Medication Safety and Management in 2025: Key Insights on Generics, Aging, and Drug Interactions
When it comes to medication safety, the practice of ensuring drugs are used correctly to avoid harm while maximizing benefit. Also known as drug safety, it’s not just about taking pills as directed—it’s about understanding how your body, age, genetics, and other meds interact in ways that can make or break your health. In November 2025, the focus wasn’t on hype or trends. It was on real, daily risks: a senior falling because of a sedating antihistamine, a child’s asthma worsening after a generic switch, or someone with kidney disease taking metformin at a dangerous dose because no one checked their eGFR.
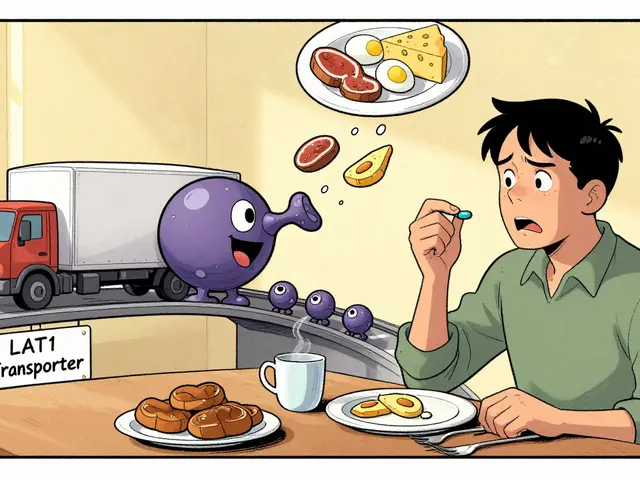
One big theme? generic drugs, lower-cost versions of brand-name medications that must meet strict bioequivalence standards. Also known as brand equivalents, they’re not always interchangeable—especially for drugs with a narrow therapeutic index, a small window between an effective dose and a toxic one. Also known as NTI drugs, these include thyroid meds, seizure drugs, and blood thinners. The FDA, EMA, and Japan all handle them differently, and skipping the right monitoring can lead to hospitalization. Then there’s aging and medication, how the body’s ability to process drugs changes after 65, increasing side effects and fall risks. Also known as geriatric pharmacology, this isn’t just about taking fewer pills—it’s about knowing which ones become dangerous over time, like benzodiazepines or anticholinergics, and how the Beers Criteria helps doctors cut the risk. And don’t forget drug interactions, when two or more medications interfere with each other’s absorption, metabolism, or effect. Also known as medication conflicts, these aren’t always obvious. Calcium blocks bisphosphonates. Decongestants spike blood pressure. Even sunscreen ingredients can mess with hormone levels if used daily. All of this ties into pharmacogenomics, how your genes affect how you respond to drugs. Also known as personalized medicine, this field is finally moving from labs into clinics, helping explain why one person gets dizzy on a low dose while another needs triple the amount.
What you’ll find in this collection isn’t theory. It’s what people are actually dealing with: a commercial driver worried about losing their CDL over a prescribed anxiety med, a parent unsure if switching their child’s ADHD drug is safe, someone with vitiligo finding real cosmetic help, or a senior preparing for their Medicare medication review. These aren’t edge cases. They’re everyday situations where the wrong pill, the wrong timing, or the wrong assumption can change everything. No fluff. No marketing. Just what you need to know to stay safe, save money, and ask the right questions.