FDA Approval: What It Means for Your Medications and Why It Matters
When a drug gets FDA approval, the U.S. Food and Drug Administration’s official clearance that a medication is safe and effective for its intended use. Also known as drug market authorization, it’s the gatekeeper between a lab discovery and your medicine cabinet. This isn’t a formality—it’s a years-long process that checks everything from how the drug works in your body to whether it’s safer than existing options. Without it, you’d be taking pills with no proof they do what they claim—or worse, ones that could harm you.
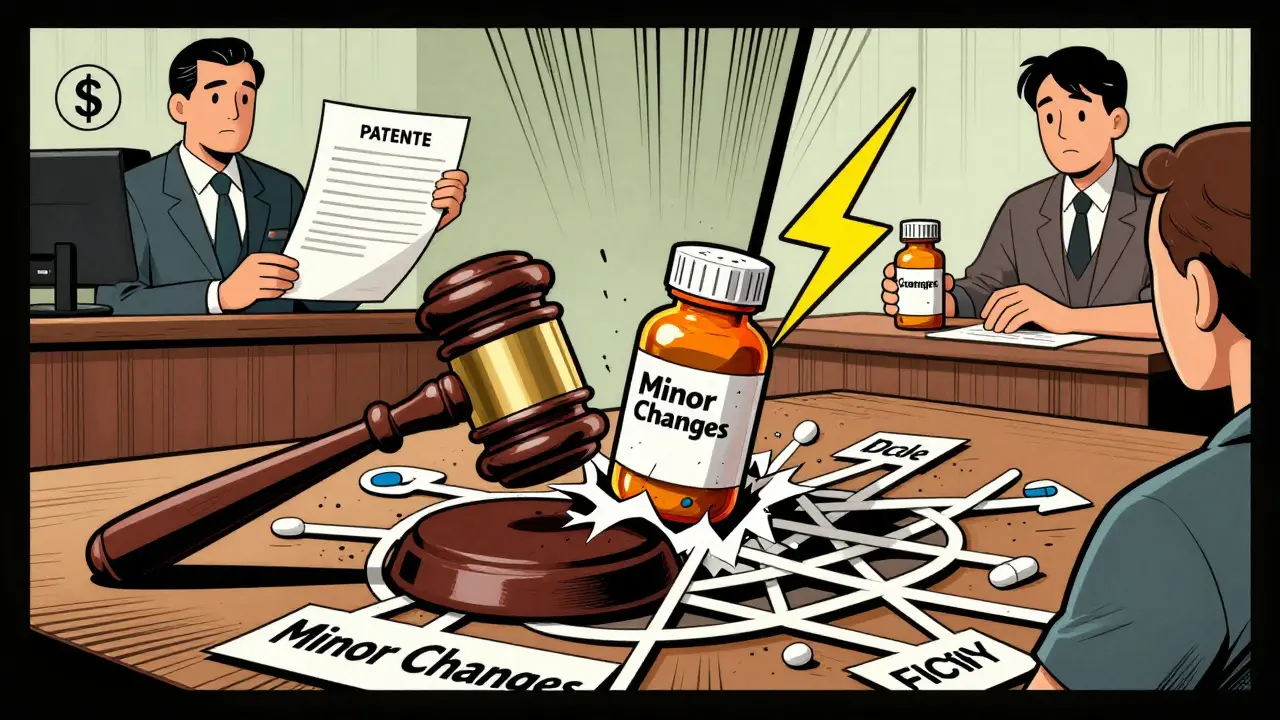
FDA approval doesn’t mean the same thing for every drug. For brand-name pills, it means years of clinical trials, thousands of patients, and strict data review. But for generic drugs, copies of brand-name medications that must meet the same safety and effectiveness standards, the process is different. Generics don’t repeat full clinical trials—they prove they deliver the same active ingredient at the same rate and strength. That’s why a generic version of metformin or betaxolol works just like the brand. But for narrow therapeutic index drugs, medications where small changes in dose can cause serious harm or treatment failure, the FDA demands even tighter controls. Drugs like lithium, warfarin, or certain antiseizure meds can’t just be swapped out. Even tiny differences in how a generic is made can throw off your treatment.
The FDA doesn’t just approve drugs—it watches them after they hit the market. If a drug causes unexpected side effects, like diphenhydramine triggering seizures or NSAIDs damaging kidneys in people on lithium, the agency can issue warnings or pull it. That’s why you’ll see safety updates on prescriptions for sleep meds, statins, or asthma inhalers. And when it comes to pharmaceutical regulation, the system of rules and oversight that ensures drugs meet quality, safety, and efficacy standards, the FDA is just one player. Countries like the EMA in Europe or Health Canada have their own rules, which is why a drug approved in the U.S. might not be available elsewhere—or vice versa. Medical tourists often don’t realize that pills bought overseas might not have gone through any real safety checks.
Understanding FDA approval helps you ask better questions. If your doctor switches you to a generic, is it safe for your condition? If you’re on a high-risk drug, did it get special scrutiny? When you see an orphan drug with a $500,000 price tag, you’ll know why—it got seven years of market exclusivity to offset the tiny patient pool. And if you’re using an OTC sunscreen or sleep aid, you should know: even over-the-counter products need FDA approval to make health claims. The system isn’t perfect, but it’s the best shield we have between you and dangerous, untested, or mislabeled meds. Below, you’ll find real-world stories of how this approval process affects your health—from drug interactions that slip through cracks to the hidden risks of switching generics in kids or older adults. These aren’t abstract rules. They’re the reason some pills save lives and others nearly end them.