Drug Interactions: What You Need to Know Before Taking Multiple Medications
When you take more than one medication, drug interactions, harmful or unexpected changes in how drugs work when taken together. Also known as medication interactions, they’re not rare—they happen every day to people managing chronic conditions, aging, or multiple prescriptions. It’s not just about mixing pills. It’s about how your liver processes them, how your genes respond, and whether a simple OTC painkiller cancels out your blood pressure medicine.
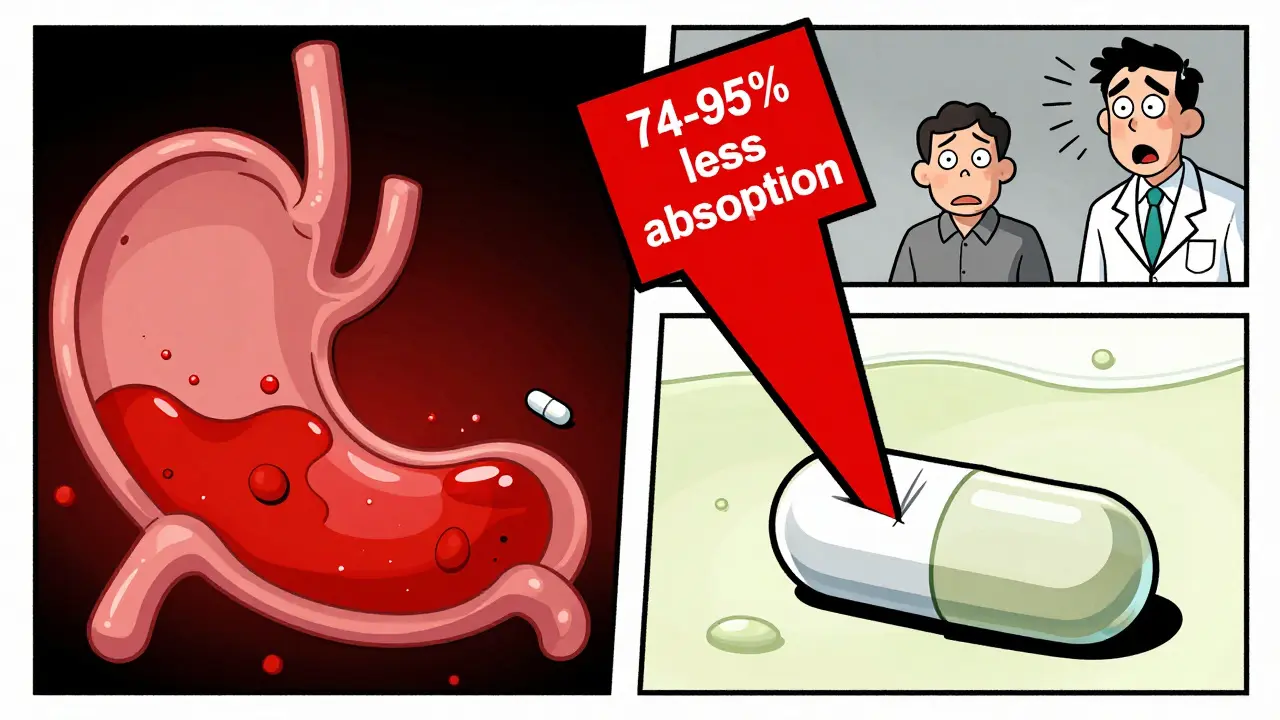
One of the biggest hidden risks is polypharmacy, taking five or more medications at once. It’s common in older adults, but it’s not inevitable. A single drug like rifampin, an antibiotic that speeds up liver enzyme activity, can slash the effectiveness of blood thinners, antivirals, and even birth control. Meanwhile, pharmacogenomics, how your genes affect how you respond to drugs, explains why one person gets sick from a dose that helps someone else. These aren’t theoretical concerns—they’re why some people end up in the ER after taking Zyrtec-D with heart meds, or why statins cause muscle pain in some but not others.
Drug interactions don’t always show up as nausea or dizziness. Sometimes they’re silent: your antidepressant stops working because of an herbal supplement, your diabetes drug becomes less effective after starting a new steroid, or your blood thinner doesn’t thin enough because of a common antacid. That’s why a Medicare medication review isn’t just paperwork—it’s a lifesaver. And it’s why knowing what’s in your pillpack matters more than you think.
Below, you’ll find real stories from people who’ve been caught off guard by these interactions—and the clear, no-fluff guides that help you avoid the same mistakes. From how decongestants raise blood pressure to why turmeric supplements can interfere with chemo, this collection cuts through the noise. You won’t find vague warnings here. Just facts, specific drugs, and what to do next.