Gene-Based Drug Selection: How Your DNA Shapes Your Medication Choices
When you take a pill, your body doesn’t just react the same way everyone else does. Gene-based drug selection, the practice of matching medications to a person’s genetic makeup to improve effectiveness and reduce harm. Also known as pharmacogenomics, it’s not science fiction—it’s happening in clinics right now. Two people can take the same antidepressant, but one feels better while the other gets nauseous or dizzy. Why? It’s not about willpower or lifestyle. It’s often about a single gene variation that changes how fast your liver breaks down the drug.
This isn’t just about side effects. Pharmacogenomics, the study of how genes influence drug response explains why some people need twice the dose of a blood thinner to work, while others bleed dangerously on a standard dose. It’s why statins cause muscle pain in some but not others. And it’s why a child with asthma might react badly to a generic version of their inhaler—their genes process the active ingredient differently than an adult’s. Genetic drug response, the way your DNA determines how a drug affects you isn’t optional anymore. It’s the difference between treatment that works and treatment that puts you at risk.
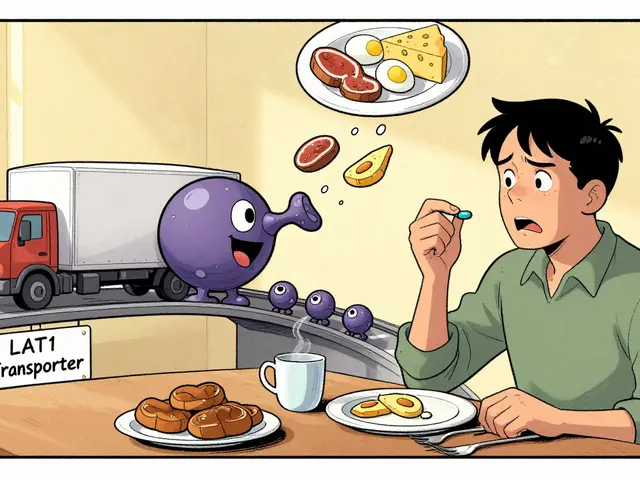
Doctors aren’t guessing anymore. Blood tests and saliva kits are now used to check for key gene variants like CYP2D6, CYP2C19, and SLCO1B1—genes that control how your body handles everything from painkillers to cholesterol meds. If you’re on warfarin, SSRIs, or even certain cancer drugs, your genes might already be guiding your dose. This isn’t just for rare diseases. It’s for common conditions: depression, heart disease, asthma, arthritis. The more you know about your genetic profile, the less trial and error you’ll face.
And it’s not just about picking the right drug. It’s about avoiding the wrong one. Some people carry a gene variant that makes them ultra-sensitive to codeine—turning a simple painkiller into a life-threatening opioid. Others can’t activate clopidogrel, the blood thinner, at all. Without testing, they’re left vulnerable to heart attacks. This is why gene-based drug selection isn’t a luxury. It’s a safety net.
Below, you’ll find real stories and science-backed guides showing how this works in practice. From statin muscle pain linked to genetics, to why some people can’t tolerate certain antidepressants, to how pediatric meds need special handling because of DNA differences—you’ll see exactly how your genes are already shaping your health journey. No fluff. Just what you need to know to talk to your doctor, ask the right questions, and get the right pill for your body.