NSAID Kidney Damage: What You Need to Know Before Taking Pain Relievers
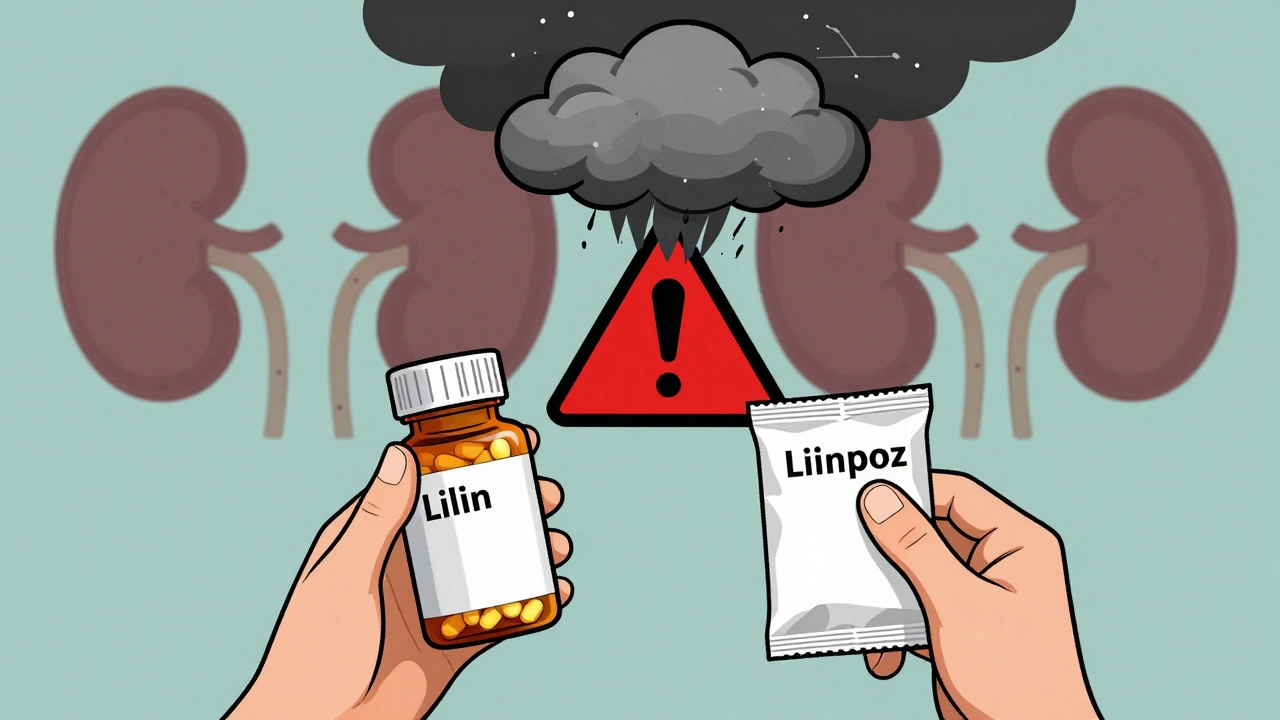
When you reach for ibuprofen or naproxen for a headache or sore back, you’re using a type of drug called a NSAID, nonsteroidal anti-inflammatory drugs that reduce pain, fever, and inflammation. Also known as non-steroidal anti-inflammatories, these are among the most commonly used medications worldwide—but they’re not harmless, especially for your kidneys. Unlike acetaminophen, which mostly affects the liver, NSAIDs work by blocking enzymes that help regulate blood flow to the kidneys. Over time, or in high doses, that can lead to real, sometimes permanent, kidney damage, a decline in kidney function that can progress to chronic kidney disease or acute kidney injury.
People with existing conditions like high blood pressure, diabetes, or heart failure are at higher risk, but even healthy adults can get hurt if they take NSAIDs daily for months or years. One study found that regular users of NSAIDs had a 20% higher chance of developing kidney problems over five years compared to non-users. The damage often builds quietly—no pain, no warning—until blood tests show your kidneys aren’t filtering waste like they should. Older adults, especially those over 65, are most vulnerable. And it’s not just prescription NSAIDs: over-the-counter pills like Advil and Aleve add up fast when taken for back pain, arthritis, or menstrual cramps.
What makes this worse is that many people don’t realize NSAIDs can interact with other meds. If you’re on blood pressure drugs like ACE inhibitors or diuretics, or have dehydration from illness or exercise, your kidneys are already under stress—and NSAIDs push them over the edge. Even a single high dose can trigger sudden kidney failure in someone with low blood volume. The renal toxicity, the harmful effect of drugs on kidney tissue isn’t always obvious, but it shows up in lab results: rising creatinine, dropping eGFR, or protein in the urine. These aren’t just numbers—they’re signs your kidneys are struggling.
You don’t have to stop taking NSAIDs entirely, but you need to know the risks and how to use them safely. If you’re taking them for chronic pain, talk to your doctor about alternatives like physical therapy, acetaminophen, or targeted injections. If you’re on daily pain meds, ask for a kidney function test. Keep track of how often you’re taking them—once a week is very different from twice a day. And never take them if you’re dehydrated, sick with vomiting or diarrhea, or already have kidney disease. The goal isn’t fear—it’s awareness. Small changes can make a big difference.
Below, you’ll find real-world insights from people who’ve dealt with kidney issues linked to pain meds, guides on safer alternatives, and clear explanations of how these drugs affect your body. Whether you’re managing arthritis, recovering from an injury, or just want to avoid silent damage, these posts give you the facts you need to protect your kidneys without giving up relief.