Emergency Response: What to Do When Medication Risks Turn Critical
When a emergency response, the immediate actions taken when a medication causes life-threatening side effects. Also known as medication crisis protocol, it’s not just about calling 911—it’s about recognizing the warning signs before the situation spirals. Too many people wait until someone stops breathing or passes out before acting. But in cases like sedative overdose, a dangerous drop in breathing caused by sleeping pills or anti-anxiety drugs, every minute counts. Slow breathing, blue lips, unresponsiveness—these aren’t just side effects. They’re red flags that demand instant action. And it’s not just overdoses. Even routine meds like lithium, a mood stabilizer used for bipolar disorder that becomes toxic when kidney function drops can turn deadly if paired with common painkillers like ibuprofen. The risk isn’t theoretical—it’s documented in real cases where patients ended up in the ER because no one knew the interaction existed.
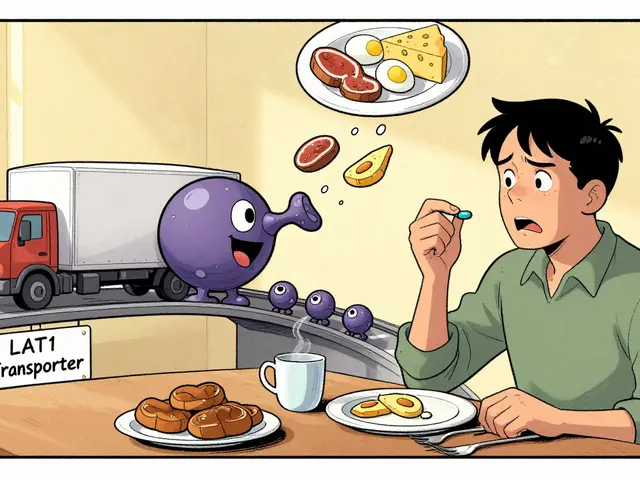
Emergency response isn’t just for accidental overdoses. It’s also for silent killers like sleep apnea, a condition where breathing stops repeatedly during sleep, silently raising blood pressure and straining the heart. People with untreated sleep apnea are far more likely to have heart attacks or strokes, yet most don’t realize their snoring is a medical emergency waiting to happen. Same with respiratory depression, the dangerous slowing of breathing that can follow sedatives, opioids, or even some allergy meds. It doesn’t always come with screaming or panic. Sometimes, it’s just a loved one who won’t wake up. That’s why knowing the signs matters more than waiting for a doctor’s appointment. And when it comes to drug interactions, when two or more medications clash in harmful ways inside the body, the danger isn’t always obvious. Lithium and NSAIDs? Deadly combo. Rifampin and blood thinners? Could cause a stroke. Even something as simple as calcium supplements can make osteoporosis meds useless if taken at the wrong time. These aren’t edge cases—they’re common mistakes that happen because people assume their meds are safe together.
You don’t need to be a pharmacist to spot trouble. You just need to know what to look for: confusion, extreme drowsiness, trouble breathing, chest pain, or sudden changes in behavior. Keep a list of every medication you or a loved one takes—including vitamins and OTC pills. Know the risks. Ask your pharmacist: "Could this cause trouble if taken with anything else?" Don’t wait for a crisis to learn the answer. The articles below give you real, actionable info on the most dangerous medication risks you might face—from recognizing an overdose before it’s too late, to understanding why some drugs are safe for some people but deadly for others. This isn’t theory. It’s what you need to know to act fast, stay safe, and maybe even save a life.