Complex Generic Drugs: What You Need to Know About Safety, Switching, and Side Effects
When you hear complex generic drugs, generic medications that require precise dosing because even small changes can cause serious harm. Also known as narrow therapeutic index (NTI) generics, it is a category of medicines where the difference between a safe dose and a dangerous one is razor-thin. These aren’t your everyday pain relievers or antihistamines. They’re drugs like lithium, warfarin, phenytoin, and levothyroxine—medications where a 10% shift in blood levels can mean the difference between control and crisis. That’s why switching from brand to generic, or even between different generic brands, isn’t just a cost-saving move—it’s a medical decision.
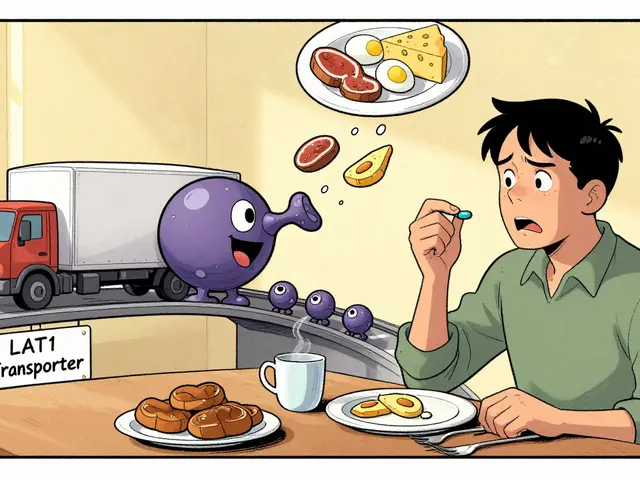
That’s where NTI generics, generic versions of drugs with a narrow therapeutic index that require stricter regulatory oversight come into play. The FDA, EMA, and other agencies treat these differently because bioequivalence isn’t enough. A generic version might meet the technical standard, but in real life, it can still cause spikes in toxicity or drops in effectiveness—especially in older adults, people with kidney issues, or those on multiple meds. Studies show that patients on NTI generics sometimes experience more hospital visits after a switch, not because the drug is bad, but because their bodies react unpredictably to slight formulation changes. And it’s not just about the pill itself—drug interactions, when one medication changes how another is absorbed, metabolized, or cleared from the body make things worse. Take lithium and ibuprofen: even a few days of a common painkiller can push lithium levels into toxic range. Or rifampin, an antibiotic that can slash anticoagulant levels by half, leaving patients unprotected from clots. These aren’t rare edge cases. They happen every day.
And then there’s the hidden layer: pharmacogenomics, how your genes affect how your body processes drugs. Two people taking the same generic drug, at the same dose, can have wildly different results because of tiny variations in their DNA. One might metabolize a drug too slowly and build up toxic levels. Another might clear it too fast and get no benefit. This isn’t science fiction—it’s why some patients do better on brand-name drugs, even when generics are cheaper. It’s why switching a child’s asthma inhaler or an elderly person’s blood thinner can trigger falls, seizures, or heart problems. The system assumes all generics are equal. But in practice, they’re not.
What you’ll find in the articles below isn’t a list of drug names. It’s a guide to the real-world risks behind the pills. You’ll learn how to spot when a generic switch might be dangerous, why some medications need lab monitoring after every change, how aging changes how your body handles these drugs, and what to ask your doctor before accepting a substitution. These aren’t theoretical concerns. They’re the reasons people end up in the ER, why seniors fall, why asthma flares up, and why some treatments fail even when they’re supposed to work. This is the quiet side of pharmacy—the part no one talks about until something goes wrong. Let’s fix that.