Colitis Biomarkers: What They Are and How They Guide Treatment
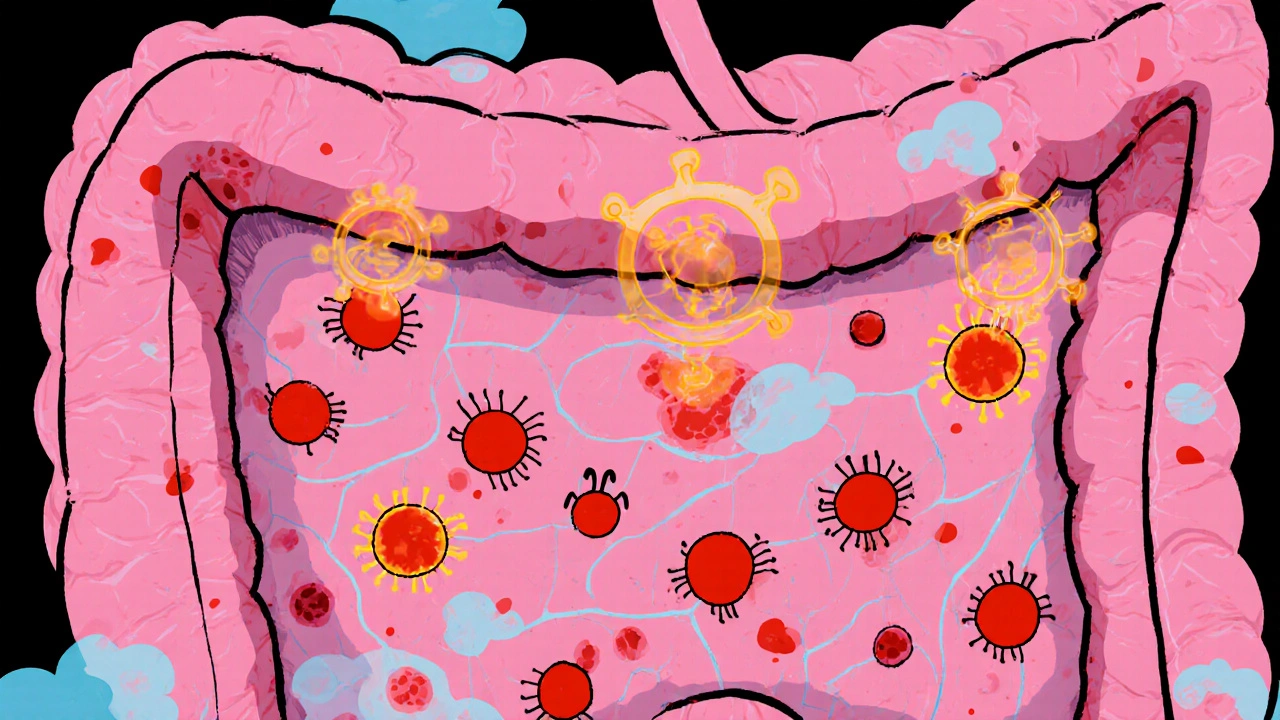
When you have colitis biomarkers, measurable biological indicators that signal inflammation or damage in the colon. Also known as inflammatory bowel disease markers, they help doctors tell if your symptoms are from ulcerative colitis, Crohn’s disease, or something else entirely. These aren’t guesses—they’re lab results backed by real data from blood, stool, or tissue samples.
One of the most common fecal calprotectin, a protein released by white blood cells during gut inflammation tells you if there’s active inflammation in your intestines. High levels mean your colitis is flaring. Low levels suggest remission—or that your symptoms might be from IBS, not colitis. Then there’s C-reactive protein, a liver-made marker that rises with systemic inflammation, often checked alongside calprotectin. Blood tests for erythrocyte sedimentation rate (ESR), another inflammation indicator give doctors a broader picture. None of these alone can diagnose colitis, but together they cut through the noise.
What’s powerful about these biomarkers is how they change treatment. If your calprotectin stays high after starting a new drug, your doctor knows it’s not working—not just because you still feel bad, but because the numbers prove it. That means less trial and error, fewer unnecessary colonoscopies, and faster adjustments. Some newer biomarkers, like anti-Saccharomyces cerevisiae antibodies (ASCA) or perinuclear antineutrophil cytoplasmic antibodies (pANCA), help distinguish between Crohn’s and ulcerative colitis early on, which changes everything about your long-term plan.
You won’t find every biomarker in every clinic yet. But the ones used today—calprotectin, CRP, ESR—are becoming standard. And research is pushing forward. Studies now look at gut microbiome patterns, genetic markers, and even stool RNA profiles to predict flares before symptoms start. These aren’t science fiction—they’re the next wave of personalized care.
What you’ll find in the posts below isn’t just theory. It’s real-world comparisons: how drugs like lurasidone affect gut-brain links, how guaifenesin might ease IBS-like colitis symptoms, and how biomarkers tie into broader gut health research. You’ll see how testing connects to treatment, and why knowing your numbers matters more than ever.