DOACs and rifampin: What You Need to Know About This Dangerous Interaction
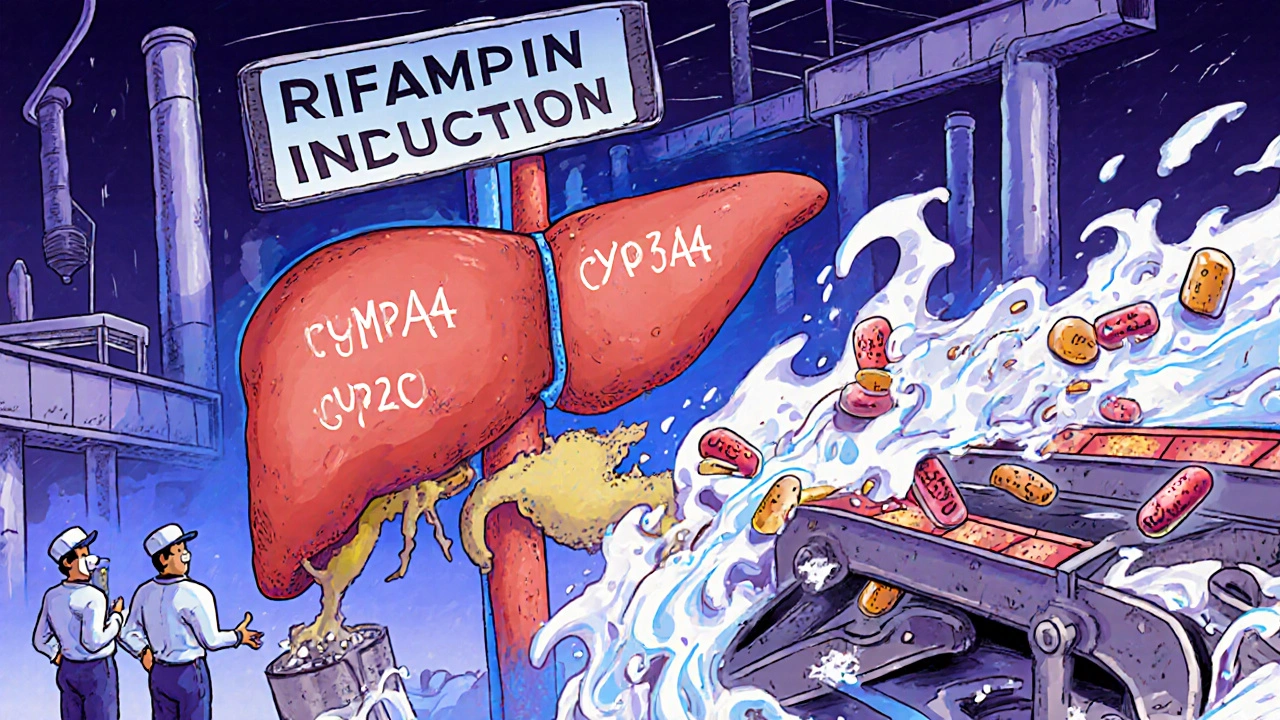
When you take DOACs, direct oral anticoagulants like apixaban, rivaroxaban, dabigatran, or edoxaban used to prevent strokes and blood clots. Also known as non-vitamin K oral anticoagulants, these drugs work differently than warfarin—but they’re just as sensitive to what else you’re taking. Now add rifampin, a powerful antibiotic used to treat tuberculosis and other serious infections. This combo can turn a life-saving medication into a dangerous gamble. Rifampin doesn’t just kill bacteria—it flips on your liver’s drug-processing system, forcing it to break down DOACs way too fast. The result? Your blood thinners vanish from your system before they can do their job. Suddenly, you’re at risk for clots, strokes, or pulmonary embolisms—even if you took your pill on time.
This isn’t theoretical. A 2020 study in the Journal of the American College of Cardiology tracked patients on rivaroxaban who started rifampin. Within days, their drug levels dropped by over 70%. One patient had a stroke. Another needed emergency surgery for a blood clot. These aren’t rare cases. They’re predictable. And they’re preventable—if you know to ask. The same thing happens with dabigatran and apixaban. Even edoxaban, the one often thought to be more stable, isn’t safe with rifampin. The FDA and European Medicines Agency both warn against this mix. No exceptions. No "just a short course." If you’re on a DOAC and your doctor prescribes rifampin, you need a new plan—right away.
What do you do instead? If you need antibiotics, talk to your doctor about alternatives that don’t interfere. Doxycycline, amoxicillin, or azithromycin might work depending on your infection. If rifampin is your only option—maybe you have TB or a stubborn staph infection—your doctor might switch you back to warfarin, which can be monitored with blood tests. Or they might adjust your DOAC dose, but only under strict supervision. Never change your meds on your own. And if you’re already on both, watch for signs: sudden dizziness, chest pain, swelling in one leg, trouble breathing. These aren’t just side effects—they’re red flags.
Below, you’ll find real-world stories and detailed comparisons from patients and doctors who’ve dealt with this exact problem. Some switched drugs. Others got lucky with timing. A few didn’t make it. This isn’t just about pharmacology. It’s about survival. Let’s look at what actually works—and what almost kills.