Orphan Drug Exclusivity: What It Means for Patients and Drug Prices
When a drug gets orphan drug exclusivity, a 7-year period of market protection granted by the FDA to drugs treating rare diseases affecting fewer than 200,000 people in the U.S., it means no other company can sell a similar version for that same condition—not even if the patent has expired. This isn’t about innovation alone. It’s a legal tool designed to fix a broken market: why would a company spend millions developing a drug for a disease that affects just a few thousand people? The answer: because the government says they can charge whatever they want for seven years.
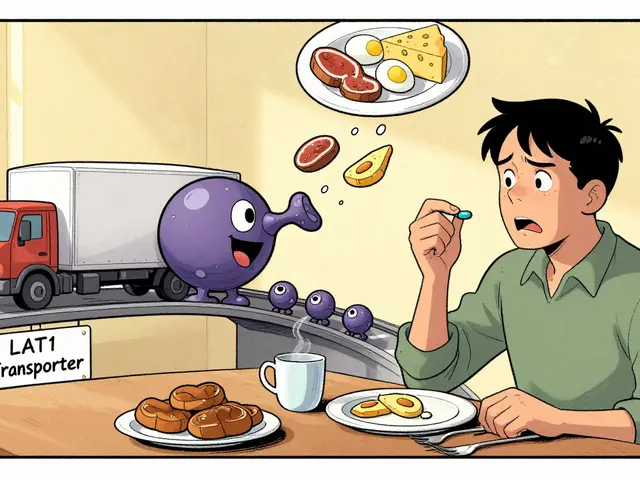
That exclusivity is separate from patents. A drug can have both, or just one. The FDA grants orphan drug designation, a status given before approval to drugs targeting rare conditions, unlocking tax credits, research grants, and fee waivers. But exclusivity kicks in only after approval. And once it’s locked in, competitors can’t enter—even if they prove their version is safer, cheaper, or works better. This has led to some shocking outcomes. A drug originally approved in the 1960s for a rare blood disorder now costs $100,000 a year—not because it’s new, but because it holds orphan exclusivity. Meanwhile, drug pricing, the cost patients and insurers pay for medications, often spikes after orphan designation due to lack of competition. Some companies even buy up older drugs, reapply for orphan status, and jack up prices overnight.
It’s not all bad. Before orphan incentives, many rare diseases had zero treatments. Today, over 600 orphan drugs are approved—up from just a handful in the 1980s. But the system is being abused. Companies sometimes split one disease into smaller subgroups just to qualify. Or they file for exclusivity on minor changes to existing drugs—like switching from a pill to a liquid. These tactics stretch the intent of the law. And patients pay the price. You won’t find these drugs on pharmacy discount cards. Insurance often denies them. Some families sell homes to afford a single month’s supply.
What you’ll find in the posts below isn’t a list of orphan drugs. It’s a collection of real-world stories about how drug rules affect people. You’ll see how orphan drug exclusivity connects to generic competition, how it plays into medication access, and why a 20-year-old pill can cost more than a new car. There’s no sugarcoating it: the system works for some, but leaves others behind. These articles don’t just explain the rules—they show you what happens when they’re pushed to the edge.