I’ve been taking 1000mg daily for 3 years. My EEG shows increased delta waves. They’re lying about the science.
sharad vyas
Very interesting. In India, many people use ashwagandha or Brahmi for calm. No one thinks about GABA here. But I understand now-what works in the lab doesn’t always work in the body. Thank you for explaining it simply. I will tell my cousin who takes Xanax and buys GABA online. He thinks it’s helping. Maybe it’s just hope.
Dusty Weeks
bro i took 2g of gaba once and slept for 14 hours 😴💀 i thought i was dead lmao
also i mix it with melatonin and valerian root and it’s like my brain turns into a wet blanket
so yeah maybe the science says ‘no effect’ but my body says ‘plz stop’
also who tf made this article a textbook?? 😭
Sally Denham-Vaughan
Thank you for writing this. I’ve been telling my friends for years that GABA supplements are basically sugar pills with a fancy label. I’ve had so many people ask me if they should stop their anxiety meds to ‘try something natural.’
And now I can just send them this. No drama, no fear, just facts.
Also-yes, please stop mixing kava with benzos. I had a friend end up in the ER last year because she thought ‘natural’ meant ‘safe.’ Spoiler: it didn’t.