Annual Medication Review: What It Is and Why It Saves Lives
When you take multiple pills every day, an annual medication review, a structured check-up of all your medications by a pharmacist or doctor to spot risks and simplify your regimen. Also known as a medication reconciliation, it’s not optional—it’s essential, especially if you’re over 65 or managing chronic conditions like diabetes, heart disease, or depression. Think of it like an oil change for your body: you don’t wait until the engine seizes to check the fluids. Yet, most people never get one unless they’re hospitalized. That’s a problem. Studies show nearly 40% of older adults are taking at least one drug that doesn’t belong in their regimen, and over 20% are on medications that interact dangerously with each other.
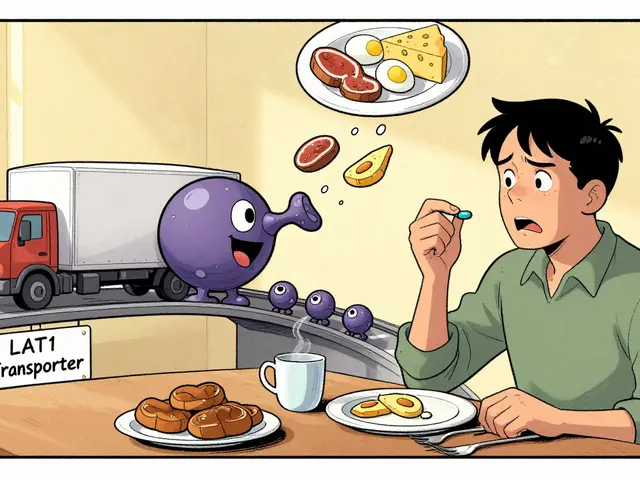
That’s where drug interactions, when two or more medications affect each other’s strength, side effects, or how your body processes them come in. Take someone on warfarin for blood thinning who starts taking rifampin for an infection—suddenly, the warfarin stops working, and the risk of stroke spikes. Or someone on statins who adds a muscle-relaxant and ends up with unexplained pain, thinking it’s just aging. These aren’t rare mistakes. They happen every day because no one sat down with all the bottles and asked: "What are you really taking, and why?" An annual medication review digs into this. It doesn’t just list pills—it asks questions like: Is this still helping? Could this be causing your dizziness? Is there a cheaper, safer option?
This isn’t just about seniors. Parents of kids on long-term asthma meds need it too. Switching generics without checking for subtle differences can trigger flare-ups. People on antidepressants, thyroid meds, or painkillers often don’t realize their anxiety or fatigue might be drug-induced, not mental. The medication management, the ongoing process of tracking, adjusting, and optimizing drug use to maximize safety and effectiveness you get during an annual review is the difference between feeling okay and feeling like yourself again. And it’s not magic—it’s method. Pharmacists use tools like the Beers Criteria for older adults, FRIDs lists for fall risks, and pharmacogenomic flags to spot who might react badly to certain drugs.
What you’ll find in the posts below isn’t theory. It’s real stories: how sedating meds increase fall risk in older adults, why generics can be risky for children, how rifampin kills anticoagulant levels, and how muscle aches from statins are often misdiagnosed. You’ll see how biologics, antihistamines, and even turmeric supplements can clash with your daily pills. Each article is a piece of the puzzle—showing you what to ask, what to watch for, and when to push back. No fluff. No sales pitches. Just what happens when you finally take control of your meds instead of letting them control you.