Parkinsonism: What to watch for and what you can do
Parkinsonism is a group of movement problems that look like Parkinson's disease but can come from different causes. If you or someone you care for is moving slower, shaking at rest, or losing balance, it’s worth knowing the difference — because the cause affects treatment and outlook.
How parkinsonism shows up
Symptoms often start slowly. Key signs include bradykinesia (slow movement), muscle stiffness, a resting tremor (shaking when the hand is at rest), and postural instability (trouble with balance). People also report smaller handwriting, a quieter voice, reduced facial expression, and softer steps. Not everyone has every symptom, and the mix can help a doctor figure out the cause.
Timing and pattern matter. Symptoms that start after taking certain medications — especially older antipsychotics or some anti-nausea drugs — often point to drug-induced parkinsonism. Sudden worsening, early falls, trouble looking up/down, or poor response to typical Parkinson's meds suggest an atypical form like progressive supranuclear palsy or multiple system atrophy.
Causes, tests, and what treatments look like
Common causes include:
- Idiopathic Parkinson's disease — the most familiar cause.
- Drug-induced parkinsonism — from meds like haloperidol, risperidone, or metoclopramide.
- Vascular parkinsonism — small strokes affecting movement circuits.
- Atypical parkinsonian disorders — progressive conditions with extra features.
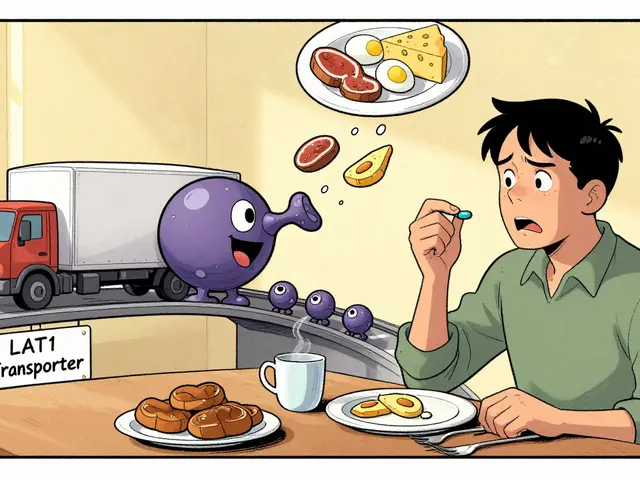
Diagnosis is mainly clinical: a doctor checks symptoms, how they progress, and whether levodopa helps. Your clinician may order brain MRI to rule out strokes or structural problems, and a dopamine transporter (DAT) scan in unclear cases. Blood tests can rule out rare mimics.
Treatment depends on the cause. If a medication is responsible, stopping or switching the drug can improve symptoms. For Parkinson's disease and some parkinsonisms, levodopa remains the most effective drug to ease movement problems. Other options include dopamine agonists, MAO-B inhibitors, and COMT inhibitors. Physical therapy, occupational therapy, speech therapy, and balance training help a lot. In selected patients with persistent symptoms, deep brain stimulation (DBS) can be an option.
Practical tips you can use now: keep a daily symptom log (time, what you notice, meds taken), ask your prescriber about any medicine that blocks dopamine, start balance and strength exercises early, and fall-proof the home (good lighting, remove rugs, grab bars). If symptoms appear quickly or include fainting, severe confusion, or swallowing problems, seek care right away.
Want more detail? Our resources cover medication guides, safe online pharmacy options, and rehab tips to help manage parkinsonism day to day. If you have questions about a specific drug or symptom, bring your notes to a neurology or movement-disorders visit — a focused exam changes treatment choices.