Combination Medications: What They Are, Why They Matter, and What to Watch For
When you take a combination medication, a single pill or liquid that contains two or more active drugs meant to work together. Also known as fixed-dose combinations, these are designed to make treatment easier—fewer pills, fewer doses, and sometimes better results. But they’re not always safer. In fact, mixing drugs in one tablet can hide risks you wouldn’t see if you took them separately. Think of Zyrtec-D or Claritin-D: they combine an antihistamine with a decongestant like pseudoephedrine to tackle both runny nose and stuffiness. Sounds convenient, right? But if you have high blood pressure or take a heart medication, that decongestant could spike your blood pressure or cause an irregular heartbeat. You might not even know you’re at risk because the label doesn’t scream "danger"—it just says "for cold and allergies."
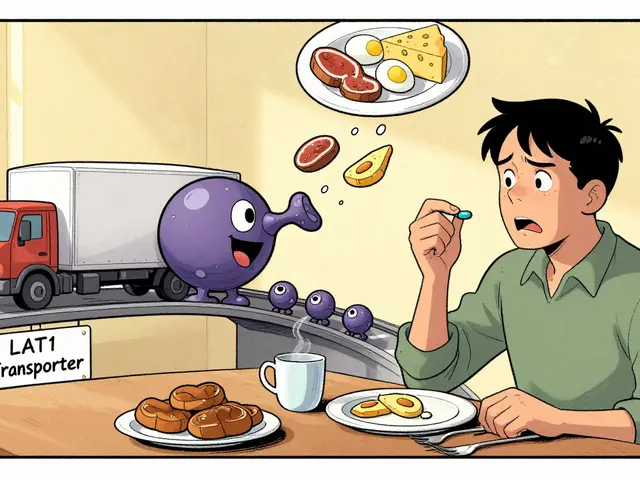
Combination medications are everywhere. They’re in pills for high blood pressure, diabetes, depression, and even acid reflux. Some are smart pairings—like metformin and SGLT2 inhibitors for diabetes, where the drugs help each other work better. Others? They’re more about convenience than care. A lot of these combos were created because drug companies could patent a new mix even if the individual drugs were old. That’s why you’ll see so many versions of the same combo, each with a slightly different name but the same ingredients. And here’s the problem: when your doctor prescribes a combo, they might not realize you’re already taking one of the ingredients alone. That’s called polypharmacy, the use of multiple medications at the same time. Also known as medication overload, it’s a silent issue in older adults and people with chronic conditions. One study found that nearly 1 in 4 seniors take five or more prescriptions—and nearly half of those include at least one combination drug. The result? More side effects, more confusion, and more trips to the ER.
Some combos are lifesavers. Others? They’re ticking time bombs. Rifampin, for example, can tank the levels of blood thinners and antivirals by speeding up how your liver breaks them down. That’s not something you’d catch if you just looked at the pill bottle—you’d need to know how the drugs interact. Same goes for statins and certain antibiotics, or antidepressants and migraine meds. These aren’t rare edge cases. They’re common, and they’re often missed because doctors don’t always check for drug interactions, when two or more medications affect each other’s effects or safety. Also known as medication interactions, they’re one of the top causes of preventable hospitalizations. The good news? You don’t have to guess. You can ask your pharmacist to run a full interaction check. You can bring every pill, capsule, and supplement to your next appointment. You can say, "Is this combo really necessary?" And you can insist on a medication review—especially if you’re over 65 or managing more than one chronic condition.
What you’ll find in the posts below isn’t a list of every combo out there. It’s a real-world look at the ones that matter—the ones that cause anxiety, raise blood pressure, mess with kidney function, or hide dangers behind simple labels. From Zyrtec-D to metformin combos, from statin mixtures to antipsychotic blends, these are the pills people take every day without knowing the full story. You’ll learn what to watch for, who’s most at risk, and how to talk to your doctor so you’re not just taking medicine—you’re managing your health.